Session 3 Flashcards
(31 cards)
Describe the mechanical system of the lungs and thorax including what happens in a pneumothorax
- Air is drawn into the lungs by expanding the volume of the thoracic cavity.
- During breathing, work is done to move the lungs and thorax and overcome resistance to allow the flow of air through the airways.
- The space between the lungs (covered by visceral pleura) and thoracic wall (parietal pleura) – the pleural space – is normally filled with a few mls of fluid, forming a pleural seal which holds the visceral outer surface of the lungs to the inner surface (lined with parietal pleura) of the thoracic wall. Therefore, if the volume of the thorax cage changes, the volume of the lungs will also change
- The pleural seal ensures lungs fill the thoracic cavity – the lungs are held at a larger volume by the pleural
- Pneumothorax: if the integrity of the pleural seal is broken, the lungs will tend to collapse. E.g. if air gets in between the two layers of the pleura, fluid surface tension is lost and the lungs collapse.
- The lungs are elastic structures and if removed from the chest cavity, the inward elastic recoil of the lungs causes the lungs to totally collapse
- The chest wall on the other hand recoils outwards when the thoracic cavity is open to the atmosphere e.g. during thoracic surgery.
- In the living respiratory system, since the lungs and chest wall will recoil in opposing directions, it creates a sub-atmospheric (negative) pressure within the pleural cavity.
Describe the resting expiratory level
- In the absence of muscular activity (when the respiratory muscles are relaxed), there is an equilibrium position, when the inward force of the elastic recoil of the lungs is balanced by the outward recoil of the chest wall. This corresponds to the state of the lungs at the end of a normal quiet expiration.
- This equilibrium is known as the resting expiratory level.
Lungs pull in and up
Thoracic cage pulls out
Passive stretch of diaphragm pulls down (diaphragm flattens)
- At the resting expiratory level, all forces are in balance like a set of springs. If disturbed, the mechanical system will spring back to the expiratory level.
- The lung volume that exists at the end of expiration is the functional residual capacity (FRC). At FRC, the elastic forces of lung and chest walls are equal and in opposite direction.
- Breathing in from the equilibrium position involves contraction of the diaphragm and the external intercostal muscles.
- Breathing out involves passive recoil of the lungs in quiet expiration and contraction of the abdominal muscles and the internal intercostal muscles in forced expiration.
- Once these muscle contractions stop, the lungs and thorax will return to the equilibrium position by passive recoil.
What happens during inspiration and quiet expiration? How far does atmospheric air go?
In inspiration as the volume of the thorax increases, so will volume of the lungs (due to the pleural seal).
- During inspiration, the volume of the lungs increases as the volume of the thorax increases due to the pleural seal. The increase in the volume of the lung cause the alveolar pressure to fall below the atmospheric pressure, and air flows into the lungs.
- This causes the alveolar pressure to gradually rise back to atmospheric pressure, when inspiration ceases.
- In quiet expiration, the elastic recoil of the lung results in a decrease of the volume of the thorax and lung.
- The decrease in lung volume causes the pressure in the terminal and respiratory bronchioles to rise above atmospheric pressure so air flows back out again, until the alveolar pressure returns to atmospheric pressure.
- Fresh atmospheric air reaches only as far as the terminal and respiratory bronchioles. Exchange of oxygen and carbon dioxide occurs by diffusion between atmospheric air in the terminal and respiratory bronchioles and alveolar gas. This maintains the normal composition of alveolar gas.
Describe pleural pressures in quiet respiration
- In quiet respiration, pressure in the pleural cavity remains negative (sub-atmospheric) throughout the respiratory cycle
- At the resting expiratory level the pleural pressure is negative (because lungs and chest wall are recoiling in opposite directions).
- During inspiration, as the chest wall expands outwards, the pleural pressure becomes more negative and returns to the original (negative) pressure as the lung returns to the resting expiratory level in quiet expiration.

What muscles are involved in quiet and forced inspiration?
In quiet breathing:
- The diaphragm which is the major muscle (70%) of inspiration moves down (flattens) to increase the VERTICAL dimension. It works against the forces required to stretch the lungs= - i.e. to stretch the elastic tissue of the lung and to stretch the film of fluid lining the alveoli
- The external intercostal muscles move in a bucket-handle movement to increase the ANTERO-POSTERIOR and TRANSVERSE diameters of the thorax.
In forced inspiration (i.e. when ventilation is increased or resistance to respiration is present), accessory muscles of inspiration are used
- Sternocleidomastoid and scalene muscles of the neck
- Serratus anterior
- Pectoralis major
What muscles are used in expiration?
In quiet breathing, expiration is passive due to the elastic recoil of the lungs
In forced expiration, accessory muscles of expiration are used
- Internal intercostal muscles
- Abdominal wall muscles (external & internal oblique muscles and the rectus abdominis muscles)
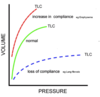
Define the term ‘compliance’ of the lungs and state how, in principle, it is measured
- The stretchiness of the lungs is known as compliance
- Compliance is defined as the volume change per unit pressure change
- High compliance means the lungs are easy to stretch
- Increase in compliance could be caused by something like emphysema whilst loss of compliance could be caused by lung fibrosis
- Compliance is measured by measuring the change in lung volume for a given pressure. The greater the lung volume, the greater the compliance and vice versa.
- However even with the constant elasticity of lung structures, compliance will also depend on the starting volume from which it is measured so it is more usual to calculate Specific Compliance which is: Volume Change Per Unit Pressure Change / Starting Volume of Lungs
Where do the elastic properties of the lungs arise from?
The elastic properties of the lungs arise from two sources: elastic tissues in the lungs and surface tension forces of the fluid lining the alveoli
Explain about surface tension
- Surface Tension: the airways and alveoli of the lungs are lined with a film of fluid which is increased in area as the lungs expand. This increase in area is opposed by surface tension of the lining fluid, because the area of a gas-liquid interface always tends to a minimum.
- The fluid is there because it facilitates diffusion – gases dissolve in fluid and diffuse.
- Surface tension is interactions between molecules at the surface of a liquid, making the surface resist stretching. The higher the surface tension, the harder the lungs are to stretch (lowers compliance)
What is Surfactant?
- The alveolar lining fluid contains a surfactant whose effect is to reduce surface tension forces.
- Surfactant is a complex mixture of phospholipids and proteins, with detergent properties.
- It is produced by Type 2 alveolar cells
- The hydrophilic ends of these molecules lies in the alveolar fluid and the hydrophobic end projects into the alveolar gas.
- As a result they float on the surface of the lining fluid, interspersed between the fluid molecules, disrupting interaction between surface molecules and thereby reducing the surface tension.
What happens to the surfactant when the alveolus expands and shrinks?
- As an alveolus expands, its surface area increases and the surfactant molecules are spread further apart, making them LESS EFFICIENT in reducing the surface tension. Hence as the alveolus expands, the surface tension of the fluid lining it INCREASES.
- As an alveolus shrinks (deflates), the surfactant molecules come closer together increasing their concentration on the surface and act more EFFICIENTLY to reduce the surface tension. Hence, the effect of surfactant is to REDUCE surface tension forces greatly as area of the alveolus decreases.
- The force required to expand small alveoli is therefore LESS than that required to expand large ones – little breaths are easy, big breaths are hard – the effect of surfactant gets smaller as the lungs get bigger.
- This property of Surfactant also serves to stabilize the lungs by preventing small alveoli collapsing into big ones.
What is Hysteresis?
Hysteresis (a physical phenomenon): different amounts of energy is required to move a substance in different directions
- The energy put into stretching a film of surfactant is not all recovered when the film recoils.
- This loss is greatest when tidal volume is maximal; the bigger the area and shape, the more energy is lost (when the lungs recoil) so the less efficient breathing becomes)
- Another reason why little breaths are best

Explain how alveoli are like bubbles?
The alveoli are like an interconnected series of bubbles.
- Bubbles are formed when a film of fluid surround gas
- Film shrinks (reduces surface tension) to compress gas (by Boyle’s law) until eventually there is equilibrium between tension and pressure
- The pressure within a bubble is determined by the Law of Laplace:
P = (2T)/(r) where P = pressure in the alveolus, T = surface tension, r = radius of alveolus
- If T is constant, smaller bubbles with a smaller radius would have higher pressures within it and larger bubbles have low pressure
- Therefore if 2 bubbles are connected by an airway the smaller bubble, which has a higher pressure, will empty into the larger bubble (which has a lower pressure).
- The effect of this would be that the larger bubbles will collet air from the smaller bubbles which would collapse
- Alveoli vary in size, so if the surface tension was constant, the alveoli would collapse to form a few huge air filled spaces (known as bullae). This would drastically reduce the surface area available for gas exchange, because the combined surface area of a few large bulla would be much less than the combined surface area of thousands of small alveoli.
Why couldn’t our lungs exist without surfactant?
In the normal lung, the alveolus expands increasing its radius and the surfactant molecules are spread further apart, making them less efficient, thereby increasing the surface tension.
- As the alveolus expands, both surface area and surface tension increase
- As the alveolus shrinks, both surface area and surface tension decrease
Therefore, different sized alveoli can have the same pressure within them. This stabilizes the lungs by preventing small alveoli collapsing into big ones.
- In the absence of surfactant, our lungs could not exist. Surfactant maintains pressure independent of size so big and little alveoli can co-exist.
What happens when surfactant is absent? Give examples
Lung surfactant is absent from alveoli of a fetus younger than about 25-weeks and is occasionally absent from full term babies, producing ‘Respiratory Distress Syndrome’.
- Babies have too little surfactant so their lungs are very stiff (creating breathing difficulty) and they have only few, large alveoli (the little alveoli has collapsed into the bigger ones so surface area for gas exchange is reduced) so breathing and gas exchange is compromised
- If you know the baby is premature, you can give Mum steroids to stimulate development of lungs (increasing surfactant production) or you can give babies inhaled artificial surfactant if they’re on ventilation
- Respiratory Distress Syndrome can also occur in adults who suffer severe trauma – can be very serious, very difficult to manage.
Summarise Surfactant in three points
- Increases lung compliance by decreasing surface tension
- Stabilises the lungs by preventing small alveoli collapsing into big ones
- Prevents the surface tension in alveoli creating a suction force tending to cause transudation fluid from pulmonary capillaries
Explain about the principles of resistance
- Energy must be expended to force air through the airways (as well as against the elastic nature of the lungs)
- The resistance of an airway to flow is determined by Poiseulles Law when flow is laminar, which is true of most of the airways of the lungs.
- Resistance = (pressure) / (rate of flow) = [8 x viscosity of air x length of tube]/ [π x radius^4]
- Resistance of a single tube increases sharply with falling radius. So an individual alveoli has high resistance because of its small radius. However, the combined resistance of the small airways is normally low because they are connected in PARALLEL over a branching structure where the total resistance to flow in the downstream branches is less than the resistance of the upstream branch. The branching structure means at each branch there is an increase in the number of airways in parallel (increase in number of alternative pathways) so their collective resistance decreases
Where in the tract is most of the resistance to breathing then?
Most of the resistance to breathing therefore resides in the upper respiratory tract, except when the small airways are compressed during forced expiration.
- At normal lung volumes in normal lungs, highest resistance in the trachea and lowest in the small airways so breathing is easy (ease of movement of air gets easier as you go deeper due to the increased number of tubes in parallel)
- When the lung is compressed during forced expiration, small airways (with no cartilage rings) are narrowed (due to Poiselle’s law) so resistance increases dramatically and air is trapped in the alveoli (so it hard to get air out and through the compressed narrow bronchioles). Eventually the resistance gets so high you cannot get air through – this is the residual volume
Resistance to flow through airways is of little significance to total work load of breathing in healthy subjects, though it can often be affected by disease.
At rest, the work of breathing consumes only 0.1% of total oxygen consumption so is efficient.
What happens to the resistance in Obstructive Airway Disease? And when do you need to do more work to breathe?
- Obstructive Airway Disease: if the small airways are narrowed by disease such as asthma or chronic bronchitis, resistance increases much earlier in expiration and breathing out can become very difficult. Can be extremely distressing.
- Work is done against the elastic recoil of lungs and thorax; the greatest part of work done is against more or less equally the elastic properties of lung tissues and surface tension forces in the alveoli.
- Most of the effort is required to stretch the lungs unless diaphragm cannot easily move into abdomen (something is in or around the abdomen limiting the rise of abdominal pressure which must match the decrease in the pressure of the thorax therefore preventing diaphragm from moving up) e.g. pregnancy, obesity (fat is incompressible), corsets (often worn these days to support back). You have to do extra work.
Explain about common lung fnction tests
The effects of respiratory diseases may be examined non-invasively by examination of the airstream at the mouth under various conditions. Such ‘lung function’ tests are often useful in the diagnosis and management of respiratory disease. Tests need to assess
- The mechanical condition of the lungs (e.g. to find out whether they’re abnormally stiff or abnormally stretchy)
- Resistance of the airways
- Diffusion across alveolar membrane (effective gas diffusion)
Lung function may be inferred from measurement of volumes, pressures/ flows and/or composition at the mouth.
Describe Simple Spirometry
- The patient fills their lungs as much as possible from the atmosphere, and breathes out as far and fast as possible through a rapidly responding Spirometer.
- Simple spirometry allows measurement of many lung volumes and capacities. Vital capacity (maximum inspiration to maximum expiration) is particularly significant. Tables can be used to predict the vital capacity of an individual of known age, height and sex.
- Vital capacity may be less than normal because the lungs are not:
- Filled normally in inspiration (affected by compliance of the lungs and force of the inspiratory muscles – the stiffer the lungs, the lower the upper limit)
- Emptied normally in expiration (increasing airway resistance as the lungs are compressed – airways are narrowed for some reason)
- Or both

Describe the measurement of forced vital capacity (FVC) and forced expiratory volume in one second (FEV1.0)
- Spirometry can produce a Vitalograph trace which is a plot of volume expired vs time (seconds – typically 6) after a full inspiration
- Initially rapid rise to a plateau
- Forced Vital Capacity (FVC) is the maximum volume that can be expired from full lungs. Typically 5L in normal adults
- Forced Expiratory Volume in One Second (FEV1.0) is the volume expired in the first second of expiration rom full lungs. It is affected by how quickly air flow slows down so FEV1.0 is low if the airways are narrowed. Normally >70%
- Obstructive and restrictive deficits are distinguished by measuring the Forced Expiratory Volume in one second (FEV1.0). In normal individuals this is greater than 70% of the Forced Vital Cavity i.e. FEV1/FVC ratio is <70%
Explain obstructive and restrictive patterns of spirometry
- Maximal filling of the lungs is determined by the balance between the maximum inspiratory effort and the force of recoil of the lungs. If the lungs are unusually stiff or inspiratory effect is compromised by muscle weakness, injury or deformity or there is a problem with the chest wall, they start less full so FVC will be reduced but air will come out normall so FEV1.0 will be >70% of FVC. This is known as a restrictive deficit.
- During expiration, particularly when forced, the small airways are compressed (narrowed), increasing flow resistance, eventually to the point where no more air can be driven out of the alveoli. If airways are narrowed, then expiratory flow is compromised much earlier in expiration, producing an ‘obstructive’ deficit (lungs are easy to fill but hard to empty). FEV1.0 will be reduced as air will come out more slowly but FVC will ne relatively normal.
- Restrictive and obstructive deficits may be separated by asking patients to breathe out rapidly from maximal inspiration through a single breath spirometer which plots volume expired against time (a ‘vitalograph’)
- A time-volume plot (graph) is often referred to as a ‘vitalograph’ tracing.
What would you see in a vitalograph showing an obstructive deficit?
FVC is nearly normal
FEV1 is reduced markedly
FEV1/FVC ratio is <70%







