Repro Path Flashcards
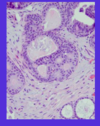
mature cystic terratoma
from somatic totipotentgerm cell
Most common ovarian tumor of reproductive age group
95% of germ cell tumors are mature teratomas
Tumor differentiation towards all three germ cell layers
Skin is the most common tissue seen
46XX
Rarely malignancy may arise in one of the elements of tumor tissue ( in older women)
what age do embryonal tumors peak in children?
befoer age 5 - very rare after that

what would be the expected endometrial biopsy with unopposed estrogen?
proliferative endometrium with breakdown
- You have estrogen without progesterone.
- Eventually you will have breakdown of the EM, because normally proliferative EM is not meant to be there forever.
- It’s meant to be opposed by progesterone, and undergo secretory differentiation.
- If you don’t have the progesterone, then the proliferative EM grows to a certain point and then starts to break down.
- Usually what you see, you have proliferative EM with breakdown.

serous carcinoma
- Large solid and cystic areas
Necrosis and hemorrhage
fibroadenoma vs phyllodes tumors

fixation of cells in cytopathology
- When you’re taking specimens for histopathology, you always use formalin, but formalin is not a good fixative for cells because it bursts the cells- makes them swell and then you can’t interpret them.
- Most samples can go to the laboratory “fresh”, which means with no fixative in it- you can just take the sample and bring it on over to us. If it’s going to be delayed, you can refrigerate it, and cells will last overnight in refrigeration.
- In some cases you have to fix the cells, and the fixative that we use is ethyl alcohol. One of the problems that we always have in the beginning of July is that ethyl alcohol is typically not available on the hospital wards and rubbing alcohol is, so people put rubbing alcohol in their solutions and it bursts the cells.
- In some of our clinics, they will actually teach you how to make the slides, because in some areas the clinician is actually doing the fine needle aspiration. So they’ll teach you how to smear the slides and then let them dry by air or fix them by ethanol.
stage I ovarian carcinoma
Stage I: Limited to one or both ovaries. Five year survival 90%
what is the functional unit of the breast?
the lobule

•The terminal duct and ducules that come out compose the terminal duct lobular unit and that again is where most carcinomas occru
- AT menarchy these ducts proliferate and give rise to some 30 epithelium lined ductules and acini and all those ducules and acini come together to form the lobule
- The breast is divided in to major duct systems that then divide up into lobules
- It’s really lobules that become functional unit of mammary gland
- It’s where you see most of the benign and malignant lesions that occur in the breast.

bartholian gland abcess

- The Bartholin glands can get infected and form abscesses.
- Bartholin glands normally are mucinous glands, with a mucinous lining, but with an infection shown here [bottom right], it can undergo a squamous metaplasia.
- Management is with drainage and antibiotics.
placental abruption
painful third trimester bleeding
premature separation of plaenta after 20 wks, secondary to rupture of maternal vessels
if marginal - vaginal bleeding
if central - retroplacental hematoma (accumulation of blood - uterus hard and painful, no bleeding!)
higher incidence of toxemia and HTN
fetal complications from prematurity
risk inversely related to GA at delivery
respiratory distress syndrome (hyaline membrane disease)
necrotizing enterocolitis
retinopothy
sepsis
neuro issues
proliferative fibrocystic change vs proliferative fibrocystic change with atypia

what day of the cycle is ovulation
day 14
what gene has a bad prognosis for neuroblastoma
N-myc amplification
nonprolif fibrocystic change vs proliferative fibrocystic change of the breast
prolif - 1.5-2x increased risk of cancer

Rh mechanism
- Rh negative woman before pregnancy
- pregnancy occurs, fetus is Rh-positive
- after deliver, Rh alloimmunization occurs in the mother and she dvelops antibodies for Rh
- The next positive with an Rh positive fetus - maternal abs can ross the placenta, enter the fetal blood stream, attach to the Rh-positive red cells causing hemolysis

what is the leading cause of death in infants without birth defects?
prematurity
how do we follow neuroblastoma?
▫Elevated urine metabolites (vanillylmandelic acid [VMA] and homovanillic acid [HVA]). Measuring elevated serum catecholamines is not practical. Typically clinicians measure elevated urine metabolites. Looking at VMA and HVA in terms of whether you have overall catecholamine overexpression. Unlike pheochromocytoma which also produces catecholamines, children with neuroblastoma tend not to present with signs of hypertension. Urine catecholamines are important because they set up a baseline. If a child comes in with high urine catecholamine and then after their tumor is resected they’re still high, it suggests incomplete resection or unknown metastatic disease. If they’re low and subsequently become high several months later, it can suggest recurrence.
if twins and embryo splits at second wk of gestation (late)
monochromatic
monoambiotic
only thing that splits is laminar disk!!

3 components of Wilms Tumor
- Triphasic tumor
- (1) small round blue cell component-primitive blastema; [blue arrow]
- (2) epithelial component-immature tubules (most often) and glomeruli [black arrow]
- (3) mesenchymal stromal component [green arrow]


neuroblastoma
The other aspect that we can see in this tumor, parts of this tumor can have an appearance like this. Rather than having a diffuse round blue cell component, they’ll have Schwannian differentiation. Schwannian differentiation suggests that the tumor has fascicles of eosinophilic spindle cells intermixed with ganglion cells. So these are the ganglion cells that we just talked about (black arrow) and these spindle cells with elongated oval nuclei (blue arrow) and this longer eosinophilic cytoplasm. This is an example of Schwannian stromal differentiation.

proliferative fibrocystic change without atypial
1.5-2x risk
mild dysplasia
- This is the surface layer [the top layer].
- In the normal maturation process, the cells get bigger and their nuclei get smaller as they go to the surface.
- The very early terms used to describe these lesions were mild dysplasia, moderate dysplasia, severe dysplasia and in situ carcinoma.
In mild dysplasia, up to 1/3 of the epithelium shows immature cells – they do not mature and they become atypical. But above that, you get maturation of cells.

serum marker for choriocarcinoma
HCG
Anti-D abs
Rh positive or Rh negative
Rhogam protects against developing abs to D
type II ovarain cancer pathogenesis
Type II pathogenesis starts with p53 mutations in fallopian tube fimbrial epithelium that gives rise to STIC (serous tubal intraepithelial carcinoma). STIC cells are possibly implanted on the ovulation injury site and grow rapidly to present as high stage ovarian cancers.
Possible precursor of type II ovarian cancer is STIC.
II – p53 mutation in fibrae epitheium

Under a microscope, the features of invasion are these cells which have left their boundaries and are starting to grow into surrounding tissue, like here (1).
triple test for breast cancer
- clinical
- radiologic
- pathologic
chorionic villi - 2nd trimester
Smaller
Stroma more cellular
Increased number of blood vessels
Discontinuous layer of cytotrophoblast
Have more CV that can fit in smaller space! Higher SA (surface area)!!! à more absorption (ie: like when u have microvili in small intestine à increased SA = more nutrients for baby
SA increases in CV as CV get smaller and smaller as requirements for baby’s growth increase.

transudate vs exudate
- Transudate is an accumulation of fluid due to increased hydrostatic or osmotic forces, and usually these kind of things happen in a congestive heart failure or pleural fluid in the lungs.
- So you’re looking at this smear [bottom left], you see there’s red blood cells in the background, some lymphocytes [small, solid red balls], and these mesothelial cells. What you’re really trying to notice is that there’s not very many cells, so this is more of a transudate.
- When you look at exudate, you get at an accumulation of fluid usually due to inflammation with increased capillary permeability. That is usually highly cellular.

what 3 breast cancers have best prognosis?
- medullary
- colloid/mucinous
- tubular
treatment of ovarian surface epithelium carcinoma
Surgery: Debulking and Staging
TAH/BSO, pelvic and peritoneal biopsies, omentectomy, para-aortic and pelvic lymph node dissection for staging
Aspiration of ascites, pelvic wash, biopsies from paracolic gutters, surface of diaphragm for staging
Adjuvant Chemotherapy: Combination of a platinum compound (carboplatin/cisplatin) and a taxane (paclitaxel/docetaxel)
pap:

•In contrast, in high grade squamous intra-epithelial lesion, the nuclei are much more enlarged. They almost fill the cells and are much more variable in shape and size. Some are larger and some are smaller.
placental accreta
villi attach to myometrium because no intervening decidua
maternal compliations in preterm labor/PPSOM
infection related to prolonged cervical dilation or ruptured membranes
chorioamniotiis - bacterial
hemorrhage
morbidity from opeation
how do you diagnose if need to give rhogam
determine if fetus is at risk: paternal Rh type/zygosity
fetal testing if father is heterozygous or unknown (amnio > CVS), possible cell free fetal DNA in the future
neuroblastoma stage 4S
It has a special stage called 4S where you have either stage I or II primary tumor but you have evidence of remote disease within the liver, the skin, or the bone marrow. In bone marrow it has to be minimal disease with less than 5% of cell population representing the tumor and there has to be no evidence of concomitant boney destruction. In those cases the prognosis is actually very very good
serous ovarian tumors
Very commonly bilateral - most common and most lethal
- Serous cystadenoma (60%)
- Borderline serous tumor (15%)
- Serous adenocarcinoma (25%)
Low Grade serous adenocarcinoma (Type I cancer)
High grade serous adenocarcinoma (Type II cancer)

what percent of deaths in children from cancer?
11% of deaths
2% of cancers in children
endometrial atrophy
- Atrophy is usually a normal physiologic condition in patients who are postmenopausal.
- It is the most common cause of bleeding in postmenopausal women—not cancer, not EM polyps, not leiomyoma, but simply atrophy.
- It’s worth it to remember that.
- The ovaries basically undergo atrophy, and they stop producing the steroid hormones.
- Therefore, the EM lining becomes very thin, the stroma becomes more fibrotic, the glands are less numerous, and some of them are cysticaly dilated.
- The epithelial lining is simple, meaning one single-cell, and is sometimes dilated.
- That’s normal.
- Something you have atrophy also in young patients.
- In those circumstances, you can see this in patients who are on oral contraceptive pills (OCPs.)
- Another cause, which was more frequent in the past, is when you have young patients with cervical carcinoma, especially the patients who do not undergo normal pap smear testing. [Rambles about how she doesn’t know current guidelines.]
- They can develop cervical cancer, young patients, and sometimes it can be advanced.
- Before you can do any surgery, sometimes you have to treat them with radiation therapy to the pelvis.
- If the ovaries are in the field of the radiation, it also can induce atrophy of the ovary, and then therefore you have atrophy of the EM in younger patients.
- Sometimes you have Premature Ovarian Failure.
- In all these conditions, when the ovaries are not producing those steroid hormones, you would expect to see atrophy in the EM.

surface inclusion cysts
Surface inclucision cysts occur due to ovulation injuries – cytoplasm gets stuck, some cysts undergo metaplasia and give rise to serous or mucinous metaplasia
Because surface injury w more ovulation – more injury is a higher risk
Surface inclusion cysts are formed by invagination of surface epithelium during re-epithelialization of ovulation associated surface injury.
They may undergo mucinous or serous metaplasia.
Most women have inclusion cysts in their ovaries
Women with cancer in one ovary have a higher no. of inclusion cysts in the contralateral ovary compared to women in general population

if twins and embryo splits early (first 4 days) of gestation
dichroionic diamniotic (fused placentae or own placenta)

1.Since there is a tight space; there will be a common membrane from 2 separate amnions/chorions that fuse in center
lymph nodes in cervical carcinoma
pelvic lymph nodes
epithelium?

clear cell type
Secretory type glands with cytoplasmic clearing, clearing because cytoplasm contains a lot of glucogen which is lost during provessing
LN in vulvar carcinoma
inguinal lymph nodes
low risk HPV
6/11
rarely found in cervical carcinoma
breast:

invasive lobular carcinoma
Why is a biopsy dangerous in Wilm’s Tumor?
in a lot of tumors, a child is diagnosed with a tumor, they go in and do a biopsy in order to figure out what it is and then they dictate treatment and then child has a resection. Dangerous to do in WT. If you biopsy WT you automatically upstage the tumor to stage III because it’s considered intratumoral spillage. Intratumoral spillage also occurs if you do an intraoperative frozen section or if the tumor is transected at the time of initial surgery. Problem is that if you penetrate WT it seeds very easily. They assum eif there’s any defect in the capsule whatsoever then there is tumor within in the abdominal cavity and child is treated according to stage III protocol which is much more aggressive.
if twins and embryo splits preimplantation in first wk of gestation
monochorionic
diamniotic
1.If split happens later at stage of blastocyst; when trphoblast has dvlped; tropho will give rise to 1 placental disk + 1 chorion surrounding 2 babies; since amion cav hasn’t dvlpd yet, ea baby will have its own amnion à monochorionic + diamniotic twin gestation

fetal phase
10 wks gestation-birth
pathophys of HPV and cervical cancer
- These are the events after infection. There is a virion which can stay latent in the host for some time or can progress to HPV infection producing these complete virion particles on the surface cells. That would be considered LGSIL [top right figure].
- If the pt can’t get rid of the infection, it will persist. Under the role of some cofactors such as immune response etc., these cells accumulate genetic abnormalities and progress to HGSIL [bottom right figure] and eventually they acquire the ability to invade underlying tissue and become invasive carcinoma [bottom left figure].
- This progression occurs over many years, not weeks or months.

exfoliative cytology
•Urine, CSF
Exfoliative cytology- where the cells just fall off into the fluid that bathes them. So into the urine, the bladder lining cells just fall off and you see them in the urine specimen. In CSF, the same thing; if there’s an abnormality in the lining cells of the meninges, they can fall off into the CSF and you’re looking for that.
stage IV ovarian carcinoma
Stage IV: Distant metastasis. Five year survival 15%

embryonal rhabdomyocarcoma
rare
childhood
“grape” - cross striations
- You get grape-like vesicles, and this is a muscle-like tumor so you get cross striations on those tumor cells.
- This is a child’s reproductive system removed for this rhabdomyosarcoma.
complications of gestational diabetes
spontaneous abortin
congenital malformations (mermaid syndrome, heart disease, neural tube defects)
macrosomia (90th percentile, over 4000 grams) increased delivery compliations
preeclampsia
polyhydraminos
epithelium?

endometrial
Proliferative type glands with columnar cells

fibroma

Benign
Perimenopausal women
Can be mixed with theca cells (fibrothecoma) and produce estrogen
Basal cell nevus syndrome: Bilateral fibrothecomas, basal cell carcinoma, odontogenic cysts of jaw
Meig’s syndrome: Ovarian fibroma with ascites and pleural effusion
Spindly benign cells, less mitotic activity, just remove
Assocaited w ascites – don’t know why
Basal cell nev – bilateral fibroma
chorionic villi in the first trimester
large with double layer of trophoplast (cyto - inner, syncytio - outer)
loose stroma
few blood vessels
CV relatively large ; maternal blood float btwn CV
CV forms a barrier btwn maternal blood + fetal blood that is very thick
CV = large; very little SA

non proliferative fibrosis of cystic change
CYSTS RUPTURE WITH RELEASE OF SECRETORY MATERIAL INTO STROMA WITH RESULTING CHRONIC INFLAMMATION AND FIBROSIS
- This is your normal breast tissue [points to first picture, yellow part]. It should really be fatty and looks more yellow.
- But you see white areas are just fibroconnective tissue.
[reads slide]
•And again here [bottom picture] instead of seeing lots of small acini, the fibrous tissue surrounds these acinar tissues and you get an area of fibrosis

Chronic Endometritis
- Similarly, we have chronic endometritis.
- You have a chronic inflammatory infiltrate within the EM, which is recognized by these cells with this pink Golgi zone, which are basically plasma cells. [Circle is where she felt the cells displayed this clearly.]
- Most commonly, when you see this in the EM nowadays, it’s actually related to the placement of an intrauterine device (IUD).
- When an IUD is present, it’s a foreign body sitting in the EM cavity, and it irritates the EM so you have a response from the immune system, and you have chronic endometritis in some patients.
- The other thing is that when you have retained products of conception, meaning the placental tissue, you can also have chronic endometritis (in addition to acute) if it stays there for a long time.
- Also, as part of Chronic Pelvic Inflammatory Disease, you can have inflammation along the endometrium, along the fallopian tubes, and sometimes can also involve the ovaries.
- You usually remove the offending cause depending on the circumstances.
most common ovarian germ cell tumor?
Germ cell tumors account for 15-20% of ovarian tumors
95% of germ cell tumors are mature cystic teratomas, seen in all age groups
Malignant germ cell tumors are seen mainly in children and young adults (unlike carcinomas which occur mainly in postmenopausal and elderly women)
Malignant germ cell tumors grow rapidly, are usually unilateral, show predilection for lymphatic and hematogenous dissemination
Prognosis in general is good with chemotherapy
serum marker for ovarian carcinoma
CA-125
CA-125 is not a good routine screening tool for ovarian cancer because it may be elevated in benign conditions such as endometriosis and may not be elevated in over one third of patients with ovarian cancer
CA-125 can be used for screening in patients with family history of ovarian cancer
CA-125 is routinely used for measuring the response to chemotherapy or to detect recurrence in ovarian cancer patients
why is toxemia associated with infarcts?
inadequate maternal vessels remodeling
ischemia of the placenta
what is the most common ovarian tumor type?
surface epithelial tumors (70%)
most lethal
liquid based pap smear
- Today we use a liquid based cytology, and the two methods that are out there are just two different companies: thin prep, which is the Cytec company, and autocyte, which is the Surepath company.
- What happens is when you take the smear, you actually stick it into a vial of fixative.
- The benefit of this is you can then use the remainder of the fixative to do the HPV, gonorrhea, and chlamydia testing. The patient doesn’t have to come back or have separate swabs taken; you can do it all off of one vial.
Recently they have said that you can do human papilloma virus testing without the pap smear, so instead of having a pap smear every year for your normal checkup, if your HPV is negative you can go every 3 years and not have a pap. And again, this is all evolving; it’s all relatively new in this last decade
- Once this specimen gets to the laboratory, they spin it and all of these cells fall into this fixative and they spin it down into a preparation that allows you to make a smear.
- So years ago, the traditional smear looked like this [right], and today it looks like this [left].
- I think the advantage of it was that a tech has to screen this whole thing, and the likelihood of missing something is much higher when you have to screen this one by one [right] versus screening a much smaller area [left].
- So the cells not only get concentrated together, these techniques also remove a lot of the mucus and the blood that’s there.

Krukenberg tumor
Krukenberg tumor is a metastatic adenocarcinoma in the ovary with signet ring morphology
15% of carcinomas presenting in the ovary are metastatic
- Breast, GI, Endometrium
Krukenberg tumor shows mucin filled signet ring cells with eccentric nucleus embedded in fibrous stroma
Most common primary source for Krukenberg tumor is stomach cancer (70%).
Colon, appendix and breast are other common primary sites for Krukenberg tumor
Bilateral mucinous ovarian tumors are likely to be metastatic from other site

tubal carcinoma
Primary Tumors: Very rare
Most primary malignancies are serous adenocarcinomas that may present as ovarian masses due to early involvement of Ovary
Metastatic Tumors
Ovary, endometrium, breast, cervix
toxemia of pregnancy
- Toxemia of pregnancy is also related to ischemia of placental disc
- Preeclampsia presents w/ triad of symptoms! (HTN + PROTEINURIA + EDEMA – removed as criteria b/c very common in pregnancy)
- Happens in 6% pregnancies
- usually in mom’s 1st preg during last trimester of pregnancy à important b/c in pts w/ HTN, <22wks preg + HTN, need to think about essential hypertension (not related to pregnancy)
- 20% moms w/ complete moles will present w/ HTN in early pregnancy
- hypertension
- proteinuria
- (edema – common in pregnancy) removed as criterion
- Toxemia associated w/ placental abruption + infarction à easy to understand ischemia
•
•Eclampsia – when mom gets convulsions/seizures
- preeclampsia plus convulsions
fetal complications of Rh
varying degrees of anemia due to alloimmune hemlytic anemia
severity depends on antibody concentration (expressed as iter)
severe anemia –> high output cardiac failure, hydrops fetalis (abnormal accumulation of fluid in 2 or more fetal compartments, including ascites, pleural effusion, pericardial effusion, and skin edema), death
what is the most common cancer in children?
leukemia - 36%
percentage of persistant and high grade dysplasia?
10%
failed placental separation
placental accreta - villi attached to myometrium
(also incretia when penetrate myometrium and percreta when perforate serosa)
due to abnormal adherence of placenta to uterine muscle without intervening decidua
associated with placenta previa uterine scar (c-section)

leiomyomas
- growth of the myometrium
- They grow big sometimes, and they can outgrow their blood supplies. Therefore, you have ischemic changes.
- In this case [top left], you have ischemia; you have leakage of the fluid from the epithelium because it becomes compromised.
- You have cystic degeneration of these leiomyomas. [green arrow]
This is a hysterectomy specimen that is difficult to even recognize.
- This was the cervix [red arrow]
- This was the uterus, the uterine carcass [circle]
- And you have these huge masses that are subserosal [green arrow is one example].
- You can imagine that the symptoms of these patients.
- The uterus is located between the urinary bladder, which is anterior, and the rectum, which is posterior.
- If this mass is sitting right there, it can lead to urinary frequency or constipation.
- They also mimic ovarian masses because they extend laterally.
This whole thing is very painful, and it can interfere with fertility in these patients as well.

HPV integration and cancer
- An additional factor that leads to progression of carcinoma or initiation of dysplasia is integration into host genome.
- Normally E6 and E7 proteins are suppressed by E1 and E2.
- But the integration usually occurs in E1 and E2 area, so there is loss of E1 and E2 function after integration into the host genome. Therefore, there is increased expression of E6 and E7 and are able to bind to more retinoblastoma and p53 to cause further proliferation and other abnormality.

invasive ductal caricnoma of the breast
70-80%
neuroblastoma
- 2nd most common malignancy in childhood
- Median age at diagnosis: 22 months
- Most common site: adrenal gland
- 90% produce catecholamines
▫Elevated serum catecholamines
▫Elevated urine metabolites (vanillylmandelic acid [VMA] and homovanillic acid [HVA])
breast stroma
- Majority of the stroma [points to top figure]
- These are your acini [points to purple holes in LLQ of image]
- They come together to form a lobule
- So here would be a lobule [traces circle of a group of acini that share the same patch of whiteish-purplish tissue] here would be a lobule etc [proceeds to circle more groups of acini. I guess if you go by the patches of white as marking a lobule]
- Here is one of the larger ducts [points to big thing that looks like a broken fork on right side]
- And the lobules then become separated by stroma
- The majority of stroma just consists of dense fibroconnective tissue and mixed with some fatty tissue
- But the lobules are imposed by a hormonally responsive stroma so that when some of the neoplasms occur in the breasts and occur in the stroma, it occurs in this stroma that is responsive to hormones [points to stroma around lobules]

mucinous type ovarian epiltheila tumor derivation
endocervical epithelium
severe dysplasia
•In severe dysplasia, more than 2/3 loss of maturation.

mutation in low grade serous type ovarian tumor
kras
braf
endometrial stromal sarcoma
- Finally, the other sarcoma that you see most frequently is endometrial stromal sarcoma.
- The tumor cells are similar to the endometrial stroma in the proliferative phase of the EM.
- Although it’s a low grade malignancy, it has a pretty high local recurrence rate: about 40%.
- This is with the caveat that you have to follow up with them for a very long time.
- They can recur even after 20 years.
- The patient is not off the hook, even if she has a hysterectomy.
- They have to be followed up for a long time because the tumor can come back in the pelvis, and it’s pretty high at 40% recurrence.
- The good news is that they express estrogen and progesterone receptors.
- Even patients with gland metastasis can respond to hormonal manipulation, like high doses of progesterone.
- They can shrink sometimes, even in the lungs.
The lung metastasis are still really rare; most of the time it’s a local recurrence within the pelvis

endometriod type ovarian epiltheila tumor derivation
endometrial epithelium

condyloma (HPV effect)
chorionic villi - 3rd trimester
smallest CV 0 increased in number
cytotrophoblast not apparent
syncytiotrophoblastic knots
syncytiovascular membranes
Lots of capillary blood vessels located at periophery of CV;
In some areas, the only barrier btwn maternal blood (present in spaces) + fetal blood = syncitial vascular membrane à composed of basement membrane of endothelial cells + a little syncytiotrophoblast
- very thin = very hi/efficient exchange


neuroblastoma
These circles are reminiscent of tubular structures or rosettes. They’re not true rosettes though because they’re not surrounding a definitive lumen. They are instead surrounding a central portion of neuropil. These are called HOMER-WRIGHT psudeorosettes
acute salpingitis
Purulent infection: Neisseria gonorrhae, Chlamydia trachomatis, Mycoplasma, E.coli, H. influenzii, grp A streptococci
Young, sexually active patients, mostly under 25
Ascending route of infection through the cervical canal and endometrial cavity
Cornual resection of fallopian tubes or sterilization reduces the risk of salpingi

- Here is an example of Herpes on a Pap smear: multi-nucleated cells that have a ground glass appearance to the nuclei [black arrow]. They characteristically have this nuclear molding.
- You can say that this woman has a herpetic infection.
- These nuclei actually mold into one another, meaning that they press up against one another – see here it looks like a moon [green arrow] – they are normally round. The nuclei would just be round if they were not molding – like the ones here [red arrows]. But this one forms the [molding] shape [points to the big cluster of nuclei in the middle] and it’s a characteristic feature of Herpes. They mold together and ground glass is when you can see through it – it’s opaque. You can see how this nucleus [black arrow] looks different from this nucleus [red arrow].
what is preterm gestation?
<37 wks
staging of breast cancer
0 - DCIS, LCIS
1 - invasive cancer less than 2 cm with negative nodes and no metastasis
2 - invasive cancer 2-5 cm or involved movable axillary nodes
3 - greater than 5 cm with positive nodes or any size with fixed axillary nodes
4 - distant metastese
lymph nodes in vaginal carcinoma
- Vaginal cancer from the upper half goes to pelvic, and lower half goes to inguinal
- So these are the lymph nodes that the surgeon will take out, depending on the primary site
epithelial hyperplasia of the breast
- This is proliferative epithelial hyperplasia - 1.5-2x increased risk
- The cells are proliferating and you notice that they form slit-like spaces.
- The irregular nature of slit-like spaces that help the pathologist determine between proliferative and atypical hyperplasia
In proliferative the spaces focus more on the outside area rather than the inner area
- And now what you see here [points to bottom picture, left most ductule] are these ductules and how filed they become
- And this is the proliferations of the cells. We’re going to contrast these cells later with atypical epithelial hyperplasia

indirect coombs
diagnosis of alloimmunization
incubate maternal serum with known Rh(D) positive RBCs
RBCs then washed and suspended in serum with anti human globulin
RBCs with maternal anti-RhD will be agglutinated
gestational hypertension
new onset hypertension in pregnancy without other findings after 20 wks gestation
what drug do we give for preterm labor to reduce cerbral palsy
magnesium sulfate
Tunica albuginea ovarii
- Ovary is covered by a single layer of surface epithelium derived from the embryonic ceolomic epithelium
- Surface epithelium sits on a layer of dense connective tissue called Tunica albuginea ovarii

why is toxemia associated with placental abruption?
incrased placental vasoconstrictors and maternal hypertension
damage of maternal vessels

leukoplakia
white patch
finding w dysplasia
mucinous tumors of the ovary
Unilateral, endocervical epithelium
Large in size
Multiloculated
- Mucinous cystadenoma (80-85%)
- Borderline Mucinous tumor (5-10%)
- Mucinous Adenocarcinoma (10%)
what is normal weight at term?
3300 +/- 600 grams
6.5-8 lbs
type I vs type II endometrial carcinoma
•Pathogenetic types –
– Endometrioid Adenocarcinoma (80%)-type I
- Associated with unopposed and prolonged estrogen exposure.
- Obesity, Diabetes, Infertility, Hypertension (positive correlation)
- Low-grade
–Serous Carcinomas – less common, -type II
- Older age group
- High-grade
- Usually it’s a high grade tumor and frequently presents at the highest stage, meaning it has spread more at the time of diagnosis.


mild dysplasia
•showing some enlarged nuclei, some overlapping of nuclei, and some loss of maturation [arrow].

granulosa cell tumor

Juvenile form: before puberty
Secretes Estrogen and inhibin : Precocious puberty, endometrial hyperplasia/carcinoma
Low Malignant: local spread, recurrence and very rare metastasis
Prognosis better in Juvenile form
Call-exener bodies ( arrow) – aborted follicles – lined by oval cells, pink
coffee bean nuclei
serous borderline tumor
cystic with a few solid areas

apocrine metaplasia
of benign breast cysts

- The other change is something that’s call apocrine metaplasia
- If you remember metaplasia – one cell type changing to another
- These cells become apocrine
- Apocrine cells have abundant granular cytoplasm
- Prominent nucleoli
- They are characteristic change in cysts
- Secretory products in cysts can calcify and appear on mammogram
- The fluid can appear brown to blue because it can get hemosiderin in it or you can hemorrhage into it and it changes color
difference between male and female breast cancer?
scant amt of breast tissue - rapidly infiltrates skin and thoracic wall!
male presents at higher stages
types of sex cord stromal tumors
Benign
Thecoma
Fibroma
Malignant
Granulosa cell tumor
Sertoli and Leydig cell tumors

koilocytes

- But here, what we’re looking for is not only the accumulation of this halo, but we are also looking at the nuclei. Recall that the nuclei are usually pretty small, but here, look how large the nuclei are getting [red arrow]. But you still have a lot of cytoplasm. Cells that have larger nuclei, abundant cytoplasm are called low-grade SIL.
- When you get to the higher grades, the nuclei keep getting bigger and the cytoplasm shrinks. So they have a much larger nucleus and a much smaller amount of cytoplasm.
genetic makeup of complete mole
one sperm with nonviable egg or 2 sperm with nonviable egg

No fetus growth! Only get molar chorionic vili
Can have 2 sperm fertilization à if both YY, baby will die (46YY is non-viable)
Can have 2 haploid sperm fertilization empty egg
treatment of benign ovarian surface epithelial tumors
Cystectomy or Unilateral Oophorectomy
what is in normal umbilical cord?
1 vein + 2 arteries

placental infarct
area if ischemic necrosis due to obsruction of blood supply (thrombus in spiral arteries, outside compression)
peripheral or marginal
if small - no clinical significance
if large and centaral - higher mortality! assoc w diabetes, HTN, lupus
•Infarcted area = pale + pink; corresponds to necrotic vili caused by ischemia

proliferative phase
- The proliferative phase is usually the phase that is responsible for the variation in length of the menstrual cycle.
- It can last between 10-20 days.
- It can be different in different women, or even different during the lifetime of the same woman.
- It’s characterized by regeneration of the EM lining after the previous shedding, so therefore you have proliferation of glands and stroma.
- It’s basically regulated by estrogen.
- When you look microscopically at high magnification of the glands, you can easily see mitotic figures [green arrows in top left.] These are the proliferative EM glands.
- You can also see mitoses within the stroma [lower right], quite a few of them.
- Basically this shows you that it’s a regenerating and proliferating.
- You can see more mitotic activity sometimes in normal proliferative EM when you have a low grade cancer.

cryosurgery
for cervical dysplasia
•Cryosurgery is used for low grade lesions. You freeze the lesion and it’ll die off, and hopefully that’ll be the end of that.

immature terratoma from totipotent cell
Rare
Most patients under 20 yrs of age.
Mature and immature elements from three germinal layers.
Immature neural tissue common. Grows rapidly, can rupture in peritoneal cavity or metastasize to lymph nodes, lung, liver. Treatment: Surgery + chemotherapy.
endometrial polyps
- Another condition which is a cause for bleeding from the EM are EM polyps.
- You have the polyp here [giant ball shown by navy arrow]. You have cystically dilated glands. You can see them on low power [green circle although they’re everywhere in the polyp].
- On high power [lower right picture], you normally see the thick-walled blood vessel [square], which you can sometimes see on imaging.
- Later on you will have a lab session, and some of the OB/Gyn colleagues will sometimes see on US the feeding blood vessel into the EM polyps.
- We can have a good idea sometimes on imaging that the patients might have EM polyps in the EM cavity.
- Then you also have a fibrotic stroma [lower middle picture] and this sort of disorderly glands, cystically dilated.
- They are not neatly arranged like you would see in the normal proliferative or secretory phase of EM.

stage II ovarian carcinoma
Stage II: Involvement of pelvic tissues. Five year survival 60%
serous type ovarian epiltheila tumor derivation
fallopian tube epithelium
aspiration cytology
breast, lymph nodes
•Aspiration cytology- taking a thin little needle, sticking it into a lump and bump. We do a lot of this in breast, lymph nodes, and thyroid
moderate dysplasia
•In moderate dysplasia, there is 1/3 to 2/3 loss of maturation.
cells atypical in the bottom

embryonic phase
<10 wks
woman’s lifetime risk of developing ovarian cancer?
1 in 72
Ewing Sarcoma/PNET
- 2nd most common bone cancer in adolescents after osteosarcoma
- M:F 1.3:1
- Rare in Africans and African-Americans
- Typically occurs in diaphysis of long bones, pelvis, ribs
small blue cells - Small round blue cell tumor. Characteristic picture of pediatric tumors. Solid growth pattern. Intervening fibrous septa with a high degree intratumoral vascularization.
non-proliferative fibrocystic change of the breast
alteration present in most women
lumpy bumpy changes on exam
20-40 years of age, peaks premenopause
NO RISK of breast cancer

endometrial carcinosarcoma
- Another condition that is very rare is carcinosarcoma.
- It’s composed of both malignant epithelial and malignant mesenchymal components, as the name indicates: carcino-sarcoma.
- The sarcomatous component in these tumors can look like malignant smooth muscle when it’s homologous.
- Sometimes the malignant sarcomatous component can have differentiation towards cartilage, bone, skeletal muscle, so it’s something that you normally don’t see in the uterus. Therefore, this type is called heterologous.


•Severe dysplasia: more than 2/3 loss of maturation.
host factors for progression of HPV?
- Host factors include smoking, which reduces local immune response in the cervix by loss of dendritic cells.
- Anti-oxidants are helpful in preventing infections of various types.
- During pregnancy, immune response is suppressed, and therefore infection can progress more rapidly.
- Other things that lead to reduced immune status such as HIV infection will also lead to more rapid progression of HPV infection.
- The role of oral contraceptives and other concurrent infection is controversial.

chronic salpingitis
Pyosalpinx: Pus in the lumen, thinning of wall
Hydrosalpinx: Very thinned wall with loss of smooth muscle and plicae, non-ciliated epithelium, no inflammation
Fibrosis – don’t see neutrophils as much
Plicae fuse together and block lumen
choriocarcinoma and mole
preceded by mole in 50%
rapidly invasive, widely metastatic
sheets of malignant cells recapitualiting primitive cyto-syncitiotrophoblast
no villi formation
high hCG
extremely responsive to chemo


neuroblastoma
The other thing to keep in mind with this tumor is that you may have areas with further differentiation. So you have a small round blue cell here (upper red arrow) and adjacent to it you have a much larger cell (black arrow) with an eccentric nucleus, prominent nucleolus and abundant eosinophilic cytoplasm. Right next to that you have a cell that also has a very large nucleus (green arrow) but you can see that it has more cytoplasm compared to this (blue arrow). This is showing maturation toward ganglion cell differentiation. This is another key feature.

cervical adenocarcinoma
clear type ovarian epiltheila tumor derivation
secretory endometrial epithelum

Ovarian counterpart of testicular seminoma - from undifferentiated germ cell
Most common malignant germ cell tumor of ovary
Patients in 20s and 30s
Undifferentiated germ cells
May produce hCG leading to elevated serum hCG levels
Radiosensitive, excellent prognosis
Sheets of germ cells interspersed by fibrotic septa – with some lymphocytes
Malignant, very radiosensitive, very good prognosis
difference between high grade and low grade>
Morphologically the main difference between low grade and high grade serous carcinoma is the degree of nuclear atypia ( mild in low grade, severe in high grade)
Low grade serous carcinoma is often seen in association with borderline serous tumors, shows KRAS and BRAF mutations and is relatively chemoresistant
High grade serous carcinoma is often seen in association with fallopian tube STIC lesions, shows p53 mutation and is relatively chemosensitive
High – shows ugly pleomorphic nuclei w mitotic figures
Low – less mitotic

comedocarcinoma of the breast
high grade malignant cells with central necrosis
necrosis calficies and is noted


lymphoma
- The important thing about cytology is you can use immunohistochemistry to help you define what it is. Immunohistochemistry is another stain that we use – we have a bunch of immunohistochemical markers that are helpful. This is for leukocyte common antigen [bottom right image] – see all the cells that are stained brown. That helps you to say it is lymphoid.
- We can do the smears in conjunction with a bunch of stains to help us determine what the tumor is.
- This is important b/c if this were a metastatic lesion from somewhere else you would want to know from where. Lymphomas are very differently treated than carcinomas.

Botryoid rhabdomyosarcoma occurs along the mucosal membrane of hollow organs (bladder, vagina, nasal cavity). This histologic appearance is classic. One you should remember and know.
You have your squamous mucosal surface (black arrow). Squamous mucosa lines vaginal canal. Immediately under that you have condensed hypercellular layer of cells. This layer of cells is an undifferentiated small round blue cell proliferation called the cambium layer. Supposed to be reminiscent of the cambium layer from which tree roots start to grow. So very condensed cell layer of cell growth. Underneath that you have this very pauci(?) cellular loose mixoid type of tumor growth. Botryoid rhabdomyosarcoma has an extraordinarily good prognosis.

cervical intraepithelial neoplasia categorization
- everything under that category can invade.
- Grade 1 has a lower chance of invasion than grade 3. Grades 1-3 correspond to mild, moderate and severe dysplasia.
- The most recent terminology is in cytology which classifies HPV infections and mild dysplasia as low grade and moderate and severe dysplasia as high grade squamous intraepithelial lesion.
- If you have low grade SIL, the pt can be managed conservatively. If you have high grade SIL, the management is more aggressive, with cone biopsy for the most part.

pap smear
- You use a spatula or brush to scrape the cervix in the area where squamous epithelium joins columnar epithelium.
- This is the body of the uterus [1] and this is the vaginal opening [2].

preeclampsia
new onset of hypertension AND proteinuira OR end-organ dysfunction, occuring after 20 wks of gestation in a previously normotensive woman
multisystem, progressive
ranges from mild-severe
progression may be gradual or rapid
Rhogam
16% of Rh negative wmen become sensitized after 2 deliveries of Rh positive infants
give postpartum anti-D immunoglobulin - reduces risk to 2%
give postpartum and antepartum - reduces risk to .1%
pooled plasma source - derived from hman plasma
give at 28wks if fetus is Rh [ositive
fibroadenoma of the breast
benign

- Has two components – fibrous = stroma,
- adenoma = glandular
This is characteristic look of fibroadenoma – longer than it is wide
- Why is that important?
- Things that are benign spread along the fascial plane and why this extends side to side and not up and down
- Cancers in the breast go through the fascial planes.
When I show you cancer, they are characteristically wider than they are long
- This contrasts to the cyst which looked all black because this is made up of fibrous and glandular tissue. This will have speckled normal-looking breast tissue within here.
- If you trace it along edges, it looks well-circumscribed.
how to differentiate bleeding from placental previa and plancental abruption?
placental abruption is painful bleeding, placenta previa is painless
pathogenesis of preeclampsia
not entirely understood but both maternal and placental
maternal vascular insufficiency, increase placental mass without correspondingly increasing placental blood flow (increase prevalence at high altitudes)
abnormal placental development (impaired trophoblast differentiation and invasion, abnormal remodeling of the spiral arteries)
immuno factors (exposure to paternal/fetal antigens appears to be protective)
increased sensitivity to angiotensin II
schiller test
•, the application of iodine to the squamous epithelium, which normally contains glycogen and is a brown color, but with dysplasia there’s a loss of glycogen and those areas look white. So you can biopsy those areas if you don’t see anything that you can see with your eyes. You can use vinegar and it’ll do the same thing.
mutation in mucinous type ovarian tumor
kras
most important prognostic factor in breast cancer?
lymph node metastasis

borderline mucinous tumor
Epithelial stratification
Mild nuclear atypia
NO stromal invasion
finger like layers lined w mult layers

mucinous cystadenoma
Complicated epithelial architecture: cribriform/solid patterns
Nuclear atypia
Stromal Invasion
Differential diagnosis for mucinous ovarian tumors should always include metastatic mucinous tumors from gastrointestinal tract. Appendix and colon are the most common primary sites for metastatic mucinous tumor in ovary.
glands back to back, stroma has been infiltrated
choriocarcinoma
Choriocarcinoma differentiates towards extraembryonic tissue (placental). It secretes beta hCG. Responsive to chemotherapy
totipotent - diff toward placental


psammoma bodies
serous carcinoma
pathogenesis of wilm’s tumor
Malignant neoplasm derived from nephrogenic blastema
If you were to look at fetal kidney up until the 37th week of gestation immediately under the capsule is your nephrogenic (? Cant understand what she says) which shows the primitive cells that lead to nephrogenesis and these cells are the origin of the Wilms tumor. The Wilms Tumor histology tries to recapitulate normal nephrogenesis.
placenta previa
low lying placenta
marginal, partial, complete
painless 3rd trimester bleeding
associated w placenta accreta (inability to do labor at the end)
- When the placenta is so low (in placenta previa), it can cover internal cervical oss partially/completely; requires C section for delivery of baby
- Pt had placenta previa associated w/ placenta accreta (very thin decidua); if u have placenta previa, u have higher risk of also having placenta acretaà this pt had both accreta + previa à caused massive hemorrhage
pap:

•] Shown here is the effect of the HPV infection: the nuclei get larger; the cells acquire a perinuclear clearing – this empty space around the nuclei known as koilocytic change. These are all changes of HPV infection, also in cytology they are called part of low grade squamous intra-epithelial lesion.
in situ ductal carcinoma of the breast
15-30% of breast cancer - helped by mammography
cannot invatde through BM of ducts –> can’t metastasize!
can spread through the ductal system and involve large segments!!

polycystic ovary disease
LEFT: Have thick, pearly capsule outside because ovulation has not been occurring so the capsule is very thick.
RIGHT: In the superficial cortex there are multiple cysts with a thin wall and prominent theca cell layers.

•The Pap smear shows cells with very hyperchromatic nuclei [bottom left image]. Much larger nuclei. Also see the orange cytoplasm typical of squamous cell carcinoma. Once you see this, you know what the pt has.
Squamous cell carcinomas are also spindled – see the shapes of the nuclei here, the oval spindled cells [red oval]. This is a keratinizing squamous cell carcinoma
atypical ductal hyperplasia of the breast
4-5x risk
architectural and cytological atypia - more rounded spaces and monomorphism of cells
cells fail to entirely fill the lumen
usually assciated w calcification
- The spaces, rather than irregular, become more uniform and rounded.
- Even cells themselves, start to become larger and more pleimorphic.
- Differences in size and shape – although there is some monotony and start to look very similar to one another
[reads second point]
- meaning there are still these spaces but again within these spaces can have calcification because there is proteinaceous material
- Lead to calcifications on mammogram that may be subject to biopsy
why is plaenta previa more frequently associated with placental accreta?
deficiency of decidua
Acute Endometritis
- Acute endometritis is uncommon.
- It can cause discharge from the vagina, infertility, and uterine tenderness, like any inflammation.
- In some patients it can be asymptomatic.
- Most of the time it’s related to retained placental tissue.
- This is composed of chorionic villi.
- It can be either post-abortion or post-partum after normal delivery when some of the placental tissue was left behind and can lead to infection.
- Usually when you have an infection, it’s polymicrobrial and caused by an ascending infection from the normal flora of the vagina.
- The treatment would be, if you have retained tissue, to remove it.
- If you have an infection of bacterial origin, you would treat it with antibiotics.
partial hydatidiform mole
mix of edematous villi and normal sized villi
In contrast, a partial mole occurs when a haploid egg is fertilized by two sperm or by one sperm which reduplicates itself yielding the genotypes of 69,XXY (triploid) or 92,XXXY (tetraploid).[4]
Irregular villous outline (trophoblastic inclusions)
Fetal parts à can have development of an abnml baby
Persistent GTD is low, 0.4%-4%
Very rare reported cases of choriocarcinoma; can become cancerous

type II ovarian cancer
Type II ovarian cancers are rapidly growing and present at stage III or IV. Histologically they are not seen associated with possible precursors such as an adenoma or borderline ovarian tumor. They show p53 mutations. Most patients with BRCA mutations get type II ovarian cancer.
High grade serous, High grade endometrioid and undifferentiated carcinoma are type II ovarian cancers
High grade Serous
High grade Endometrioid
MMMT ( carcinosarcoma)
Undifferentiated carcinoma
Most type II ovarian tumors are supposed to be arising in the fimbrial end of fallopian tube as a result of p53 mutation occurring in the fimbrial epithelium.
pap smear shows LGSIL?
- If the Pap smear shows a LGSIL, these women are tested for HPV.
- If high risk HPV is detected, these pt undergo colposcopy and biopsy.
- If the high risk HPV is negative, these pt are followed with Pap smears.
how do we differentiate neuroblastoma?
In order to define a neuroblastoma you have to have a shwannian core tumor. The area that I showed you before, the shwannian stroma, that has to make up less than 50% of the tumor in order to classify it as a neuroblastoma.
. Further going on to indicate whether or not you’re dealing with an undifferentiated, poorly differentiated or a dedifferentiating subtype that’s where the preseence fo those ganglion cells comes into play. A tumor with no ganglion cell
Poorly differentiated subtypes have less than 5% ganglion cell differentiation or evidence of neuropil and maturation. Differentiating subtypes have greater than 5%. So that’s the next stage in terms of whether or not you’re dealing with a favorable or unfavorable prognosis.differentiation and little or no neuropil is called an undifferentiated subtypes.
mechanism of toxemia in pregnancy
•3 key events in toxemia happen
- Decreased maternal perfusion (aka ischemic placenta)
- Placenta makes more vasoconstrictive substances + less vasodilator production à set up for HTN in mom
- Damage from injury of the endothelium à can activate coagulation in maternal blood vessels (aka disseminated intravascular coagulation)
à if happens in kidney, mom gets proteinuria b/c won’t have normal filtration in the kidney
à if happens in CNS, mom gets convulsions
à if happens in liver, get abnml LFTs b/c of necrosis of hepatocytes
•
•Bascially inflammation/abnml remodeling of mom’s blood vessels during 2nd wk of 1st trimester + remodeling of blood vessels present in superficial SM (smooth muscle) layer à won’t perfuse placenta adequatelyà can lead to ischemia
treatment for malignant germ cell tumors
Mature cystic Teratoma: Cystectomy or unilateral oophorectomy
Malignant: Unilateral salpingo-oophorectomy plus chemotherapy
Malignant germ cell tumors are usually treated with unilateral salpingo-oophorectomy and chemotherapy since bilaterality is not very high and most patients are young so preservation of fertility is important.
Most malignant germ cell tumors respond to chemotherapy well and 5 year survival rate is close to 100% even when tumor has spread beyond the ovary.

mucinous cystadenoma

Multilocular
Smooth cyst walls
Lined by a single layer of mucinous epithelium with basally located small nuclei
cysts mutli loculated – no solid in their, thin 1 layer of epithelium, papillary/finger like projeections, all w single layers
organic vs dysfunctional uterine bleeding
dysfunctional: anovulatory (hormonal) is most common cause
excessive estrogen without progesterone
- DUB is generally ascribed to poorly understood derangement in functional effects of hormones on the EM.
- Dx of exclusion after other known causes of abnormal bleeding are ruled out.
- Anovulatory cycle is the most common case of DUB in the reproductive age group.
DUB due to anovulatory cycles typically occurs at menarche and at menopause, but can occur at any time during the reproductive years
change in chorionic villi over pregnancy
become smaller and increase in number to increase surface area with a thin barrier

plasmacytoid
- These large cells are in an arrangement called plasmacytoid- the nuclei shifts all the way to one side of the cell and there’s a lot of cytoplasm.
- That’s a typical arrangement of what happens in a breast cancer.
Plasmacytoid means resembling the cytoplasm of plasma cells; normal plasma cells have their nuclei shifted towards one side.
hormonal influences of breast cancer
sporadic related to hormone exposure
increased exposure to estrogen unopposed by progesterone - may be that estrogens stim growth facotrs!
eclampsia
new onset grand mal seizures in a woman with preeclampsia that cannot be attributed to another cause
may occur during or right after labor - give magnesium sulfate for labor of preeclampsia
Leiomyosarcoma
- malignant sarcoma with a smooth muscle differentiation.
- As pathologic criteria, like any malignancy, you have cellular atypia, necrosis, and high mitotic counts in these tumors.
- Leiomyosarcomas are bad news.
- You have only a 50% five year survival, about 50% recurrence rate, and 78% chance of having distant metastasis, usually to the lungs.
- Sarcomas usually use the veins to metastasize. That’s why you should always check the lungs when you have leiomyosarcoma.
- You don’t have very good chemo for leiomyosarcoma. You don’t have much to offer to these patients.

complete hydatidiform mole
Molar pregnancy is an abnormal form of pregnancy in which a non-viable fertilized egg implants in the uterus and will fail to come to term. A molar pregnancy is a gestational trophoblastic disease[1] which grows into a mass in the uterus that has swollen chorionic villi. These villi grow in clusters that resemble grapes.[2] A molar pregnancy can develop when a fertilized egg does not contain an original maternal nucleus. The products of conception may or may not contain fetal tissue. A complete mole is caused by a single (incidence is about 90%) or two (incidence is about 10%) sperm combining with an egg which has lost its DNA (the sperm then reduplicates forming a “complete” 46 chromosome set) [4] Thegenotype is typically 46,XX (diploid) due to subsequent mitosis of the fertilizing sperm, but can also be 46,XY (diploid).[4] 46,YY (diploid) is not observed.
Associated w/ Trophoblastic proliferation
- No dvlpmt of baby; No fetal parts
- Prognosis
80-90% benign
10% invasive mole
2.5% choriocarcinoma
Mom only needs to be followed + no pregnancy in future b/c not sure if increased HCG is caused by this or by new pregnancy
Small percent of moms w/ complete moles can become choriocarcinoma

Alveolar rhabdomyosarcoma
Tends to occur, in contrast to embryonal and botryoid, in older children so early teens to mid-adolescence. It tends to occur in deep muscles of the extremities as well as axial skeletal and perineum
Alveolar rhabdomyosarcoma is characterized by an alveolar or lepidic pattern of growth. It’s supposed to look like alveolar septa of lung. Have this discohesive component of cells that sort of falls into the middle (black arrow). These tumors will typically have anaplasia, high mitotic activity and may have intratumoral necrosis.

presentation of polycystic ovary disease
Most common complaint is difficulty to conceive, or infertility.
There is a wide presentation of symptoms.
A lot of patients are asymptomatic until they can’t conceive.
A big chunk of patients have symptoms: amenorrhea, acne, hirsuitism, and they come to clinicians for that.
The basic syndrome: characterized by secondary amenorrhea, or irregular menstrual cycles. They may be infertile. Hirsutism, acne.
A lot of patients are obese.
On ultrasound both ovaries will have multiple cortical cysts.

sertoli-leydig cell tumor

Very rare ( 1% of all ovarian tumors)
All ages but common in child bearing years
Low malignant potential/ may metastasize
Resemble embryonic testis
Reinke crystals ( arrow) in Leydig cells
Secretes weak androgens : Virilization with large tumors
Resembles primitive tubules – arrange in tubule shapes
Look like leidig cells
hydrops placenta
common end-stage pway of variable etiology
cardiac failure
tissue hypoxia and edema in the fetus and placenta
ovarian carcinoma
Florid cellular proliferation giving rise to solid areas
Nuclear atypia
High mitotic activity
Areas of necrosis
Stromal infiltration = Metastatic potential
Borderline tumor grows proliferally – solid areas – access to blood vessels in the stroma

secretory phase
- For example, on Day 17, you have a lot of clearing beneath the nucleus in the cells of the EM glands. [Gestures around a gland.]
- These are the subnuclear secretory vacuoles. The whole cell looks like a piano key.
- This is morphologic proof that ovulation took place.
- Later on, these vacuoles are moved into the apical portion of the cytoplasm and secreted into the lumen on Day 19.
- From Day 20 on, the changes within the stroma, rather than the EM glands, are important for dating the EM.
- On Day 22, you see these pale areas all over the place. This is edema fluid, which is accumulating there.
- On Day 22, you have implantation of the fertilized ovum.
- If you don’t have it, then you have these secretory changes [Day 25] which are in the form of decidualized stroma.
- These pink areas that you see between the glands, these are decidualized stroma, and it’s diffuse on Day 25.

epithelum?

serous (fallopian tube derivation)
Cuboidal to columnar cells with central nucleus and cilia
exposure to HPV?
75%

- You can get HPV infections in this area.
- This tends to be a low risk HPV infection that gives you raised lesions- these are called condylomas.
- These are low-risk so they don’t go on to cancer, but they can present a clinical problem.

mosaic vessels
•Mosaic refers to pattern of blood vessels with a mosaic pattern
finding w dysplasia
wat is considered large for gesational age?
>4000 gms
macrosomia
borderline tumor
Proliferation of epithelial lining of inclusion cyst gives rise to some solid areas
Mild nuclear atypia is seen
Can shed epithelial cells from its surface and cause implants on peritoneal surfaces or on other organs
No stromal infiltration
Can not metastasize
Recurs
5 year survival up to 90% even with peritoneal involvement
Death due to non-malignant complications of disease such as bowel obstruction
Benign can start undergoing some proliferation, start forming areas of stratification w mult layers, epithelial tufts can get pushed off and lay if fluid, can be shed into peritoneum
mixed./borderline – not single layer, more prolific growith – has not invaded ovarian stroma yet! Has not accessed blood vessels – no metastatic potential

invasive mole
molar tissue penetrates or perforates myometrium
hCG emains elevated
need to treat with chemo and hysterectomy
lichen sclerosus et atrophicus.
- A lesion that occurs in older women, and for an etiology for which we don’t know, is lichen sclerosus et atrophicus.
- The skin becomes thin, with a patchy white appearance and itchy skin.
- This is a gross appearance [left]
- This is a microscopic picture [right] with a lot of keratin. But the epithelium itself is thin, and then there’s hyalized collagen below that.

what two cancers are associated with endometriosis?
endometriod adenocarcinoma
clear cell carcinoma
Both are seen associated with endometriosis in up to 50% of cases
They resemble the endometrial cancers of same morphology
Squamous morules (arrow) are often seen in endometrioid carcinoma just like in the endometrioid carcinoma of endometrium
Endometriod – looks like in uterus
Clear cell – clear cytoplasm

how is pediatric cancer different from adult cancer?
- Lower incidence
- Different tumor types - Carcinoma is rare!
- Overall better prognosis
- Special predispositions
Chromosomal and genetic syndromes
Congenital immunodeficiency syndromes
•Increased significance of late effects of therapy
what is cut off for Low birth weight
<2500 grams
small for gestational age (<10%ile)
preterm
congenital cytomegalovirus infection
most common hematogenous infection of the fetus
most mothers are asymptomatic
most infants are asymptomatic
risks: primary and recurrent maternal infection

moderate dysplasia
•slightly more than 50% loss of maturation.
what is term gestation?
37-42 wks
pelvic inflammatory disease
PID ( pelvic inflammatory disease ) = chronic salpingitis with involvement of surrounding structures including ovary and parametrium
PID is characterized by exacerbations of acute episodes
IUD usage is associated with Actinomyces infection which is rare otherwise: Risk of infection is related to the length of IUD usage, 85% cases occurring after 3 or more years of IUD usage
management of patient at increased risk of preterm delivery <34 wks
corticosteroids to reduce risk/severity of RDS
abx
tocolysis to delay delivery for 48 hours
what are the 2 layers of trophoblast cells?
inner - cytotrophoblast
outer - syncytiotrophtrophoblast
- We focus on cytotrophobast (white à has fingerlike projections; very proliferative, but no production of substances/hormones)
- Gray cells w/ nuclei = SYNCYTIOTROPHOBLAST (terminally differentiated; circled in blue)
- SYNCITIOTROPHOBLAST MAKES HCG (human chorionic gonadotrophin)
- During second week, embryo + everything formed by conception is embedded in endometrium when the process of implantation is complete
- White = trophoblast à 1’ chorionic vili; composed of trophoblast
adenomyosis
- The uterine smooth muscle wall is markedly thickened because….you see these little red dots? [navy arrow for one example]
- These dots correspond microscopically [right side] to the present of EM glands and stroma within the smooth muscle.
- You can see the two pinks stripes of smooth muscle on either side of the purple stroma and glandular EM tissue in the center.
- When this is present within the smooth muscle wall, they induce smooth muscle hyperplasia.
- Therefore the uterine wall is thickened, but it’s not forming any well-circumscribed masses. It’s a diffuse process.
- Contrast this to slide 41, where you have well-circumscribed masses.
- With adenomyosis, you don’t have these. Just diffuse thickening of the uterine wall.
- It’s a very painful condition, because these EM glands and stroma are present within the smooth muscle, but they slough like they would in the EM cavity without a way to get out.
- This induces a lot of inflammatory response in those areas.
- You have cytokines, which leads to quite a lot of pain.
•

treatment of polycystic ovary disease
TREATMENT: lifestyle changes – lose weight.
Metformin itself can cause ovulation, used to treat the hyperinsulinemia.
If you don’t want to get pregnant – want to regularize menstrual cycle through the use of oral contraceptives.
Androgenic symptoms are treated with anti-androgens.
Patients who want to conceive can be treated with clomiphene.
high risk HPV
HPV 16/18
risk of progression to high grade dysplasia around 20%
type I ovarian cancer pathogenesis
Type I pathogenesis starts with the formation of cortical inclusion cysts that undergo mullerian metaplasia ( serous/mucinous/endometrioid). It follows a stepwise progression from adenoma to carcinoma through borderline tumors. K-ras mutations are most commonly seen in mucinous carcinoma, B-raf in low grade serous carcinoma and PTEN in endometrioid carcinoma of ovary.


brenner tumor
Rare
Benign
Transitional epithelium nests separated by fibrous stroma
Sharp cytoplasmic borders, clear cytoplasm, Nuclear grooves
Borderline and malignant forms (Atypical Proliferative Brenner Tumor and Transitional cell carcinoma) are very rare
brenner – rarely seen, benign, solid/firm, cystic, nests of transitional epithleium
Oval nuclei w grooves

keratin pearls
squamous cell carcinoma of the vulva
•Microscopically, these well differentiated lesions have these keratin pearls (1), a feature of squamous cells in a well-differentiated carcinoma.
These epithelial pearls are invading underlying stroma, so it’s an invasive cancer
breast ductule lining
- The ductules are lined by 2 layers [points to bottom figure]: inner layer of epithelial cells, outer layer of myoepithelial cells
- Things that make something be benign
- Lose these when something becomes malignant
- Ducts are lined by a basement membrane
- What will become important will be tumors that don’t break through the basement membrane and don’t have the ability to spread anymore

TORCHES infection
Tosoplasmosis
Other (parvovirus B19, varicella zoster, listeria)
Rubella
Cytomegalovirus
HErpes virus
Syphilis
A vertically transmitted infection (or mother-to-child transmission) is an infection caused by bacteria, viruses, or in rare cases, parasitestransmitted directly from the mother to an embryo, fetus, or baby during pregnancy or childbirth. It can occur when the mother gets an infection as anintercurrent disease in pregnancy. Nutritional deficiencies may exacerbate the risks of perinatal infection.

mature teratoma - from totipotent cell tending toward somatic
Most common ovarian tumor of reproductive age group
95% of germ cell tumors are mature teratomas
Tumor differentiation towards all three germ cell layers
Skin is the most common tissue seen
46XX
Rarely malignancy may arise in one of the elements of tumor tissue ( in older women)
Squamous carcinoma is the most common type of carcinoma arising in dermoid cyst
Post meiotic reduplication of germ cell
Occasionally can develop metaplasia and ca
common membrane in dichorionic diamniotic twins?
can be monozygotic or dizygotic
opaque
four layers: 2 amnion, 2 chorion (fused)

transitional type ovarian epiltheila tumor derivation
urinary epithelum
endometriosis
- This time, you have the presence of EM glands and stroma but it’s outside of the uterus.
- In adenomyosis, you have EM glands and stroma within the smooth muscle wall of the uterus, which is also abnormal.
- It should be just in the EM cavity.
- In this condition, it’s completely outside.
- It’s also in young patients, usually in the reproductive age group.
It can also lead to infertility and to pain: to pelvic pain and to painful intercourse
epithelum

Columnar cells with basal nuclei and pale blue cytoplasm, mucin vacules, nuclei are small and on basophil
endocervical derivation
cone biopsy
done for high grade dysplasia. So basically, you remove a cone-shaped piece of cervix and I’ll show you how that looks like. Sometimes the cone biopsy margins come out positive with dysplasia.

Gene mutation in Ewing/PNET
11;22 which is the EWS/FLI-1 translocation.
Now use dual fusion break apart probe and fluorescent in situ hybridization. Take EWS and label each side of it. Side is dependent on where you put the break point. Breakpoint is usually at 22q. So you label each side. So in a normal chromosome they should be right next to each other.

management of preeclampsia
definitive treatment is delivery (at >37 wks it’s recommended, even without severe features)
expectant management if no severe features (daily BP monitoring, lab testing/wk, corticosteroids)
Mg sulfate for labor to reduce seizure risk
anti hyptertensives avoided if BP below 160/110 (don’t change disease process)
termination is offered <24 wks (bad prognosis)
dysgerminoma
from undifferentiated germ cell

Sheets of germ cells interspersed by fibrotic septa – with some lymphocytes
Malignant, very radiosensitive, very good prognosis
invasive ductal carcinoma of the breast
70-80% of carcinomas
irregular spiculate masses
stony hard to cut section
malignant cells in cords, solid cell nests, tubules

staging of cervical carcinoma
- The prognosis of cervical cancer depends on the stage of disease.
- The earlier the stage, the better the prognosis; so much so that if the disease is less than 5mm invasive, called Stage IA, survival is 98%. That’s pretty amazing, you can pick up cancer early and you’ll get close to 100% survival.
- If it’s greater than 5mm invasion, prognosis falls down to 80%.
- If there’s involvement of vagina or parametrium with Stage II, 70%.
- With pelvic sidewall, there’s a considerably worse prognosis, with 35% survival.
- And Stage IV would be mucosal involvement of bladder or rectum, with only 10% survival.

treatment of borderline ovarian surface epithelial tumors
Young patient: Cystectomy/ unilateral Oophorectomy
Older patient: Bilateral salpingo-oophorectomy with hysterectomy and staging
velamentous umbilical cord
- Velamentous – umbilical cord inserted into fetal membrane at edge of the placenta; rare; what’s important is that the blood vessels are now crossing internal cervical oss; if baby trying to push into cervical canal (where the velamentous insertion of the umbilical cord is located à THE BABY TRYING TO PUSH THROUGH THE CERVICAL CANAL WILL SQUISH AND CAUSE RUPTURE OF THE BLOOD VESSELS à THIS CONDITION IS CALLED VASA PREVIA
- BABY NEEDS TO GET C SECTION TO AVOID RISK OF HEMMORRHAGE
- ALSO PRONE TO MECHANICAL INJURIES B/C NO CUSION (usually connective tissue will form a cushion around the umbilical blood vessels; in velamentous insertion, the blood vessels are OUTSIDE of the umbilical cord à don’t have the protective connective tissue cushion à VERY PRONE TO MECHANICAL INJURY!!)


serous borderline tumor
- epithelial stratification (4-5 cell layers)
tufting of epithelium
- mild nuclear atypia - Psammoma bodies (arrow)
- No stromal invasion
ER/PR +
better prognosis!
can be treated with tamoxifen (anti estrogen that blocks ER) or arimidex (aromatase inhibitor)
management of patient at increased risk of preterm labor <32 wks
corticosteroids (reduce risk/severity of RDS)
magnesium sulfate to reduce risk of cerebral palsy
abx to prevent vertical transmission of GBS
tocolysis - delay delivery for 48hrs
primary, secondary, tertiary chorionic villi
Primary CV (trophoblast ONLY), day 12 - 14 (end of 2nd week)
Secondary CV (tropho then acquires mesenchymal core) @3rd wk , day 16
Tertiary CV (blood vessels form end of 3rd wk; can see on H&E section ) , day 21 (3rd - 5th week) à building block of placenta
ovarian cystadenoma
Lining epithelium of the inclusion cyst undergoes metaplasia to become serous or mucinous
Single layer of epithelium lines the cyst cavity
Tumors can become massive, usually filled with serous or mucinous fluid depending on the type of lining epithelium or with blood in case of endometrioma
5 year survival: 100%
All women have inclusion cysts – some get a lot bigger and accumulate fluid because cells become metaplastic into serous or mucinous, lined by SINGLE layer of epihtlium – means there isn’t much epithelial proliferation so it a benign cystadenoma

decidua
Compare w/ img B (end of 3rd trimester) à CV + separated from SM via layer of decidua à THIS IS NORMAL!!
- important b/c if decidual is smaller (ie: b/c of leiomyoma/scar tissue) à CV can grow thru and attach to SM (smooth muscle)à aka placenta atreta à important b/c at delivery of baby, placenta delivered w/ baby (dissection usually along decidual layer; usually smoothly delivered)
- if CV growing into SM, PLACENTA CAN’T BE DELIVERED à can cause hemorrhage!!! Can be deadly!! à pt will need hysterectomy!

how does invasive cervical carcinoma present?
- Spotting or bleeding
- Post coital bleeding
- Abnormal pap smear; this would typically be in a patient who has never had a pap smear in her entire lifetime
- Advanced cases of cancer may present as uremia because cervical cancer tends to grow locally and close off the ureters on the sides, therefore causing uremia.

endometrial hyperplasia with atypia vs without atypia
- On the left, you have glands that are haphazardly arranged.
- They are crowded.
- There is a reduced amount of stroma between the glands, but
- you can delineate every individual gland.
- You can have a nice stroma.
- There is no cytologic atypical in the EM epithelial lining of those glands.
- This is simple hyperplasia without atypia.
- On the other hand, when you look at the right, these glands are very crowded.
- There is hardly any stroma separating these glandular structures from each other.
- We start to have these little outpouching. [The glands look branched instead of round in cross-section.]
- At higher magnification, you have nucleoli where the chromatin is cramped.
- This is an example of complex hyperplasia with atypia, or atypical complex hyperplasia.
- This is the one that is associated with high risk of developing of developing endometrioid adenocarcinoma.

Oncoproteins of HPV?
E6, E7 - bind to tumor suppressor genes in cells
- It was discovered in 1989 that papillomavirus E7 protein is able to bind to retinoblastoma gene.
- Retinoblastoma is a tumor suppressor gene. Once cells lose tumor suppressors, they have increased ability to divide and go on to become tumors.
- One year later, it was found that E6 protein binds to p53, which is important for maintaining normal cells.
what predicts response to treatment and prognosis for wilm’s tumor?
presence/absence of anaplasia

Anaplasia in Wilms Tumor has a specific diagnosis. It is defined by two criteria and BOTH MUST BE PRESENT:
(1) Abnormal polypoid or tetraploid mitotic figures (black arrow)
(2) marked nuclear enlargement [green arrow] and hyperchromasia [blue arrow]. Nuclear enlargement must be at least 3X larger than non-anaplastic adjacent cells
Again it’s very important to distinguish between multifocal and diffuse. In the lab we will take a photomicrograph of tumor section and map out exactly where each section comes from. So we have a diagram that tells us which part of the tumor we’ve taken the section from and if we see anaplasia on that slide we can see how much of the tumor is anaplastic.

serous cystadenoma
30-60% bilateral. Unilocular, smooth walled, filled with serous/clear fluid
Bilat huge cyst – with clear fluid, clear and glistening, benign
breast:

fibroadenoma
cellular fibroblastic stroma enclosing glandular and cystic spaces lined by epithelium
n- FIBROADENOMA EPITHELIUM IS HORMONALLY RESPONSIVE
n- SLIGHT INCREASE IN SIZE AT END OF MENSTRUAL CYCLE OR DURING PREGNANCY
n- REGRESSION OCCURS POSTMENOPAUSALLY LEADING TO HYALINIZATION AND CALCIFICATION
leukoplakia of the vulva
old age
thickened keratotic vulvar skin
biopsy to rule out dysplasia


- Intense vulvar itching and white cheesy discharge are typical of candidal infection.
- You do a Pap smear and you can see the spores and the pseudohyphae. The long elongated structures in the image are the hyphae. You can make the diagnosis of candida.
- The patient will get treated and cured.
what cells give rise to the placenta?
trophoblast cells
During the 2nd wk the trophoblast proliferates rapidly and gradually differentiates into: 1) an inner cytotrophoblast, and 2) an outer syncytiotrophoblast. The erosive trophoblast invades the maternal endometrium (decidua) and blood vessels. This leads to remodeling of the vessels with leakage of maternal blood into trophoblastic spaces (lacunae). The fusion of the adjacent lacunae results in formation of lacunar network where exchange of nutrients and gasses takes place between maternal blood and the developing embryo.
molecular cytopathology
- As we move into the more molecular age, there are things in cytology that use molecular detection. One of these is Urovysion, used to aid in the diagnosis of bladder cancer in pts with hematuria (blood in urine) and to monitor tumor recurrence in pts who already have a hx.
- They just take a urine sample that looks abnormal and do FISH on it and see if they can detect aneuploidy (change in the number of chromosomes).
- They look for certain chromosomes – loss of a particular chromosome that is associated with pts having bladder cancer. Those pts with those abnormalities will probably have to get cystoscopy where they look in with a scope. Most of these pts are just monitored through urine samples, so it adds to understanding that these pts might be at a greater risk and leading to another procedure.


breast cyst
- And most of the time, the breast tissue is this blackish white tissue
- The whiter parts are normal glandular tissue
- The blacker areas are fat because majority of breast is actually composed of fatty tissue
- And this is lesion here [circles oval] and what we see here is this very darkened lesion
- If you look at edges of it, you see that it is very circumscribed, edges are quite smooth. This is characteristic of a cyst.
- It looks black because of greater transmission through fluid

struma ovarii
Monodermal teratoma
More than 50% of the tumor tissue should be thyroid tissue to be classified as Struma ovarii
5-10% patients may have hyperthyroidism clinically
20-30% patients may have thyroid cancer arising in struma ovarii ( commonly Papillary type, occasionally follicular type)
Peritoneal strumosis: Seeding of peritoneum by benign strumal tumor: Rare
Thyroid tissue! More than 50%
neonatal phase
first 28days of life
neuropil
neuroblastoma
As you look at the fibro-stromal background you’ll note that you have thicker pieces of actual fibrous tissue [black arrow] and attached to that you have this more fine fibrillary eosinophlic matrix [green arrow]. This is a very important histologic image for you to remember. The presence of this material which is called neuropil [black circle] is a key diagnostic feature for this tumor. The remainder of this tumor is a typical small round blue cell appearance. You have a very small cell. It’s very dark blue. It’s hyperchromatic. It has sort of inconspicuous nucleoli but it has lots of clumpy or vesicular chromatin.

phyllodes tumors
lobulated and irregular on ultrasound
solid and cystic
leaf-like pattern with stromal hypercellularity
biphasic: neoplastic stromal cells and epithelial lined glands
most are benign but can be malignant (associated w increased stromal cellularity, mitotic figures, rapid increase in size)


thecoma
sex cord derived tumor
Benign
Unilateral
Occur in postmenopausal women
Appears yellow grossly
Produce estrogen: Abnormal uterine bleeding, breast enlargement, endometrial hyperplasia or carcinoma
Post-menopausal – benign, well circumscribed, YELLOW bc fat has cytoplasm
Plump oval shapped cells – can mae estrogen (irregular/post men bleeding

“suspicious” in cytopathology
•If we call something “suspicious”, it means we do see abnormal cells that we think are cancer, but we’re not 100% sure because there’s not enough to definitely make that clear. When we call it “positive”, we want to be right.
epithelium of endocervix and exocervix
endocervix - columnar lining
exocervix - stratified squamous lining
•Shown here is an actual cervical slide, showing the outer part of cervix [red circle], the endocervix [yellow circle] and the squamo-columnar junction [blue circle].

stage III ovarian carcinoma
Stage III: Involvement of lymph nodes or extra-pelvic peritoneum. Five year survival 25%
pap smear recommendations
•It is recommended that women in reproductive age groups have Pap smears every 3 years. Yearly Pap smears used to be the recommendation, but people realized that these lesions don’t progress so fast, so you can still pick them up if you do a smear every 3 years.
Rh positive
his term strictly refers only to the most immunogenic D antigen of the Rh blood group system, or the Rh− blood group system. The status is usually indicated by Rh positive (Rh+ does have the D antigen) or Rh negative
what is post term gestation
>42 wks

chocolate cyst
Called a chocolate cyst because the clotted blood collected very menstrual cycle looks like chocolate
Endometriotic cysts contain clotted blood
Cyst wall is formed by endometrial epithelium and stroma
Endometriotic cysts are considered precursors of endometrioid and clear cell types of ovarian cancer
squamous cell carcinoma of the vulva
- Squamous cell carcinoma: the vulva can present with ulcer, mass, or nonspecific itching.
- Older women
- The lesions are usually well differentiated. In the cervix, lesions are typically poorly differentiated, but in the vulva they’re typically well differentiated.
where in the ovary are the germ cells?
- Outer portion is the cortex that contains the germ cells (primordial follicles) embedded in specialized stromal cells
- Inner portion is the medulla that contains the rich vascular network

extrachorial placenta
Peripheral rim of the placenta is not covered by the membranes. May be associated with vaginal bleeding and leakage of amniotic fluid.

tubular carcinoma of the rbeast
well formed tubules with absent myoepithelial layer and apocrine snouts
axillary metastases uncommon - excelllent prognosis!

pap smear shows HGSIL?
- If the Pap smear shows a HGSIL, these women undergo colposcopy and biopsy.
- Colposcopy is direct visualization of the cervix. So you can sample the most abnormal looking areas.
acute chorioamniotis
- 10% ifx = ascending ifx; usually followed by premature rupture of the maternal membrane
- caused by bacteria growing in mom’s vagina (could be Group B strep)
- Associated w/ increased perinatal mortality
- In asc ifx, when bacteria coming into amniotic fluid, mom’s immune system will respond to the infectionà can see lots of neutrophils that come from maternal decidua à can see lots of neutrophils that come in to fight ifx
- Baby can also get ifx; baby can respond to ifx à will see inflammation in vessels of the umbilical cord umbilical cord
•
•Can see lots of neutrophils in umbilical cord à means baby is also ifx’d L

most common cause of spontaneous abortion?
karyotype abnormalities
Embryonal Rhabdomyosarcoma
•Children ages 3-10 years
▫nasal and oral cavities, orbit, middle ear, prostate, paratesticular region

“atypical” in cytopathology
•Atypical” is sort of a wishy-washy category where we see something that we think is abnormal but aren’t sure.
abrasive cytology
gastring brushings
•Sometimes you have to use more of an abrasive method, and this is mainly in the gastrointestinal tract, where you have to scrape it off or brush it off. When you go through the endoscopy clinic and you’re with one of the gastroenterologists, when they put the tube down to take a biopsy, they have these little brushes that come out from the endoscopy tube and you can swirl it around a little, the cells get stuck to that brush, they put them in a fixative, and we make slides out of those cells to see whether its benign or malignant.
adenocarcinoma of the cervix
- So adenocarcinomas are much less frequent; only about 10% of cervical carcinomas are adenocarcinomas.
- The incidence may be increasing; there’s some evidence for that
- And HPV 18 is frequently detected, as opposed to HPV 16 in squamous cancers.

2 components of the endometrium?
- The lower 1/3 [below the white line], which is the regenerative layer, responds to steroid hormones in a minimal fashion.
- The upper 2/3, whih is the functional layer, sheds at the end of the menstrual cycle, proliferates, and the one which undergoes sexretory differentiation later.
- I wanted to point out to you that it’s very orderly arranged.
- This is the surface of the EM [green arrow]
- The glands are more or less perpendicular to it, and they are parallel to each other. [She gestures vaguely at the circles everywhere.]
- They are evenly spaced.
- It has a very organized look to it, which is important.

cytopathology
cytopathology is different from histopathology (where you’re looking at actual tissue). This is where you’re just looking at cells.
colloid carcinoma of the breast
older women, grows more slowly
well circumscribed, soft due to gelatinous mucinous material
small enoplastic cells float in lakes of mucin
excellent prognosis, low incidence of ln metastais

medullary carcinoma of the breast
younger women
well circumscribed
slightly better prognosis
- One is syncytial nests of very large pleomorphic cells with prominent nucleoli and frequent mitoses [mouses over pale pink part on top image]
- The other is that it is surrounded by this lymphoplasmacytic infiltrate
- So there are lymphocytes and plasmacytes surrounding it [mouses to part around the syncytial nest with lots of nuclei]
solid sheets of large cells pleomorphic nuclei with prominent muceloli and requent mitosis
lymphoplasmacytic infiltrate surrounding
**pushing borders

what if umbilical cord is too long or too short?
•Length, mean 60 cm
–Long
•knots, prolapse, strangulation
–Short
- abruption, uterine inversion, umbilical hernia
- psychomotor impairment
three patterns of non-proliferative fibrocystic change of the breast
- Have cysts – the black things
- Fibrosis – the white part on the top picture
- Adenosis – just an increase in the number of acini within a lobule

acute atheros
in toxemia of pregnancy

•Name of the pathologic changes in toxemia = ACUTE ATHEROSIS
•
•When maternal blood vessels in decidual is destroyed + replaced by fibrin (aka fibrinoid tumor) à lots of foamy histiocytes + cells around it
•
- In Toxemia à correlation btwn morphology + clinic presentation ISN’T VERY GOOD!
- Pt can have really bad clinical presentation, but no changes in blood vessels!
chronic salpingitis
Chronic Salpingitis: Chronic inflammation, fibrosis and fusion of plicae, scarring leading to:Tubo-ovarian adhesions, Tubo-ovarian abscess, Pyosalpinx, Hydrosalpinx, Ectopic Pregnancy, Infertility
PID ( pelvic inflammatory disease ) = chronic salpingitis with involvement of surrounding structures including ovary and parametrium
PID is characterized by exacerbations of acute episodes
IUD usage is associated with Actinomyces infection which is rare otherwise: Risk of infection is related to the length of IUD usage, 85% cases occurring after 3 or more years of IUD usage
succenturiate placental lobe
- Usually see succenturiate aka accessory lobe
- usually not a problem; will have an irregular piece of placental tissue
- just check to make sure the vessels in the accessory placenta are intact in case they break b/c they’re not protected by placental parenchyma/membrane surrounding the normal placenta

Treatment of ductal carcinoma in situ
segemntal excision wth radiation
mastectomy if extensive
doesn’t metastasize - no need for LN dissection
type I ovarian cancer
Indolent and Present as stage I
Develop from well established precursors such as
- Borderline tumors
- Endometriosis
Type I ovarian tumors follow the traditional model of pathogenesis i.e. they start as surface inclusion cysts, undergo metaplasia to form benign tumors and then dysplasia to form first borderline and then malignant tumors.
Common mutations seen in type I tumors are KRAS, BRAF
Mucinous adenocarcinoma, Clear cell carcinoma and low grade serous and endometrioid carcinoma are type I ovarian cancers
presentation of hydatidiform mole
vaginal bleeding in 1st trimester
uterus larger than expected
HTN in first trimester
elevated HCG

atypical ductal hyperplasia - 4-5x risk
risk factors for breast cancer
n- H/O PROLIFERATIVE BREAST DISEASE (1.5-2X) (4-5X FOR ATYPICAL DUCTAL HYPERPLASIA)
n- GEOGRAPHIC INFLUENCE: US AND NORTHERN EUROPE HAVE HIGHEST RATE
n- LENGTH OF REPRODUCTIVE LIFE: INCREASES WITH EARLY MENARCHE AND LATE MENOPAUSE
n- PARITY: MORE FREQUENT IN NULLIPAROUS
n
n- AGE AT FIRST CHILD: RISK INCREASED IN WOMEN OLDER THAN 30
n- POSTMENOPAUSAL HORMONE REPLACEMENT THERAPY SLIGHTLY INCREASES RISK
invasive lobular carcinoma of the breast
5-10%
strands of infiltrative tumor cells in a single file pattern
no formation of tubules
lacks e-cadherin

amnion nodosum
assoc w oligohydraminos and fetal urinary tract abnormalities must be excluded

- Surface of placenta should be smooth and glistening; but this placenta is sick à bumpy usually b/c of oligohydramos (not enough amniotic fluid à amniotic fluid produced by kidneys of fetus
- Should check for kidney/urinary problems in the fetus
meconium staining of fetal membrane
Green discoloration of membranes due to staining by the colonic contents, normally seen in association with fetal distress. There may be hyperplastic changes in the amnion layer with pigment-laden macrophages beneath.
Can also see meconium staining (greenish staining on fetal plate) à when baby in distress, it will pass meconium that stains fetal membranes à meconium = chemical irritant; can lead to inflammation; black brown spots = meconium eaten by macrophages

embryonal carcinoma
Embryonal carcinoma is comprised by undifferentiated totipotential cells. Responds well to chemotherapy.
totipotent cell without further differentiation
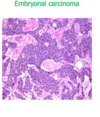
genetic makeup of partial mole
- TRIPLOID à 1 nml egg fert by 2 sperms à 69 chromosones
Complete + partial mole = 2 sets of DNA from dad
Complete = 2 sets of DNA from dad + no DNA from mom

pathogenesis of polycystic ovary disease
The basic central pathogenesis is supposed to be increased production of androgens from ovaries. The theca cells are producing a lot of androgens, so there is increased serum androgens, which are being converted into estrogen by granulosa cells, and a lot of patients are obese, so they have their adipose tissue converting it into estrogen.
We saw on the last side that when there is increased serum estrogen, there is increased LH because estrogen stimulates the productive of LH. When there is a lot of LH and estrogen, FSH production goes down.
àààHave high androgens (like testosterone or DHEAS), so high estrogen, and high LH and decreased FSH.
LH/FSH ratio is supposed to be 2-3:1
Because there is a high level of estrogen, and low progesterone because there is no ovulation taking place (no corpus luteum creation), there is increased risk of endometrial carcinoma.


