Gram Negative Bacteria Flashcards
(79 cards)
What are some of the distinctive characteristics of the Enterobacteriaceae family?
- Gram negative
- Facultative anaerobes
- Form Bacilli and Cocobacilli
- Many are commensals of the human colon that cause disease under certain circumstances
- Most can ferment glucose
- Oxidase (-)
Escherichia coli are… [Gram stain, metabolism, shape distinctive morphology]
Escherichia coli are gram negative, facultative aneroebic bacilli that are typically part of the normal flora of the human colon.
They are catalase (+) and ferment lactose
What is significant about an organism that turns MacConkey agar pink?
The organism ferments lactose
List the determinants of pathogenicity that apply to all E. coli subtypes
- Alpha-hemolysin: Pore-forming
- Aerobactin: Iron siderophore
- Polysaccharide capsulse: Inhibits phagocytosis
- Pili/fimbriae: Forms attachments
What diseases are commonly associated with E. coli infection?
Meningitis
UTI
Septic Shock
Nosocomial infections
Diarrhea (5 types)
How is an E. coli infection diagnosed?
Culturable on routine media
EMB agar: appears metallic green
MacConkey agar: turns the agar pink due to ability to ferment lactose
What are the determinants of pathogenicity of ETEC?
2 toxins that are plasmid encoded and act on gut epithelial cells
- Heat labile (LT): An A-B Toxin, increases cAMP
- Similar to cholera toxin
- Heat stable (ST): Increases cGMP
Describe an ETEC infection
Enterotoxigenic diarrhea
- “traveller’s diarrhea”
- Watery stools
- 24-72 hr incubation period
- Spread through food and water contaminated with human wasta
What are the determinants of pathogenicity of EHEC?
- Type III Secretion Systems
- Injects toxin into host cell
- Shiga-like toxin
- Inhibits 60s unit of the human ribosome
- Fimbriae
- Forms attachment and effacement lesions
Describe an EHEC infection
Enterohemorrhagic diarrhea E. coli
- Bloody diarrhea
- Crampy
- Absent or low-grade fever
- May lead to hemolytic-uremic syndrome (10% of case)
What distinguishes EHEC from other E. coli strains?
- Cannot ferment sorbitol
- Immunoassay for shiga-like toxin in stool
- O157:H7 serotype causes massive outbreaks
How is EHEC infection treated?
Rehydration
(do NOT use antibiotics)
Where is the reservoir for EHEC?
Cattle
Avoid infection by avoiding consumption of raw meat, unpasteurized dairy/juice
Salmonella enterica is a [Gram stain, metabolism, shape distinctive morphology]
- Salmonella enterica* is a gram negative, facultative intracellular, facultative aerobic, bacillus.
- Cannot ferment glucose or lactose
- Motile (has flagella)
- H2S (+)
- Acid labile (usually killed by stomach acid)
Which E. coli determinant of pathogenicity is required to cause meningitis?
K capsule
Commonly causes meningitis in neonates
What is the reservoir for Salmonella enterica serovar typhi?
Gallbladder of human carriers
What is the reservoir for Salmonella enterica serovar enteritidis?
Farm animals/uncooked chicken
Turtles and other reptiles
What is unique about the diarrhea caused by Salmonella enteria serovar enteritidis, as compared to that caused by ETEC or EPEC?
Salmonella enteriditis is a bacteria of developed countries that causes ~15% of food-bourne illness in the USA
ETEC and EPEC are common in developing countries, and are often seen in the US in individals who have traveled to these countries
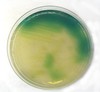
MacConkey agar culture: which enterobacteriaceae organisms might be growing on the left in this picture?

Any lactose fermentor
- E. coli
- Klebsiella
- Enterobacter
How is typhoid fever treated?
Always treat typhoid fever
- Antibiotics
- Fluroquinolone, ampicillin, chloramphenicol
- Note: Resistance is becoming more common
Yersinia pestis is [Gram stain, metabolism, shape, distinctive morphology]
Yersinia pestis is a gram negative, facultatively anaerobic, bacillus.
It is encapsulated and has a bipolar appearance on a gram stain (“closed safety pin)
Where is the environmental reservoir for Yersinia pestis?
What is the vector for human transmission?
Reservoir = rodents (prairie dogs in USA, rats historically)
Vector = fleas
Which Yersinia pestis determinant of pathogenicity allows the bacteria to multiply in large numbers in the human body?
YOPS: The effector proteins secreted by the Type III Secretion system
- YOPS disable macrophages and neutrophils -> inhibits phagocytosis and cytokine produciton
How is Yersinia pestis infection treated?
Choice: Streptomycin or gentamicin
Alternative: Doxycycline or chloraphenicol