Session 1 Flashcards
(51 cards)
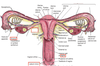
Label


Label

What is the urogenital ridge made of?
Intermediate mesoderm
What does the urogenital ridge give rise to? What does it require and where does it come from?
Embryonic kidney and gonad
Requires primordial germ cells which migrate from yolk sac into cloaca, then to the hindgut through the dorsal mesentery and finally into gonadal ridge

What happens to the mesonephric and paramesonephric ducts in male development? What part of the male DNA allows these changes to occur?
Mesonephric - becomes vas deferens
Paramesonephric - obliterated by production of mullerian inhibiting substance in males
SRY genes on the Y chromosome
What happens to the mesonephric and paramesonephric ducts in females? Why do these changes occur?
Changes occur due to lack of Y chromosome and therefore SRY genes
Mesonephric ducts - obliterated
Paramesonephric ducts:
- not obliterated due to lack of mullerian inhibiting substance
- Grow into abdominal cavity and use together to form uterus
- Forms bicordate uterus if PMD dont fuse
What are the mesonephric and paramesonephric ducts AKA?
Mesonephric - Wolffian duct
Paramesonephric - Mullerian duct
At what week do external genitalia begin to differentiate? What does it consist of at this stage?
At week 7
Consists of genital fold, swelling and tubercle
What happens to the indifferent stage to form the male external genitalia? What substance is required for this to occur?
Genital tubercle elongates and genital folds fuse to form the spongy urethra.
Requires dihydrotestosterone
What happens to the indifferent stage to form the female external genitalia?
No fusion occurs and urethra opens into the opening
Describe the descent of the testis
- Testis begin as a retroperitoneal structure
- Goes through deep inguinal and superficial inguinal ring to enter the scrotum
- Gets pulled by gubernaculum

Describe the descent of the ovaries
Ovary descends to the pelvis, pulled via the gubernaculum that becomes the ovarian ligament proper
Label


What occurs in Turner’s syndrome? When and how is it diagnosed? What is the chromsomal classification?
- 45,XO.
- Results in degeneration of ovaries at 15th week of gestation.
- Diagnosis only occurs post puberty, when a lack of a menstrual cycle and secondary sexual characteristics are revealed.
What are cloacal partitioning defects?
Failure of the cloaca to split into the reproductive/urinary system and digestive system.
What are hypospadias?
- Abnormally placed urinary hole in males and females. Defect of the urethra.
- Can open anywhere on the urethral groove (line which splits penis in 2)
What is a bicornuate uterus?
uterus fails to fuse, resulting in two uteri separated by a septum.
What is the function of GnRH?
Releases LH and FSH from Ant. Pit.
Where is LH and FSH released from?
Ant pit
What is the function of FSH and LH?
FSH - Stimulates maturation of germ cells
LH - Triggers ovulation and development of corpus luteum
What is the function of inhibin and oestrogen?
Inhibin - Inhibits FSH
Oestrogen - Promote and maintains uterus lining
What is the function of hCG and hPL (human placental lactogen)?
HCG - Promotes progesterone release form corpus luteum
hPL - Decreases maternal insulin and glucose utlitisation. Increases lipolysis.
Label


What is the tough fibrous outer layer of the testis called?
Tunica albuginea






