Rheumatoid Arthritis Flashcards
What is the hallmark of RA?
Persistent inflammatory Synovitis that usually involves peripheral joints in a symmetrical distribution. This synovitis has a propensity to erode cartilage and bone as well as reduce joint integrity.
T or F: the course of RA is variable and is likely influenced by genetics and environmental factors with some patients experiencing only mild oligoarticular disease with minimal joint damage while other patients have progressive arthritis that can result if not appropriately treated to marked functional impairment.
True.
Is any one ethnic or age group predisposed to RA?
• if so who?
RA is distributed worldwide across all ethnic groups with a peak incidence ranging from the mid 30s to 50s.
What are your chances of getting RA as you get older?
• who gets RA most commonly?
• what is the disease prevalence?
RA is most common in females (30-50) with an increased incidence with age. This disease is about 1/100 in the U.S.
T or F: RA is a disease of increased morbidity, but not increased mortality.
False, RA is associated with increased mortality - the mortality rates are about 2x as high as the general population
Which HLA type has the greatest association with RA?
• is there any increased risk if you are homozygous for this HLA type?
HLA-DRB1 or HLA-DR4 is associated with RA. People who have 2 copies have increased risk of getting the disease and the disease they get is typically more severe.
what is HLA-DR4 and what is the role of HLA-DR4 in the pathogensis of RA?
• 4 important points
HLA-DR4 is an MHC type II protein that binds and presents peptide it is known that HLA-DR4 1binds arthritogenic peptides (like type II collagen epitopes) and presents them to T-cells or it may 2present sequences that mimic arthritogenic peptides. There may also be 3direct interaction between DR4 shared epitope and the T cell receptor. 4Thymus should select against these T-cells, but it doesn’t.
What is the role of genetics and environment on development of RA?
• what environmental factors are important in the pathogenesis of RA?
- Genetic Risk Factor (HLA-DR4) are 60%
2. 40% is environment
***Smoking is a huge environmental risk factor. Its known to induce the formation of a PAD4 (protein-arginine deaminase) enzyme that turns arginine to citrulline (a non-endogenous molecule) this leads to the formation of citrullinated peptides that our immune system recognizes as foreign.
***Gengivits is also known to upregulate PAD4
What is Rheumatoid Factor?
Rheumatoid Factor = antibodies directed aginst the Fc portion of IgG (typically this is IgM but could also be IgG or IgA)
Is Rheumatoid Factor specific to RA?
NOOO, RhF is upregulated in a number of diseases (Sjorgren, Mixed CT, cyroglobulinemia, SLE, Polymyositis, Dermatomyositis).
• Its also present at low levels in the normal population
In what Non-autoimmune disorders is RhF often seen in?
- Chronic Infection - Bacterial Endocarditis
- Hepatitis B/C
- Pulmonary Fibrosis, Sarcoidosis
- Malignancy (B-cell lymphomas)
- Primary Biliary Cirrhosis
What is the most specific antibody you can look for in a patient with RA?
• what is another besides RhF ?
Anti-CCP (cyclic citrullinated peptide) antibodies are the most specific
• ANAs may be seen
Do all people that present with Rheumatoid Arthritis + ANAs have Rheupus?
No, a small portion does, BUT the majority have a milder form of RA
Is there ever evidence of autoimmunity in RA patients before they present with the disease?
Yes, people may have evidence of autoimmunity years before their RA kicks in
T or F: autoanitbodies in RA are specific only to joint antigens
FALSE, they can recognize BOTH joint antigens like type II collagen AND systemic antigens like glucose phosphate isomerase
Note: Antibodies generated in RA may locally activate complement leading to decreased C4, C5, and increased C5a
How does the prognosis for RA differ for people with the seronegative form?
People with seronegative RA tend to experience a more rapid/aggressive disease course and DO NOT respond as well to treatment
What lymphocytes are implicated in the pathogenesis of RA?
• if you biopsied the synovium what cytokines released specifically from these cells would you find and would you find a lot of them?
CD4+ TH1 and TH17 cells are all implicated in the pathogenesis of RA, but if you biopsy the synovium is has relatively little of any of the IFN-gamma or IL-17 secreted from these cells
NOTE: REGULATORY T-cell function that suppresses activation of other T cells may be low in RA synovium
What is the real contribution of T cell to synovial inflammation thought to stem from?
T cell contribution to Synovial inflammation is though to occur through antigen indepedent mechanisms that just involves direct Cell-cell contact with macrophages
If T cell cytokines aren’t high in the synovium, then what cytokines are?
• what are these cytokines?
Macrophage and Fibroblast cytokines are high in the synovium these include:
• IL-1
• TNF-alpha
• IL-6
• IL-15
• IL-18
• GM-CSF
• IL-33
Anti-inflammtory cytokines such ______________ are produced by the __________.
• is production of these enough to hold back inflammation?
Anti-inflammtory cytokines such IL-1Ra and IL-10 are produced by the SYNOVIUM but this NOT ENOUGH to overcome RA inflammation.
What is the number 1 KEY cytokine secreted by macrohpages in RA?
• what does this cytokine do that causes inflammation?
TNF-alpha = key Cytokine => this is secreted by T cells to activate macrophages. Activated Macrophage in turn secrete More TNF-alpha as well as IL-6 and IL-1.
TNF-alpha then acts to increase IL-8, IL-6, and IL-1.
- *• IL-8** works to recruit neutrophils to contribute to inflammation
- *• IL-1** (OAF - osteoclasts activating factor) activates osteoclasts causing OSTEOPENIA in these joints
- *• IL-6** - PGE2 and Fever?

T or F: the pannus actually is partially responsible for eating away the joint capsule.
True, the pannus eats into cartilage
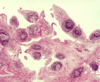
What will you see in joint effusions in an RA patient?
Neutrophils and Mononuclear cells