Session 11 Flashcards
(14 cards)
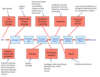
Identify the steps in the oxygen transport pathway from air to tissues
[*] Tissues consume oxygen and produce CO2 at variable rates. The circulatory and respiratory systems must work together to supply and remove gases at an appropriate rate for each tissue of the body. Each step in the chain of supply can be affected by disease, but the ultimate consequence of any such condition is that some or all parts of the body receive less oxygen than they need (hypoxia), sometimes also associated with the inappropriate accumulation of carbon dioxide.
[*] The supply of oxygen to each individual tissue depens on, first, appropriate oxygen content in arterial blood, and second on adequate local perfusion.
[*] Appropriate oxygen content in arterial blood depends on effective diffusion of oxygen from alveoli into the alveoli capillaries, and appropriate partial pressures of oxygen in the alveolar gas.
[*] Appropriate pO2 in alveolar gas depends upon adequate ventilation of the alveoli, which itself depends up on the ease of air flow through the airways, the capacity of breathing movements to generate appropriate pressure differences and appropriate composition of inspired gas.
[*] Any disease process affecting oxygen supply to tissues must affect one or more of these steps, which therefore provide a convenient classification for pathophysiology, and the ultimarte outcomes local or or generalised are poor supply of oxygen – hypoxia.
[*] Respiratory failure is when:
- Not enough oxygen enters the blood
- Not enough CO2 leaves it
- The two can occur together but do not necessarily occur together

Describe how hypoxia can be due to poor perfusion
[*] Hypoxia due to poor perfusion: this may be local or global:
- Local: as a result of arterial insufficiency or damage, individual tissues may become hypoxic. E.g. peripheral arterial disease. Atheroma in vessels limits blood flow – in the legs this produces claudication and other changes such as loss of hair, skin changes, and possible ulceration. Another example is angina, where the coronary arteries are affected.
- Global: global poor perfusion is known as SHOCK. Here arterial blood pressure falls below the level necessary to perfuse all tissues. Baroreceptor responses will exaggerate the reduction in perfusion of some tissues such as the gut and skin in order to maximise that to others such as the brain, heart and kidney. Unless corrected rapidly, the poory perfused tissues will begin to die, releasing mediators which vasodilate and causes further catastrophic circulatory collapse.

Describe how hypoxia can be due to poor oxygen content in arterial blood
[*] Hypoxia due to poor oxygen content in arterial blood:
- This may be due to low pO2 or low oxygen carrying capacity
- Low Oxygen Carrying Capacity: oxygen travels bound to haemoglobin; therefore capacity is reduced if there is less haemoglobin – anaemia – or because the haemoglobin cannot carry oxygen e.g. in CO poisoning. In anaemia, there may be too little Hb in the blood because:
Insufficient red cells are produced in the bone marrow (bone marrow disease)
Insufficient haemoglobin is synthesised e.g. because of a deficiency of some vital component e.g. iron or vitamin B12
Higher than normal loss of red cells – bleeding or red cell destruction.
- Haemoglobin may be present but not functioning if the oxygen binding sites are otherwise occupied, e.g. binding CO.
- Low partial pressure of oxygen: this may because pO2 is low in alveolar gas, or transfer of oxygen to arterial blood is impaired.
- Impaired transport of oxygen to arterial blood: this may be due to unusual barriers to diffusion or inappropriate patterns of blood flow through the pulmonary capillaries (poor ventilation perfusion matching)

Describe Poor Ventilation Perfusion Matching
- If too much blood flows through a pulmonary capillary for the ventilation of its alveolus, the pO2 will fall. This cannot be compensated by extra oxygen uptake by blood at better ventilated alveoli, as that blood is already saturated.
- Many conditions can lead to poor ventilation perfusion matching, including pulmonary emboli, pneumonia (leading to produce of exudate which fills alveoli which means air can’t get in) and consolidation (parts of the lung fill up with fluid, solidifying), other changes in the pulmonary circulation or inadequate ventilation of some part of the lungs (collapse of a lobe, large airway destruction)

Describe what is meant by Unusual Barrier to Diffusion
- The barrier to diffusion between alveolar air and pulmonary capillary blood is normally very slight, though oxygen diffuses much less readily than carbon dioxide and so it is always affected more by any change. The barrier may be increased if it gets longer, or the structure changes.
- Structural changes: fibrosis of the lung in such conditions as silicosis, fibrosing alveolitis, extrinsic allergic alveolitis and pneumoconiosis will increase the diffusion barrier by causing the barrier to thicken. Scar tissue formation further changes the diffusion barrier.
- Increased path length: formation of tissue fluid in the lung will separate the alveolar epithelium from the pulmonary capillary endothelium. This happens when hydrostatic pressure in the pulmonary capillaries exceeds oncotic pressure. Hydrostatic pressure is increased in left heart failure or following mitral valve regurgitation. Oncotic pressure is lowered in malnurition or liver failure. In volume overload, the output of the right heart may exceed the maximum output of the left heart, and increase pressure in the pulmonary capillaries. Pulmonary oedema (fluid in the space between the capillary and alveoli) lengthens diffusion pathway.
Why may Poor Ventilation occur?
may occur because it is difficult to move air through the airways or difficult to expand the lungs in inspiration.

Why may it be difficult to move air through the airways?
Difficulty moving air through the airways (hard to ventilate lungs)
- This is obstructive lung disease – such as late stages of Asthma or COPD (chronic bronchitis). Here small airways are narrowed by inflammation, mucus and bronchiolar muscle spasm, leading to problems with expiration as the airways are narrowed further as the patient tries to breathe out.
- NB: COPD could lead to Type II respiratory failure but could also lead to Type I respiratory failure due to emphysema. The destruction of lung tissue particularly the septa between the alveoli => changes in compliance => ventilation perfusion mismatch => affects oxygen supply => Type 1 failure initially
- This will be revealed by a smaller proportion of air ejected during the first second of a forced expiration – a lower FEV1.0 to FVC ratio, and by changes in the expiratory flow volume curve.
- If the obstruction is due to significan airway reactivity, it will be partially reversed by Beta-adrenoceptor agonist drugs such as salbutamol.

Why may it be difficult to expand the lungs during inspiration?
- This may be because the lungs are stiff, the chest wall is deformed or respiratory muscles are weak.
- Stiff lungs happen in fibrosis, changes in the thorax may be congenital (scoliosis, kyphosis) or acquired (e.g. trauma). Another important chest wall problem could be a Pneumothorax
- Muscle weaknesses may be local or global and can come about by defects in transmission from nerve to muscle (e.g. mysathenia gravis), in motor nerves (motor neurone disease), or damage (e.g. damage to cervical spine above C4)

Describe poor inspired pO2
[*] Inappropriate Inspired Gas: finally, the whole oxygen transport system might be working, but the gas available to breathe may not have a high enough pO2. This occurs mostly on exposure to high altitude. Acute exposure is very dangerous as ventilation and other changes need time to appear – the process of acclimatization. Eventually all aspects of the transport chain are enhanced, more ventilation, better exchange, more haemoglobin, better perfusion and better unloading of oxygen.

What leads to Type I Respiratory Failure?
[*] Problems with the exchange of oxygen between alveolar gas and pulmonary capillary will lead to Type 1 Respiratory Failure
- pO2 will be lowered with no rise in pCO2, which may even fall if the peripheral chemoreceptors stimulate increased ventilation
- Breathlessness (peripheral chemoreceptors detect large fall in O2 and increase respiration rate)
- Exercise intolerance
- Cyanosis (due to insufficient oxygen saturation)
- Some alveoli could be affected by a pulmonary embolism or poor ventilation perfusion matching could occur – poor O2 uptake in some alveoli cannot be compensated by icnreased uptake in others.
What leads to Type II Respiratory Failure?
[*] Problems with poor ventilation of the alveoli lead to the Type 2 Respiratory Failure
- Here, poor transfer of oxygen from air to alveoli will almost invariably be associated with poor transfer of CO2 from alveoli to air, so pCO2 will rise as well as pO2 falling.
- Generally these 2 changes are proportional to each other
- Pump failure
- On occasion, even with poor capacity to ventilate the fall in pO2 will trigger a sufficient increase in ventilation to keep pCO2 normal or low.
- Ineffective respiratory effort – poor respiratory effort, chest wall problems, hard to ventilate lungs
[*] Poor respiratory effort could be caused by
- Respiratory depression e.g. narcotics
- Muscle weakness: upper motor neurone and lower motor neurone (e.g. Motor Neurone disease)
What are the Acute Effects of Respiratory Failure?
- Increased CO2 and decreased O2=> Central Chemoreceptors => Breathlessness (some compensation)
- Acute Hypoxia: when pO2 < 8.0kPa
- Peripheral chemoreceptors also detect large fall in O2 => increased ventilation (breathlessness)
What are the Chronic Effects of Respiratory Failure?
Chronic hypoxia:
- Renal correction of acid base balance
- Increased ventilation (peripheral chemoreceptors detect large fall in pO2)
- Increased oxygen transport capacity (Hb increased, DPG allosterically promotes release of oxygen from Hb at tissues that need it most)
CO2 retention:
- CSF acidic corrected by choroid plexus => pH returns to normal as ratio is restored
- Initial acidosis corrected by the kidney (renal correction of acid base balance) => pH returns to normal as ratio is returned to normal.
- Reduction of respiratory drive. As soon as pH returns to normal, CO2 isn’t driving respiratory drive anymore (as central chemoreceptors have reset to the higher pCO2)
- Persisting hypoxia – this problem is unresolved. Now the hypoxia is driving the respiratory drive (eventually central chemoreceptors stop working as pCO2 increase). The patient is only breathign because of the low pO2 therefore you need to be careful when giving oxygen therapy to these patients, as once the hypoxia has been treated, there is nothing driving the respiratory drive.
Right Heart Failure (Cor pulmonare)
- Effect of hypoxia on pulmonary arteries (they all start to constrict) => Pulmonary hypertension
Chronic Respiratory Failure is severely DISABLING.
Describe the management of Respiratory Failure
- Oxygen therapy
- Removal of secretions
- Assisted ventilation
- Treat acute exacerbations (e.g. with antibiotics)


