SESAP - Alimentary - UGI Flashcards
Highest RF associated with bleeding peptic ulcer?
- NSAIDS (4.85 fold risk) H. Pylori - 1.79 fold risk
What is this?
Workup?
Treatment?
What is refractory?
Indications for surgery?
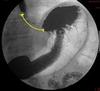
Stricture
Do swallow and EGD. EGD to r/o malignancy.
Management of benign stricture - PPI, Dilation
Balloon dilation - Most require 1-3. > 2 cm = challenging.
Refractory strictures = 14 mm CANNOT be achieved over 5 SESSION at 2 week intervals.
Recurrent = diameter can’t be maintained for 4 weeks.
Dilation balloons - mechanical (Mercury, Tungsten/Maloney) or guidewire polyvinyl bougies (Savary-Gilliard)
Do not increase the dilation diameter by > 3 mm per session.
Fundoplication once GERD and stricture are treated.
esophagectomy if truly refractory or recurrent, maximed medical therapy.
Definition of Barrett’s
- Direct endoscopic visualization of salmon colored mucosa
- pathologic findings of golbet cells in esophagus.
(columnar cells above the GEJ)
Surveillance of Barret’s
NO DYSPLASIA
FIRST YEAR: every 6 months
IF NO DYSPLASIA - every 3 years
Surveillance of Barrett’s
LOW GRADE DYSPLASIA
EVERY 6 MONTHS until NO DYSPLASIA
ANNUALLY
Surveillance of Barrett’s
HIGH GRADE DYSPLASIA
PRE-CANCEROUS
EVERY 3 MONTHS to r/o cancer
Endoscopic mucosal resection
Biopsies at 1 cm intervals (2 cm intervals at 4 quadrant if no dysplasia)
What is endoscopic mucosal resection used for?
- Barrett’s
- T1a esophageal cancer, < 2 cm in length
Esophageal Cancer: Staging
Stage 1 =
Stage 2 =
Stage 3 =
Stage 4 =
T staging review?
N staging review?
Stage 1: NO NODAL DISEASE. T1 a or b
Stage 4: Metastatic anything
extent of nodal disease distinguishes between stage 2 or 3.
N1: 1-2
N2: 3-6
N3:>7
Stage 2: 2A: Larger tumor, no nodes (T2/NO); 2B: smaller tumor/lower nodes (T1/N1or2)
Stage 3: Anything to adventitia and anything with more than 7 LN positives.
T stage:
Ti/1a/1b: in situ, lamina propria/submucosa
T2: muscularis
T3: adventitia
T4: surrounding structures
Stage 1 Esophageal Cancer
What does that mean?
Treatment?
No nodal disease.
T1A - Lamina
T1B - Submucosa
T1A - EMR, Ablative
T1B - surgery first - esosphagectomy
Stage 2 Esophageal Cancer
What does it mean?
Treatment?
Stage 2a:
T2 - muscularis, No nodes
neoadjuvant chemotherapy then surgery
Stage 2b:
T1 - submucosa with 1-2 OR 3-6 LN +
neoadjuvant chemoradiation then surgery
Esophageal Cancer -
Which stages of esophageal cancer are treated with neoadjuvant chemoradiation therapy with surgery?
Stage 2b (2a is without radiation therapy)
Stage 3
Stage IV —> potentially no surgery
Esophagectomy
Name the three types of esophagectomies?
Where are the incisions in them?
Which has the best local/regional control?
Which has the highest morbidity?
- Transhiatal –> Two incisions: Abdomen and neck for a neck anastomosis
- Ivor-Lewis –> Laparotomy and right thoracotomy (or laparoscopically or thoracoscopically) with a chest anastomposis
- THREE HOLE –> three incisions, abdomen, chest, neck
Best local/regional is the three hole because you can sample more lymph nodes and get all the tissue. has the HIGHEST morbidity rates (10-15%). Has the highest leak rate (10%)
THE equivalent to Ivor-Lewis. leak is 3% (55), <5% (5-7%)
THE has the poorest regional control because….you cannot see the entirety of the mediastinum between the neck/abdomen incisions like you can in an Ivor Lewis.
If you have a proximal esophageal cancer - what procedure?
If you have a distal esophageal cancer - what procedure?
Proximal - three hole or THE
Distal - IL > THE
Diagnostic numbers for the esophagus
- GERD - Demeester , Impedence episodes
- Achalasia - LES high pressure, resting pressure.
Demeester > 14.7, Impedance > 47 episodes
LES pressure high > 24, resting pressure > 5
Workup of esophageal Cancer?
Workup of Achalasia?
- Swallow, EGD w/ biopsy, EUS, PET-CT
- Swallow, Manometry, EGD w/ biopsy (rule out stricture/distal mass)
Etiology of dumping syndrome
Early?
Late?
Early - Hyperosmotic load –> just immediately going within 30 minutes of eating to duodenum.
Late - hypoglycemia from insulin release –> 2-3 hours after eating in the duodenum from the food load.
Gastrin
most potent stimulator?
what cells?
where in the stomach?
amino acids/peptides
g-cells
antrum
MC complication after heller myotomy?
key steps of heller?
Reflux
incision through muscular layer 2 cm on stomach, 7 cm on esophagus. Partial fundoplication to prevent reflex (typically an anterior dor…but can do a toupet)
MALT-oma
- What causative organism?
- CD-markers?
- Diagnosis?
- Treatment?
- H. pylori + check t 11/18 translocation
- CD-19, CD-20, CD-22.
- Bx –> see lymphocytic infiltration
- If H. pylori +, t 11/18 - –> quadruple therapy. If H. pylori +, t 11/18 + –> quadruple therapy + radiation + rituximab
output from
stomach?
pancreas?
biliary system?
small bowel?
stomach/mouth - 1500
pancreas - 1000
biliary - 1000
small bowel - 2000


