SAS/Review Flashcards
What is the most important consideratio when interpreting a positive IgM for pertussis?
(Ex: What could cause an inaccurate test result?)
If the patient was recently immunized with acellular pertussis vaccine, they may have a positive IgM test result without actually having the illness
If an infant has a pertussis infection, what laboratory findings would you expect to find 4 weeks after the start of symptoms
IgM: (positive or negative)
IgG: (positive or negative)
4 weeks after the start of symptoms…
IgM = positive
IgG = positive
IgM is present at the beginning of a new infection. 4 weeks is long enough for class switching to have occured to produce IgG as well
Bacteria X has a very short incubation period.
Assuming serology and PCR can both detect the presence of Bacteria X, which test will provide results soonest after the onset of symptoms?
PCR (from sputum or pus sample)
Serology studies examine antibody production, so the immune response must be fully functional for results to be accurate
Which T-cell subset is most important in driving the increased production of IgG and IgA antibodies in response to a pertussis infection?
CD4+ Th2 Helper T-cells
Your body has lots of IgA floating around in it right now
Compare the affinity of IgA for B. pertussis produced by a plasma cell after infection with the affinity of IgM on a naive B-cell before infection
Explain.
The IgA produced by the plasma cells after a B. pertussis infection is most likely has a higher affinity than the original IgM produced by a naive B cell
The original IgM has some affinity for B. pertussis.
Upon infection, Th2 CD4+ helper T-cells are activated by APCs (Bind antigen on MHC II, CD40:CD40L interaction) to form a germinal center and release cytokines
- This promotes both class switching from IgM -> IgA and somatic hypermutation
- Somatic hypermutation and selection by folicular dendritic cells will select for the IgA antibodies with the highest affinity for B. pertussis antigen
What is the principle reason to treat B. pertussis with antibiotics?
To limit the risk of secondary spread
Antibiotic treatment does not greatly affect the course of the disease for the infected individual
Compare the locations of primary and reactivation tuberculosis
Primary typically takes hold in the mid/lower lobe
Reactivation TB typically occurs in the apex of the lung
Which test for tuberculosis will tell you if an individual has a latent infection?
a) Tuberculin skin test
b) Interferon-gamma release assay
c) Nucleic acid amplification
d) Solid media
e) Liquid broth
a) Tuberculin skin test - But may cross react if the patient had any mycoplasm infection or the BCG vaccine
b) Interferon-gamma release assay
c) Nucleic acid amplification
d) Solid media
e) Liquid broth
Both answers in bold are correct
Which test for tuberculosis will most rapidly confirm a diagnosis of an active TB infection?
a) Tuberculin skin test
b) Interferon-gamma release assay
c) Nucleic acid amplification
d) Solid media
e) Liquid broth
- a) Tuberculin skin test
- 48-72 hours
- Will tell you if exposed not necessarily if infection is active
- b) Interferon-gamma release assay
- 24-48h
- Indicates immune response, but not necessarily active infection
- **c) Nucleic acid amplification
- Results in 1-2 hours**
- d) Solid media
- Weeks
- e) Liquid broth
- Weeks
Which cells are most critical in controlling the growth of M. tuberculosis?
CD4+ Th1 Helper T-cells
(Combat intracellular pathogens; in the case of MTB, they mediate the granulomatous response)
A patient who does not have an active infection are concerned about possible exposure to M. tuberculosis.
Which test is recommended? When?
- Interferon gamma release assay two months after last suspected contact
- Testing sooner may give a false negative
- Tuberculin skin test
- False positive is more likely (test has low specificity)
A 5 year-old boy presents with a fever, knee pain, and this rash
Which encapsulated, gram-negative diplococcus is the likely cause of this infection?

Neisseria meningitidis
Which test tube represents the growth of E. coli**?

Test tube 3
E. coli is an facultative aerobe; it can grow near the top of the liquid near the oxygen, but it can also survive without it and grow everywhere
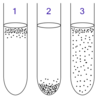
Which test tube represents the growth of Neisseria meningitidis?

Test tube 1
Neisseria meningitidis is an obligate aerobe; will need oxygen, which is located near the surface of the liquid

Increased susceptibility to Neisseria is asosciated with deficiencies in which components of the immune system?
Complement proteins from C5-C9; deficiencies of these complement proteins prevent the formation of the membrane-attack complex (MAC) (via the classic pathway) that is required to kill neisseria
Deficiencies in Factor D and properdin, required for the alternate complement pathway, also result in increased risk of Neisserial infections
Infections are likely to be recurrent and invasive
52 year old Hatian immigrant presents with fever, profuse sweating, labile hypertension, tachycardia, and facial spasms. Loud noises cause him to contrort his body in muscle spasms.
What is the likely causative agent of his symptoms?
Clostridium tetani
He has tetanus
A patient who immigrated from the Democratic Republic of the Congo last year presents with a tetanus infection.
Which treatment should be given immediately?
Injection of tetanus immunoglobulin to confer passive immunity to the patient
- Works rapidly (faster than Tdap vaccine)
(Tdap vaccine should be given to prevent subsequent infection)
22 yo presents with sudden onset of bloody diarrhea and abdominal cramps. He treats himself with some ciprofloxacin he has left over from a trip to Mexico. The diarrhea improves but he becomes more ill with cramping in his lower back, bloody urine and severe fatigue. On presentation to the ED, he is found to have anemia, thrombocytopenia and renal failure. What is the cause of his illness?
Shiga-like toxin, produced by enterohemorrhagic E. coli (EHEC)
- Associated with travel to Mexico
A patient presents with blurry vision, trouble swallowing and speaking, and labored breathing.
Which of the following toxins might be causing her symptoms?
A. Staphylococcal enterotoxin
B. Botulinum toxin
C. Tetanus toxin
D. Diphtheria toxin
B. Botulinum toxin
Symptoms are associated with flaccid paralysis
(Would be an even stronger connection if people who had eaten the same poorly canned food all presented together)
Which bacteria secrete Shiga-like toxin?
What is the effect of the toxin?
EHEC - Patients present with bloody diarrhea
Shiga-like toxin binds to globotriaosyceramide (BG3) in kidney and CNS
It inhibits the 60S unit of the bacterial ribosome to inhibit protein synthesis and cause cell death
Which cells in the body does tetanus toxin bind to?
What is the effect?
Tetanus toxin binds to presynaptic inhibitory motor nerve endings (Renshaw cells) to block the release of GABA and glycine (inhibitory neurotransmitters)
The result is constant muscle contraction; lockjaw, muscle spasm
Which cells in the body does botulinum toxin bind to?
What is the effect?
Botulinum toxin binds to presynaptic motor end plates, preventing ACh release
The result is flaccid paralysis (Blurry vision, impaired swallowing/speaking, may lead to difficulty breathing)
Describe the mechanism of action of diphtheria toxin.
What is the effect on patients?
Diphtheria toxin ADP-ribosylates EF-2, inhibiting protein synthesis
This leads to cell necrosis and pseudomembrane formation in the oropharynx, palate, nasopharynx, nose, and larynx; patients will present with sore throat, fever, difficulty swallowing, hoarseness, and rhinorrhea
Most often seen in children or immigrants who were not vaccinated
Which assay would be most useful to evaluate for the presence of HIV antigens and antibodies
Combination ELISA (aka immunoassay); can test for both antigens andtibodies at the same time
Nephelometry can do both, but not at the same time
A patient presents with 3 days of painful rash (shown below) that is isolated on his right buttock and thigh
He is not taking any medications and reports no allergies
What is the most likely cause of this rash?

Varicella Zoster Virus
- Isolated; does not cross midline
- Painful
You are treating a 35 year old patient with shingles.
What illness did this patient likely have as a child?
What is unusual or concerning about this presentation?
The patient likely had chicken pox (Varicella zoster virus) as a child; shingles is a reactivation of VZV
The presentation of shingles in this patient is concerning because they are young; VZV usually re-activates when the patient’s T-cell function is less than optimal, which happens naturally with age.
Because the patient is young, we might suspect a pathology that is suppressing the function of T-cells
Which test would be most useful to determine a patient’s CD4+ T-cell count?
Flow cytometry
Which patients should not recieve vaccines for MMR, smallpox, and chickenpox?
Patients who are immunosuppressed;
These vaccines are all live, attenuated virus vaccines; they are likely to cause illness in anyone who is immunosuppressed
Which rashe is typically only found in patients with advanced HIV/AIDS?
HHV-8 (Kaposi sarcoma)
Which agent is used to treat pneumocystis?
Trimethoprim-sulfamethoxazole
Although pneumocystis is a fungus, it must be treated wtih trimethoprim-sulfamethoxazole; other anti-fungal agents won’t work
What is the only fungus that should be treated with trimethoprim-sulfamethoxazole?
Pneumocystis
What is the rationalle for recommending combination anti-retroviral therapy?
The RNA-directed DNA-polymerase that copies the HIV genome from RNA->DNA is error prone
Mutations arise that demand broader, more comprehensive coverage to kill the different strains of HIV that may arise in a single patient; this prevents resistance to antiretroviral therapy
A new patient in your clinic presents with the following rash. He is a 43 year old male who reports unprotected sexual contact with other men since he became sexually active 20 years ago. He has not seen a doctor in the last 15 years.
What is the most concerning diagnosis for this rash?
How would you confirm your diagnosis?
How would you evaluate progression of the diagnosis?

Kaposi Sarcoma (HHV-8); this is concerning because it typically only appears in patients with advanced HIV/AIDS
Confirm diagnosis with HIV antibody/antigen ELISA
Evaluate progression with T-cell count using flow cytometry
What tissue is this?

Colon
(The cirles are Peyer’s patches?)
What tissue is this?

Thymus
What tissue is this?

Spleen
What tissue is this?

Lymph node
What tissue is this?

Tonsil
Central CD4+ T-cell tolerance occurs in which of the following tissues?

E - the thymus
Central tolerance occurs in thymus through negative selection; T-cells with high affinity for self peptides presented by MHC undergo apoptosis or become TRegs
Rheumatoid arthritis may have a hereditary basis due to the inheritance of MHC class II alleles.
The involvement of MHC class II suggests that ___________ cells are involved in the pathogenesis of rheumatoid arthritis
The involvement of MHC class II suggests that CD4+ helper T-cells cells are involved in the pathogenesis of rheumatoid arthritis
CD4+ helper T-cells recognize antigen on MHC II
Peripheral CD4+ T-cell tolerance occurs in which of the following tissues?

A - Colon
B - Lymph node
C - Tonsil
D - Spleen
Peripheral tolerance occurs in secondary lymphoid tissues; T-cells that react with antigen in the absence of co-stimulation (ex: self antigen) in the peripheral immune tissues become anergic to that specific antigen
A patient taking corticosteroids develops these white patches in her mouth
What organism is causing these patches?

Candida albicans (aka thrush)
Patients with T-cell suppression (due to steriod treatment or HIV) are more susceptible to mucosal candida
Patients with neutrophil defects (chemotherapy, inherited) are more susceptibel to invasive candida
How can environmental stimuli drive loss of peripheral T-cell tolereance?
Environmental stimuli may induce co-stimulatory molecules on APCs when the APC is presenting a self-antigen
This will cause the T-cells to become active against a self-antigen, thus compromising peripheral tolerance
Which statement is true regarding immune tolerance?
A. T regulatory cells mediate antigen-specific tolerance
B. T cells can become self-reactive during somatic hypermutation in the germinal center
C. T cells undergo receptor editing in the thymus
D. B cells are positively selected in the bone marrow
A. T regulatory cells mediate antigen-specific tolerance
(T cells do not undergo somatic hypermutation or receptor editing; B cells only undergo negative selection)
Which cell is a lymphocyte?

A - could be a B-cell or a T-cell
What type of hypersensitivity reaction involves the fomation of immune complexes?
Type III
What is Cell B?

A mast cell or a basophil
(Both are granulated; basophils leave the bone marrow already mature, mast cells mature when they reach their tissue home)
What is Cell C?

A neutrophil
What is the main cell type involved in Type I hypersensitivity?
What are the major antibodies?
Mast cells
IgE
(Type I = immediate/anaphylactic reaction)
What is the main cell type involved in Type II hypersensitivity?
What are the major antibodies?
CD8+ T cells, NK cells, Neutrophils
IgG, IgM (Cellular or matrix antigen; not free-floating)
(Type II = cytotoxic/antibody-mediated)
What is the main cell type involved in Type III hypersensitivity?
What are the major antibodies?
Neutrophils
IgG (soluble antigen)
(Type III = immune complex-mediated)
What is the main cell type involved in Type IV hypersensitivity?
What are the major antibodies?
CD4+ Th1 helper T-cells, macrophages
No antibodies!
(Type IV = delayed-type hypersensitivity)
A patient with an invasive candida infection likley has defects in which immune cells?
Neutrophils
(Defects in T-cells predispose the patient to mucosal candida)
Which component of the immune system is particularly important in fighting fungal infections?
- Th17 CD4+ helper T cells
- Secrete IL-17 -> Promote neutrophilic inflammation
- Respond to extracellular pathogens (like fungus)
- IgA
- Can dimerize and cross epithelium of the gut; fight the organism before it even enters the cells of the body
Which cells express CTLA-4?
What does CTLA-4 do in the body?
TRegs express CTLA-4
B7 on APCs binds CTLA-4
- This blocks costimulation by blocking CD-28 on T-cells from binding to B7
- This dampens the Th2 CD4+ T cell response, thus inhibiting IL-2 secretion
For which clinical diseases would you prescribe CTLA-4?
Why?
Rheumatoid arthritis (or other diseases in which you want to suppress the Th2 CD4+ T cell response)
CTLA-4 binds B7 (CD80/CD86); this prevents the T-cell’s CD28 from binding to B7, blocking the costimulatory signal
This decreases the Th2 T-cell response
A patient has a history of recurrent infections, many of which are pyogenic and/or granulomatous
Notable organisms include serratia marcescens and staph. aureus
Defects in which immune cells are suspected?
Neutrophils;
This pattern is indicative of a failure to kill organisms that have been phagocytosed;
- A defect in NAPDH oxidase would result in persistent, abscess forming infections, especially from catalase (+) organisms
- Catalase breaks down hydrogen peroxide, preventing the formation of hypochlorite ion; an oxidative burst is needed to kill them
What is the clinical presentation of a complement defect?
Infections with encapsulated bacteria
(S. penumoniae, H. influenzae, N. meningitidis)
What is the clinical presentation of a defect in humoral immunity?
Recurrent sepsis, sinopulmonary disease
(S. pneumoniae, S. aureus)
What is the clinical presentation of a defect in T cells?
- Persistent thrush
- Sinopulmonary infections
- Skin or soft tissue infections
- Chronic diarrhea
(Candida albicans, S. aureus, Pneumocystis, Herpes simplex viruses)
What is the clinical presentation of a neutrophil defect?
Abscesses of skin, soft tissue lymph nodes, bone, and liver
(S. aureus, Klebsiella spp)
What pathogens are implicated in chronic granulomatous disease?
Which immune cells might be defective?
Bacteria (LESS BurgerKiNg)
- Listeria
- E. coli
- Staphylococcus aureus
- Serratia marcescens
- Burkholderia cepacia
- Klebsiella
- Nocardia
Fungi (AC)
- Aspergillus fumigatus
- Candida


