Session 3: Hypoxia Flashcards
(21 cards)
Describe the steps in the transport of oxygen from the atmosphere to the tissues of the body
Each step in the chain of supply can be affected by disease, but the ultimate consequence of any such condition is that some or all parts of the body receive less oxygen than they need – hypoxia, which is sometimes also associated with inappropriate accumulation of carbon dioxide.

What is meant by Hypoxia?
Hypoxia is oxygen deficiency at tissue level.
- All tissues need to be supplied with oxygen at the rate they are using it, either immediately (brain, heart – so deficient needs to be corrected very quickly) or on average over minutes or hours (skin, gut etc)
- If this need is not met, they will become hypoxic, and undergo necrosis, be damaged or die.
The supply of oxygen to each individual tissue depends first on appropriate oxygen content in arterial blood, and second on adequate local perfusion.
Appropriate oxygen content in arterial blood depends on effective diffusion of oxygen from alveoli into the alveoli capillaries, and appropriate partial pressures of oxygen in the alveolar gas.
Appropriate pO2 in alveolar gas depends upon adequate ventilation of the alveoli, which itself depends upon the ease of air flow through the airways, the capacity of breathing movements to generate appropriate pressure differences and appropriate composition of inspired gas.
Any disease process affecting oxygen supply to tissues must affect one or more of these steps, which therefore provide a convenient classification for pathophysiology, and the ultimate outcome, local or generalised, is hypoxia.
Describe local poor perfusion

Local (regional): as a result of arterial insufficiency or damaged individual tissues may become hypoxic e.g. peripheral vascular disease, ischaemic heart disease, ischaemic stroke. Atheromas in vessels limit blood flow – commonest cause of arterial narrowing. In the legs this produces claudication and other changes such as loss of hair, skin changes and possibly ulceration – but symptoms are more likely to be gradual compared to embolism.. Another example is angina, where the coronary arteries are affected and also neurological deficit is a symptom of stroke. Emboli can also cause poor local perfusion (acute onset of symptoms of ischaemia)

Describe Claudication
Claudication: usually lower limb is affected, not upper
- Pain on exercise (metabolic needs increase, arterial narrowing prevents oxygen supply meeting demands)
- Relieved by rest (progressive – shorter distances bring on pain)
- Examination: weak/absent peripheral pulses, maybe pale in comparison compared to other limb, colder
- Assess by Doppler flow
- Treat by bypass
Atheroma: plaque partially occludes lumen => compromised flow, particularly when demand high
Peripheral cyanosis can occur due to poor perfusion. But you wouldn’t expect central cyanosis – not a generalized problem if the other limb is fine.

What is meant by Cyanosis, and describe the differences between local and global
Cyanosis: purplish discolouration of skin and mucous membranes due to the colour of de-saturated Hb. Present when >50gm/L of de-saturated Hb in blood.
Central Cyanosis:
- Indicates arterial hypoxia but remember hypoxia can occur without cyanosis!
- Seen in tongue and oral mucosa (which are not affected by poor perfusion problems – tongue is normally well perfused and warm).
- Concomitant peripheral cyanosis also present – blood is already hypoxic when leaving the LV.
Peripheral cyanosis:
- Seen in the extremities – fingertips, toes, ear lobes and outer lips (if it is very cold)
- Can occur without central cyanosis
- Peripheral cyanosis on its own is due to poor circulation – poor perfusion e.g. in peripheral vascular disease, cold climate
- Due to increased O2 extraction from sluggish capillary circulation
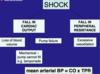
Describe global poor perfusion
global poor perfusion is known as shock. Here arterial blood pressure falls below the level necessary to perfuse all tissues. Baroreceptor responses will exaggerate the reduction in perfusion of some tissues such as the gut and skin in order to maximise that to others such as the brain, heart and kidney. Unless corrected rapidly, the poorly perfused tissues will begin to die, releasing mediators which vasodilate and causes further catastrophic circulatory collapse.

Describe hypovolaemic shock
Hypovolaemic shock (low pre-load)
Common causes include massive blood loss, fluid loss via GI tract (diarrhoea, vomiting), urinary losses (Diabetes Mellitus – diabetic ketoacidosis)
Loss of volume leads to low venous return
Low pre-load
Low cardiac output
Fall in arterial pressure
Mechanisms to replace lost volume include baro-receptor mediated sympathetic reflexes: pale, cold clammy skin, tachycardia
Venoconstriction and auto transfusion (due to Renin-angiotensin-Aldosterone system, ADH)
Describe cardiogenic shock
Cardiogenic shock (pump – heart – is failing)
- Classic cause is myocardial infarction
- Damage to myocardium
- Arterial pressure falls
- Baroreceptors stimulate sympathetic outflow
- Reduced perfusion
- Skin cold, pale and clammy
- Tachycardia
- Kidneys try to conserve volume so you get oliguria. `You also get confusion due to reduced perfusion of the brain.

Describe mechanical shock, and compare the differences between septic and anaphylactic shock
Mechanical shock (something outside of the heart affecting the filling of the heart) e.g. pleural effusion
Septic shock (total peripheral resistance has reduced – massive vasodilation)
- Endotoxin released by bacteria e.g. in pneumonia, pyelonephritis
- Overwhelming vasodilatation
- Dramatic fall in TPR
- Cardiac output cannot keep up to maintain blood pressure
- Warm red peripheries (so not classical signs of shock) as the problem is vasodilation. BUT BP is still low.
Anaphylactic shock (total peripheral resistance has reduced – massive vasodilation)
- Release of histamine from mast cells
- Overwhelming vasodilatation
- Dramatic fall in TPR
- Drop in blood ressure
- Mediators also cause bronchoconstriction and laryngeal oedema (not seen in sepsis) => breathless, wheezing
- Acutely life threatening
- Treat with adrenaline

Describe the consequences of poor perfusion in shock
- Tissue damage
- Poorly perfused tissues
- Initially use anaerobic metabolism
- Lactic acid produced – metabolic acidosis
- Tissues then begin to die
- Release of vasodilator mediators (at a local level initially)
- Circulatory collapse
- Multiple organ failure
How may hypoxia occur due to poor oxygen content in arterial blood?

Hypoxia due to poor oxygen content in arterial blood. This may be due to low pO2 or low oxygen carrying capacity.
Hypoxia due to low oxygen carrying capacity
Oxygen travels bound to haemoglobin so capacity is reduced if there is less haemoglobin – anaemia, or the haemoglobin cannot carry oxygen e.g. as in carbon monoxide poisoning.
Describe Anaemia, including the types and consequences
There may be too little haemoglobin in the blood because
- Insufficient red cells are produced in the marrow (red cell production rate does not match rate of RBC loss)
- Insufficient haemoglobin is synthesised because of:
- A deficiency of some vital component such as iron
- Higher than normal loss of red cells – bleeding or red cell destruction
- Haemoglobin may be present but not functioning if the oxygen binding sites are otherwise occupied e.g. binding CO
Types of Anaemia:
- Deficiency anaemia: iron (including due to chronic blood loss), vitamin B12/Folate. NB: in gastric colorectal cancer who lose small amounts of blood (not noticeable) but iron deficient, people with fibroids etc.
- Problems with bone marrow e.g. leukaemias
- Diseases causing excessive red cell breakdown (e.g. G6PD deficiency causing haemolysis)
- Acute loss of blood (different to chronic blood loss) e.g. massive post-partum blood loss
Consequences of anaemia: poor oxygen supply leads to tiredness, headache and poor exercise tolerance. Classic signs in the mucous membranes, tongue, sclerea, hands.

Describe how hypoxia may be caused by poor oxygenation of blood in lungs

Hypoxia due to low pO2 (low partial pressure of oxygen) in lungs
- May be due to ventilator failure (pump failure – unable to move sufficient air in and out of lungs) or this may be because pO2 is low in alveolar gas, or transfer of oxygen to arterial blood is impaired.
- Impaired transport of oxygen to arterial blood may be due to unusual barriers to diffusion or inappropriate patterns of blood flow through the pulmonary capillaries (poor ventilation perfusion matching).

How would you measure oxygen saturation? And differentiate between Types 1 and 2 Respiratory Failure
When pO2 in blood is <8kPa, this is respiratory failure
- Type 1: only hypoxia; pCO2 is normal or even low
- Type 2: hypoxia is associated with CO2 retention
Measuring poor oxygenation:
- Oxygen saturation: oxygen saturation of haemoglobin in arterial blood (SaO2) can be measured by a pulse oximeter. SaO2 is usually >95%.
- Arterial blood gas analysis: arterial blood sample obtained by arterial stab (usually radial artery). The sample is put through a blood gas analyser – estimates pO2, pCO2 and pH of arterial blood. Make sure ulnar artery is functioning though (use Allen’s test) before to prevent perfusion problems to the hand.
Describe Ventilatory Pump Failure

Respiratory Pump failure:
Not enough oxygen enters the alveoli
Not enough CO2 leaves
pO2 low, pCO2 high – Type 2 respiratory failure
If the pCO2 high, it usually means air is not being moved in or out sufficiently
Important to identify because usually need artificial ventilation
Risk of respiratory acidosis
Example of causes include myasthenia gravis but can be split to:
Poor respiratory effort: respiratory centre depression (e.g. narcotics), muscle weakness (upper motor neurone lesion, lower motor neurone lesion) e.g. trauma, severe stroke affecting the brainstem, something affecting the diaphragms
- Chest wall problems: scoliosis/kyphosis, trauma (flail chest), pneumothorax
- Stiff lungs: severe fibrosis (end stage)
- Hard to ventilate lungs: high airway resistance, COPD (late stages), asthma (severe)
Describe Poor Ventilation Perfusion Matching

Occurs in disorders where some alveoli are being poorly ventilated OR some alveoli are being poorly perfused. O2 uptake is affected more than CO2, which is easily removed by hyperventilation (therefore CO2 removal unaffected). It is Type 1 respiratory failure.
If too much blood flows through a pulmonary capillary for the ventilation of its alveolus, the pO2 will fall. This cannot be compensated by extra oxygen uptake by blood at better ventilated alveoli as that blood is already saturated.
Many conditions can lead to poor ventilation perfusion matching, including pulmonary emboli, pneumonia and consolidation, other changes in the pulmonary circulation or inadequate ventilation of some parts of the lungs (collapse of a lobe, large airway destruction).
A pulmonary embolism leads to some alveoli being poorly perfused. Blood is redirected to other parts of the lung – ventilation of affected parts is wasted. Excess perfusion in rest of the lung not matched by available ventilation (V/increased Q)
Poor ventilation of some alveoli can be due to pneumonia, acute asthma and RDS of newborn. Poor O2 uptake in these alveoli cannot be compensated by increased uptake in others. But increased CO2 removal by rest of lung prevents hypercapnia.
Describe Unusual Barrier to Diffusion

Unusual Barrier to Diffusion (=> poor diffusion across alveolar membrane)
The barrier to diffusion between alveolar air and pulmonary capillary blood is normally very slight, though oxygen diffuses much less readily than carbon dioxide, and so it is always affected more by any change. The barrier may be increased if it gets longer, or the structure changes. This normally type 1 Respiratory Failure.
Structural Changes: fibrosis of the lung in such conditions as silicosis will increase the diffusion barrier. Causes include fibrosing alveolitis, asbestosis, extrinsic allergic alveolitis, pneumoconiosis – all restrictive lung diseases
Reduced surface area for exchange: e.g. emphysema
Increased path length: formation of tissue fluid in the lung will separate the alveolar epithelium from the pulmonary capillary endothelium => pulmonary oedema
- This happens when hydrostatic pressure in the pulmonary capillaries exceeds oncotic pressure.
- Hydrostatic pressure is increased in left heart failure, or following mitral valve regurgitation.
- Oncotic pressure is lowered in malnutrition or liver failure.
- In volume overload the output of the right heart may exceed the maximum output of the left heart and increase pressure in the pulmonary capillaries.

Describe and explain the pathophysiological changes that may lead to poor ventilation of the alveolar spaces
Poor transfer of oxygen from air to alveoli will almost invariably be associated with poor transfer of CO2 from alveoli to air, so pCO2 will rise as well as pO2 falling. This is Type 2 Respiratory Failure.
Poor ventilation may occur because it is difficult to move air through the airways, or difficult to expand the lungs in inspiration.
Difficulty moving air through the airways:
- This is obstructive lung disease – such as asthma or COPD.
- Here small airways are narrowed by inflammation mucus and bronchiolar muscle spasm, leading to problems with expiration as the airways are narrowed further as the patient tries to breathe out.
- This will be revealed by a smaller proportion of air ejected during the first second of a forced expiration – a lower FEV1.0 to FVC ratio, and by changes in the expiratory flow volume curve.
- If the obstruction is due to significant airway reactivity, it will be partially reversed by beta-adrenoreceptor agonist drugs such as salbutamol.
Difficulty expanding the lungs
- This may be because the lungs are stiff, the chest wall is deformed or respiratory muscles are weak.
- Stiff lungs happen in fibrosis, changes in the thorax may be congenital (scoliosis, kyphosis) or acquired (e.g. trauma). Muscle weaknesses may be local or global, and can come about by defects in transmission from nerve to muscle (e.g. myasthenia gravis) in motor nerves (motor neurone disease) or damage (e.g. damage to cervical spine above C4)
Describe Inappropriate Inspired Gas
The whole oxygen transport system might be working, but the gas available to breathe may not have a high enough pO2. This occurs mostly on exposure to high altitude. Acute exposure is very dangerous as ventilation and other changes need time to appear – the process of acclimatisation.
Eventually all aspects of the transport chain are enhanced, more ventilation, better change, more haemoglobin, better perfusion and better unloading of oxygen.
Describe Chronic Hypoxia
E.g. in intermediate stage of fibrotic lung disease, where respiratory failure is Type 1.
Increased oxygen delivery
- Increased erythropoietin => raised Hb (can look a bit of purplish)
- Increased 2,3 DPG
Effects of hypoxia on pulmonary arterioles
- Pulmonary hypertension
- Right heart failure
- Cor pulmonale (heart failure secondary to pulmonary hypertension)
Chronic Type 2 Respiratory Failure (COPD)
Chronic Hypoxia
Chronic CO2 retention
- CSF acidity corrected by choroid plexus
- Central chemoreceptors ‘reset’ to higher CO2 level
- Persisting hypoxia
- Respiratory drive is not driven by hypoxia (via peripheral chemoreceptors



