Psychobiology and motivation (year two) Flashcards
Name the 5 major structures in the brain
- Myelencephalon: medulla, comprises tract between brain and spinal cord
o hindbrain - Metencephalon: pons and cerebellum
o hindbrain - Mesencephalon: thalamus and hypothalamus
o midbrain - Diencephalon: thalamus and hypothalamus
o forebrain - Telencephalon: cerebral cortex, limbic system, basal ganglia
o Forebrain
Describe the composition of the cerebral cortex
- Made of grey matter – small unmyelinated neurons
- White matter= large myelinated axons
- Convolutions – increase surface area
o Large – fissures
o Small – sulci
o Ridges between fissures and sulci – gyri - Longitudinal fissure separates hemispheres (connected by cerebral commissure, incl corpus callosum
- Contains neocortex and subcortical structures (hippocampus, limbic system, basal ganglia)
Describe the composition of the neocortex
- Newest part of cerebral cortex
- Neocortex = largest part of cerebral cortex (90%), other 10% is allocortex (cont hippocampus)
- Six layers
- Large neocortex ratio, correlates with complexity of behaviour
- Central/lateral fissure divide each hemispheres into 4 lobes
Give the neocortex lobes and state their functions
- Frontal lobe: motor cortex (precentral gyrus)
o Complex cognition in frontal cortex - Parietal lobe: (post central gyrus)
o Somatic sensations, orientation, object location - Temporal lobe: hearing and language
o Complex visual patterns
o Memory - Occipital lobe: visual processing
Explain the origins of phrenology
- Franz Joseph Gall (1758-1828) founded phrenology
- Tried to make assumptions about intellect and personality from examination of skull shape - assumed surface of skull reflected regions of brain development
- Classmate could recite long passages of prose and had bulging eyes – assumed that verbal memory lay in frontal region behind eyes
- Lectures on crainioscopy offended religious leaders and was banned in 1802 by Austrian government
- Identified 27 cranial regions that corresponded to traits
- Found regions responsible for murder/inclination to steal (felt criminals heads to detect patterns
Give some of the positive contributions of phrenology to modern day psychology
o Believed brain was physical organ of the mind
o Proposed that cerebral cortex contains localised function areas (proved right, broca’s area and motor cortex)
o First to identify grey matter with neurons and white matter conducting tissue (ganglia)
Describe how lesion studies led to the discovery of Broca’s aphasia
- Broca consulted about patient with neurological issues and no speech
- Could only say word “tan”
- Autopsy revealed left frontal lobe lesion
- Second patient: stroke patient, could only say 5 words
o Same lesion as Tan
o Known as Broca’s aphasia: inferior frontal gyrus on left cerebral hemisphere
Describe how lesion studies led to the discovery of Wernicke’s aphasia
- Broca: damage to Broca’s area should disrupt production, not comprehension
- Wernicke: lesions to Wernicke’s area produce primarily receptive syndromes
o Wernicke’s aphasia: poor written and spoken language comprehension, meaningless speech, speech still retains structure/rhythm/intonation
o “Word salad”
o Left temporal lobe
Explain what Brodmann areas are and how they are organised
- German neurologist Korbinian Brodmann (1868 – 1918)
- Produced maps of train based on cytoarchitectural organisation of neurons in CC (using nissl method of cell staining)
- Identified 52 areas of cerebral cortex differing histologically (cells/structures) – Brodmann’s areas
- Defined solely on neuronal organisation – since been correlate to diverse cortical functions
- Provided map based on collections on neuron types – examined using lesion studies, experimental ablation, functional neuroimaging
Define functional neuroanatomy
- Moved from basic naming of lobes to naming areas by function e.g motor areas, visual cortex
- General classification of three functional areas: sensory, motor and association
Describe the functions of the prefrontal cortex
- Very developed in humans
- Belies complex cognition, thought, social behaviour, personality etc
- Executive functions: higher order cognitive functions – word fluency, inhibition, switching attention
- Working memory
- Recall
Explain the implications of prefrontal cortex damage
- Early studies: large portions of PFC can be removed without loss of mental capacity – gave revise to development of lobotomy/leucotomy
- Lobotomy: severing connections from PFC to other brain areas
- Procedure introduced by Antonio Egas Moniz – won nobel prize for medicine for discovering lobotomy as a treatment for psychosis
- Mixed success: some patients more docile, others committed suicide or were severely brain damaged
- David Ferrier (1876): ablation of frontal lobes in monkeys resulted in loss of faculty of attentive and intelligent observation but senses unimpaired
Give the subdivisions of the prefrontal cortex and their functions
- Dorsolateral PFC: working memory, rule-learning, planning
- Orbitofrontal PFC: inhibitory/emotional control and inability to function in social domains
- Ventrolateral PFC: human inferior temporal gyrus, disparate functions - spatial attention, inhibitory control, language
Describe the role of the primary motor cortex and what led to its discovery
- Precentral gyrus
- 1937: Penfield and Boldrey mapped primary motor cortex of conscious human patients during neurosurgery with electrical stims on cortical surface (noted which body parts moved in response to stimulation)
- Each stimulation activated a contralateral muscle and produced simple movement – primary motor cortex is organised somatotropically
- Somatotopic layout referred to as motor homunculus
Describe the implications of lesions to the primary motor cortex
- Extensive damage to PMC doesn’t eliminate all voluntary movement
- Large lesions to PMC disrupts ability to move individual body parts independently, reduces speed/accuracy/force
- Other movements able due to association and secondary motor areas
Describe the role of association motor areas
- Posterior parietal association cortex: integrates orientation info about body parts/external objects positions
- DLPFC receives projections from posterior parietal cortex and projects to secondary motor cortex, primary motor cortex and frontal eye field
- DLPFC responds in anticipation of motor activity
Describe the role of the secondary motor cortex and explain how it processes information
- Receives input from association cortex
- Premotor cortex:
o Anterior to primary motor cortex
o Receives highly processed sensory info
o Planning of movement - Frontal eye field
o Anterior to premotor cortex
o Controls voluntary eye movements - Electrical stim of secondary motor area elicits complex movements, involving both sides of body
Describe the role of sensory areas and what they consist of
- Consist of primary, secondary and association areas
o Primary areas receive input from thalamic relay nuclei
o Secondary cortex receives input from PSC or other secondary areas
o Association areas integrate info from more than one sensory system - Posterior parts of brain behind central sulcus
- Large parts of brain dedicated to processing sensory stimuli
- Postcentral gyrus = location of PSC
Describe the role of the primary somatosensory cortex
- Penfield et al. (1937) – electrical stim to cortical surface (conscious patients)
- Brodmann areas 1-3 (in postcentral gyrus) – sensations in various areas
- Somatotropic organisation
- Medial parts = leg, lateral parts = face – more sensitive to touch
- Distribution biased towards areas with high sensory discrimination e.g fingers, mouth
- SII (secondary somatosensory cortex): ventral to PSC in postcentral gyrus – receives input from PSC
Explain the implications of damage to the somatosensory system and association cortex
- Damage to PSC has mild effects
- Corkin et al (1970) – unilateral lesion of PSC in epileptics – two minor contralateral deficits – ability to detect light touch, reduced ability to identify objects by touch
- Somatosensory signals conducted to highest level of sensory hierarchy is association cortex
Describe the role of the visual cortex
- Vision represented in brain in three main regions
- Primary visual cortex: posterior occipital lobe
o Most input from visual relay of thalamus - Secondary visual cortex (prestriate and inferotemporal cortices) : receive input from PVC and visual association cortex
- Association cortex: posterior parietal cortex
Explain the implications of damage to the primary visual cortex
- Produces a scotoma (area of blindness) in corresponding area of contralateral visual field
o Contralateral = side of body that is opposite to that of the brain structure - Many patients unaware of scotomas – visual completion occurs
Give the areas of the visual system
- 12 functional areas of VC identified
- About 30 in monkeys (24 secondary, 7 association)
- Selective lesions produce different visual losses
Define and locate the dorsal and ventral streams
- Info from PVC projects to areas of SVC and AC by dorsal and ventral stream
o Dorsal stream: projecting up to posterior parietal cortex
Spatial stimuli (location of objects, movement)
o Ventral stream: projects across to inferotemporal cortex
Characteristics of object (colour, shape)
Describe what deficits can result from damage to the dorsal and ventral streams
- Damage to posterior PC – can describe objects but can’t touch them
- Damage to ITC – difficulty describing, but can pick them up
Describe what can happen if there is damage to the secondary visual cortex
- Prosopagnosia (face blindness)
- Coined in 1947 by Joachim Bodamer
- Usually results from damage to right fusiform gyrus during head trauma/stroke/degenerative diseases
Give examples of sensory areas and their Brodmann areas
- Auditory areas – primary auditory cortex: superior temporal lobe, inside lateral sulcus (BA 41)
o Auditory association area: posterior to PVC (BA22) – evaluates sounds - Gustatory (taste) cortex – BA43, roof of lateral sulcus
- Olfactory cortex – medial temporal lobe, connects to limbic system
- Association areas are where primary inputs are processed/comprehended
Define and explain the role of monoamine pathways
- Neurotransmitter pathways have been mapped
- Dahlstrom and fuxe (1964) – used immunofluorescence staining to visualise pathways of serotonin, dopamine and noradrenaline
- MN emanate from brainstem and project to forebrain and beyond
Define and explain central lateralisation of function
- Left/right cerebral hemispheres separated apart by cerebral comissures
- Dax (1836) – 40 brain damage patients had speech problems and damage in left hemisphere
- FMRI, PET, unilateral lesions, split brain patients studied
o Language/motor abilities of left hemisphere apparent
o No substantial differentces between hemispheres, may only have slight biases - Lateralisation is statistical – language is most lateralised
- Some skills show hemispheric dominance
Describe and explain how functional MRIs work
- Shows structure and activity of brain
- Blood flow are neuronal activation coupled
- FMRI detects changes in blood flow due to blood being diamagnetic
- Laird et al. (2009) Extensive convergence in large portions of left inferior frontal gyrus, centering on BA 44/45 (Broca’s area)
Define and explain functional connectivity analysis
- fMRI analysis technique to observe which brain areas correlate with another in terms of activation
- Can measure BOLD signal from entire brain during task encompassing the reward system and compare to relevant groups
- Can examine BOLD signal changes associated with the trains when we expect system level activation
Describe how technology is advancing frontiers in neuroscience
- Transcranial stimulation: non-invasive method of brain stimulation
o Relies on electromagnetic induction using insulated coil placed over the scalp
o Focused on area of the brain thought to play role in mood regulation - Brain computer interface: can help those with paralysis of the body to communicate using electrical signals from their brains
Define morphology
Morphology: classification in terms of number of neuronal processes (projections from cells)
Give two types of multipolar neurons
Two types of multipolar neurons
Golgi 1 neurons: long axons
Golgi 2 neurons: shorter axons, project locally
Give the three major purposes and types of neurons
Three major purposed:
Sensation – afferent neurons
Gather/send info from senses
Integration – interneurons
Process all info gathered
Action – motor neurons
Send signals to effectors e.g muscles and glands
Give a definition of pain
“An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage” – International Association for the Study of Pain (2020)
Give the three dimensions of pain
Dimensions of pain:
Sensory: physical stimulus, intensity, location
Affective: unpleasantness, emotions
Cognitive: attention memory, expectation, imagination
Explain sensory integration
From receptors to spinal cord to brain
Transmitted via primary sensory neurons (nociceptors) – spinal cord – streamed up to CNS via multipolar neurons (golgi 1 type)
Describe projection neurons
Projection neurons: project from spinal cord to the brain
Define nociceptive-specific neurons
interneuron specialised for processing pain
Define Wide-dynamic range neurons
interneuron specialised for dealing with painful and non-painful stimuli
Define descending pathways
Descending pathways: neurons descending from brain to spinal cord to modulate pain in SC, dictates pain sensitivity
Explain how nociceptive processing is arranged in the central nervous system
Nociceptive processing in CNS is distributed and degenerate
See Coghill R
Distributed: processing is done independently by multiple sites in CNS, multiple brain regions activated in parallel
Degenerate: have a very resistant pain response system: there is no single brain centre. Not one area of the brain can be disturbed and completely stop pain sensation
Multiple brain areas dedicated to pain, all with the same function
Describe the role of sensory neurons
Contains receptors (either cellular e.g vision, molecular e.g pain)
Translate receptor codes to neural codes
Transmit information to CNS
E.g visual neuron: bipolar, attached to cellular receptor (cilia sensitive to physical stimuli of light)
E.g of cellular receptor: rods and cones
Describe the anatomy of nociceptors
Nociceptors (pain sensors) are free nerve endings
Epidermis doesn’t contain nociceptors
Nociceptors contained in dermis
Describe the anatomy of the epidermis
Epidermis doesn’t contain nociceptors
Nociceptors contained in dermis
Merkel discs and Meissner discs: cellular receptors at end of touch fibres, detect different subtle types of pressure
Molecular receptors: small compared to cellular receptors, polymodal (detect many types of pain e.g pain by pressure, chemical pain – chilli from capsaicin, temperature)
Describe the role of TRP channels
TRP channels: most common type of molecular receptor for pain
Voltage gated calcium channels
Describe the role of the TRP V1 channel
TRP V1 channel let calcium into cell from outside, triggering change in membrane voltage generating action potential
Agonists: temperatures above 43’, capsaicin, anandamide (found in chocolate and plants, fatty acid neurotransmitter), acid environments, osmotic pressure
Define conformational change
Conformational change: change in protein structure allowing calcium ions to enter into cell, depolarising the membrane and generating action potentials
Describe the anatomy and role of C fibres
C fibres:
non-mylinated
carry mechanical, thermal and chemical pain
- 2-1.5 mm diameter
- 5-2m/s conduction speed (walking)
Describe the anatomy and role of A-Delta fibres
A-delta
Mechanical and thermal pain
Myelinated
1-5 mm diameter
5-40 m/s conduction speed (cycling)
Describe the anatomy and role of A-beta fibres
A-beta
Touch information
Myelinated
6-12 mm diameter
35-90 m/s conduction speed (race car)
Describe the anatomy and role of A-Alpha fibres
A-Alpha
Proprioception
Myelinated
13-20mm diameter
80-120 m/s conduction speed (jet plane)
Explain which fibres and responsible for first pain
A-delta fibres responsible for first sensation of pain, C fibres responsible for slower, aching pain
First pain sensation takes 2-300ms
Explain which fibres are responsible for second pain
Second pain sensations take 1 second to reach the brain, longer duration
EEG: c fibre has lower amplitude and is harder to measure on EEG
First pain encoded partly within somatosensory cortex, second pain encoded in anterior cingulate cortex and posterior insula cortex
Describe the nociceptive pathway in the spinal cord
Peripheral sensory neurons have cell bodies in dorsal root ganglion (unipolar neurons), axons continue into dorsal horn and synapse on various interneurons or projection neurons (these cross spinal cords and enter spinothalamic tracts – goes to brain)
10 laminae in spinal cord: different types of cells, including different types of neurons
Describe where substantia gelatinosa and WDR interneurons are found
Substantia gelatinosa interneurons
Mainly found in laminar 2
Wide dynamic range interneurons
Mainly found in laminar 5 and 3
Explain the gate control theory
Important for gate control theory
Non-painful sensory inputs close the “gates” to painful input, reducing pain
SG neurons of dorsal horn are inhibitory
C fibres (pain) inhibit SG neurons
Ab-fibres (touch) excite SG neurons
SG acts as gate and determines whether pain is encoded within WDR neurons that transmit info to brain
Explain the population coding theory
Population coding theory
Recruitment of larger numbers of WDR neurons is associated with increasing intensities of pain
Relationship between WDR neurons and pain could be due to WDR neurons having larger receptive fields (provides mechanism for spatial summation of pain)
WDR neurons selectively expand receptive fields in response to nociceptive inputs
Increasingly intense noxious inputs increase size of RFs – more WDR neurons activated by more intense stimuli
Noxious stimulus intensity can be encoded by progressive recruitment of increasing WDR neurons
Noxious inputs = pain inputs
Explain spinal integration
Spinal distribution of nociceptive input/ potential neuron recruitment may be driven by widely branching primary afferents and propriospinal interconnections
Primary afferents (A-delta and C-fibres) branch before entering spinal cord
Activation of ascending neurons in segment
Activation of ascending neurons in a different segment
Propriospinal interconnections may transmit nociceptive information, even to contralateral dorsal horn
Propriospinal interconnections provide substrate for wide ranging facilitation/inhibition of neurons across many spinal segments
Explain lateral inhibition
Spatial perception sharpened due to inhibitory integration process
Also explains nonlinearity of spatial summation of pain i.e stimuli that are close together summate less than those further apart (up to about 20cm)
Explain and define pain pathways
1st neuron: spinal ganglion – grey matter of spinal cord
2nd neuron (projection neuron, excitatory): grey matter – thalamus, crossing in anterior part of spinal cord
3rd neuron: thalamus (ventrobasal complex) – multiple brain areas of cerebral cortex activated parallel
Somatosensory cortex, posterior insula, anterior cingulate cortex , amygdala
Amygdala can be activated by parabrachial nucleus which bypasses the thalamus, can be activated earlier
All send info in a descending fashion, back down via the amygdala into the brain stem, first to periaqueductal gray then to rostral ventromedial medulla (involved in descending modulation of spinal cord)
Spinothalamic tract (anterolateral system)
Explain and define descending nociceptive control
Endogenous opioid-mediated
These are primary neurotransmitter by which insula, ACC, amygdala and hypothalamus communicate with brain stem
Info is send to first region in brain stem within midbrain – contains nucleus called periaqueductal gray
Info then sent from PAG to medulla, containing rostral ventromedial medulla
Midbrain and medulla work together and act like computer system
PAG like computer which receives info from cortical regions via endogenous opioid system then weighs up info and decides how much inhibition to apply to spinal cord
This weighing up is then sent to medulla, which acts as executer – executes instructions from PAG
Switches from opioid system to serotonin system and sends descending projections down long neurons (up to 1m) and NT now involved is serotonin
Give evidence for descending nociceptive control
Electrical stim of PAG/RVM causes behavioural suppression to pain response (Reynolds, 1969)
Microinjections of morphine opioid receptor agonist has the same antinociceptive effect
Explain research findings on investigating the integraity of neuroanatomy following potential insults due to heavy drug use
Ecstasy/MDMA produces effects by stimulating release of serotonin
Increases in serotonin neurotransmission following MDMA use is produced by action at serotonin transporter (SERT)
Can measure integrity of serotonin is PET and SPECT scans
Use makers for pre/postsynaptic serotonin
Participants injected with radioligand – radioactive tracer that will bind to SERTS or postsynaptic 5-HT neurons
Studies compare regular ecstasy users to controls (no ecstasy use)
Data meta-analysed over all studies
RESULTS
Ecstasy users showed significant SERT reductions in 11/14 brain regions, including every neocortex/limbic region
LIMITATIONS
7 Studies, low statistical power
Could not do meta regression to correlate drug use with SERT data
Use of other drugs cofound – few people use only ecstasy (ends up being drug users vs nondrug users)
Cannot say anything about reversibility of effects
Self-report issues
No data on actual cognitive function
No report on purity of the ecstasy taken – only know crude mention of ecstasy taken
Could assume effects were due to ecstasy as no known effect of cannabis on serotonin, but would be a guess
Explain research findings of regular cannabis use on neuroanatomy
Regular cannabis use associated with comorbid psychopathologies, higher levels of depression, anxiety, psychosis, deficits in performance in areas of cognition incl reward processing, learning and memory
SMRI
Regular exposure to cannabis (ongoing use and up to 28-day abstinence)
Reduced hippocampus volumes compared to controls – involved in memory
Reduced orbitofrontal cortex volumes – reward processes thought t be relevant in aetiology of substance dependence – motivation and reward functions
LIMITATIONS
Small statistical volumetric group differences – considerable overlap between regular cannabis users and controls
Neural differences between cannabis users and controls may normalise with prolonged abstinence
Cannabinoid compounds encapsulated in commonly smoked cannabis may exert independent/interactive effects
Define degeneracy
Lack of specialisation
Multiple brain areas responsive to pain
Even if anterior cingulate cortex is removed (as tried in history) pain does not cease
Damage to an area of spinal cord does not completely cause loss of pain sensation
Neuropathic pain: can increase the pain you feel, caused by damage to nerves
Difficulty to feel non-noxious sensations e.g vibration
Explain which integrative neurons are responsible for the perception of pain intensity. Include research findings in your answer
substantia gelatinosa interneurons
gate neurons
mediate between touch sensation and pain sensation
wide dynamic range neurons
original article: Coghill, R.C et al (1993) – gerbil strangler
would apply different temperature plates to rats
pain threshold for temperature on skin: 49’C is moderate to high temperature
would disconnect brain from spinal cord before studying spinal cord – modulation complicates data
peripheral nociceptors innovate L4 (region of spinal cord) at 45’C – activate of wide dynamic range neurons
WDR neuron activate in area L2-L5 at 49’C
Give evidence for wide dynamic range receptive fields
EVIDENCE: WDR receptive fields
Expansion of WDR receptive fields
Original article: Cook, A.J et al (1987)
20 second electrical stimulus applied to brain (low to high intensity)
Low receptive field for low intensity (just toes)
High receptive field for high intensity (whole leg) - more WDR neurons activated
Give evidence for spatial summation
EVIDENCE: spatial summation
Large receptive fields of WDR neurons support spatial summation, since the same neuron can respond to stimuli at 2 different locations
Can occur even when stimuli are separated by 40cm in humans
But, maximal at 55- and 10-cm separation distances (smaller distances summate less – due to lateral inhibition)
Original article: Quevado, A.S. and Coghill, R.C (2009)
Explain whether you need a brain to respond to pain
withdrawal reflex
sensation can be modulated by expectation
attention modulates spatial summation
when participants were instructed to provide an overall rating of 2 noxious stimuli, substantial spatial summation of pain was detected
caused by top-down modulation of spine
attention modulates spinal nociception
neuronal responses to painful stimulation in dorsal horn were significantly reduced under high WM load
reductions of spinal responses correlated with distraction from pain effect: reduced pain perception by distraction
likely to involve both opioidergic and nonopioidogenic – opioid antagonist did not completely block the anti-nociceptive effect of distraction
regions of anterior cingulate cortex have projections in laminae V-VII (including WDR neurons) – may provide attentional information to spinal neurons
ability to distract from pain can be life-saving e.g during war
Describe the role of PAG, RVM AND DLPT in descending nociception
PAG calculates how much analgesia to apply from opioidergic inputs from multiple brain regions
RVM and dorsolateral pontine tegmentum (DLPT) – exerts anti-nociceptive effect via serotonergic projections down to spinal cord
When you get hurt – and it’s not a serious injury – you instinctively start to rub the affected area or start shaking it vigorously. Which types of interneurons do you think might be involved?•
Theory: Gate Control Theory of Pain
C-fibres inhibit and Ab-fibres excite substantia gelatinosa (SG) of the dorsal horn
The SG consists of inhibitory interneurons that act as the gate and determine which signals should reach the WDR cells and then go further through the spinothalamic tract to reach the brain
Substantia gelatinosa (SG) neurons:–Multipolar - short axons–Spinal cord – lamina II–Inhibitory interneuron–GABA neurotransmission
Other relevant neurons:–WDR neurons: Multipolar with long axons; Spinal lamina V; Excitatory ascending projection neurons; Glutamate.–Peripheral nociceptors (e.g. C-fibres): Pseudo-unipolar; DRG (cell body); Excitatory; Glutamate.
Explain the therapeutic implications of gate control theory
TENS (transcutaneous electrical nerve stimulation)
Trains of high-frequency electrical stimuli, applied to the skin (nerve), attenuate pain for minutes or hours
Explain how spinal cord stimulation can help neuropathic pain
Stimulation of the dorsal horn tract system alleviates chronic pain: therapy by direct or epidural electrical simulation of the spinal cord
Article: Stancak et al., Eur.J.Pain (2008)
Explain how sensory adaptation occurs in context change
Exposure to bright light: pupils constrict and photoreceptors become less sensitive – stops you becoming overwhelmed
Eating fruit after chocolate cake – being underwhelmed
Explain peripheral adaptation
Peripheral adaptation: reduces amount of info that reaches CNS
Level of receptor activity changes – receptor responds strongly at first then gradually declines e.g change in retina, inner ear muscles
Explain central adaptation
Central adaptation: at subconscious level, further changes the amount of detail arriving at the cerebral cortex
Along sensory pathways in CNS
Involved inhibition of neurons along a sensory pathway e.g spinal cord, brainstem
Gradual decrease in the neuronal response of the sensory system, over time in response to a constant stimulus
Give examples of central adaptation
Sharpening: enhancing discrimination
Exposure to a complex stimulus can increase the ability to discriminate its features over time
Maintaining perceptual constancy: invariant percepts despite varying contexts e.g colour constancy
Highlighting novelty:
Detecting and responding to novel events is crucial for survival in a rapidly changing environment
Frees up attention/resources to attend to other stimuli
Efficient coding:
So that neural resources are not wasted on expected properties of the stimulus and can be devoted to signally unexpected stimuli
Explain predictive coding
As a compression tool
Linear predictive coding used since 50s to compress audio speech patterns for better transmission
As a general mechanism of perception
Efficiency is important for brain to minimise energy expenditure (20% of body total energy)
Accounts for some properties of extra classical receptive fields in dorsal ventral stream e.g sharpening
Give the symptoms of complex region pain syndrome
Symptoms:
Intense/exaggerated pain
Hypersensitivity to touch, hot/cold
Fluctuated swelling
Changes in skin colour/temperature
Changes in sweating/nail/hair growth
Pathophysiology is complex and varies
Range of biomarkers needed to support patient stratification/improve diagnosis certainty
Give some neuropsychological markers of CRPS
Increased 2-point discrimination threshold: stimulates two close together places on the skin
Digit identification: 48% of CRPS patients impaired for accuracy (Forderreuther et al., 2004)
85% patients impaired for accuracy OR response time (Kuttikat et al., 2017)
Stereognosis: identifying objects
Hand laterality recognition: identifying left or right hand
Give hypotheses of how integration contributes to CRPS
Theory: problems with spatio-temporal integration contribute to CRPS
Possibilities
Deficit in bottom-up adaptation – would increase overall response to spatially repetitive stimuli over time
Deficit in top-down adaptation – would increase responses to spatially rare stimuli over time
Explain the predictive coding model
Brain tries to predict sensory inputs; must contain representations of input probabilities
Larger mismatch responses thought to be prediction errors
Give the conclusions of Brown et al.
Larger “prediction error” like signal in CRPS patients
Results consistent with inefficient predictive coding in CRPS patients
Suggests deficit in top-down central neuronal adaptation
.Describe how postsynaptic potentials are generated
Postsynaptic cell membrane is polarised – resting-potential of approx. -70mv
NTs in synaptic cleft bind to receptors 9on the postsynaptic membrane and open channels
This allows sodium/potassium/chloride/calcium ions to enter cells – changes degree of positive or negative charge inside cell
Explain hyperpolarisation and depolarisation
Adding +/- ions can:
a. Positive ions increase likelihood signal will be sent by neuron
i. By making charge on PS membrane more positive e.g 70mv to 67mv
ii. Depolarises neuron
iii. Called excitatory postsynaptic potentials
b. Negative ions make it less likely that signal will be sent
i. By making charge on the PSM more negative e.g -70mv to -72mv
ii. Hyperpolarises neuron
iii. Called inhibitory postsynaptic potentials
Define graded in terms of PSPs
Change in post-synaptic potential is graded
a. Stronger signals from neurons result in greater depolarisation or hyperpolarisation
Explain how postsynaptic potentials are conducted
1Potential conducts passively from site of origin
- Conduction of PSPs have 2 important characteristics:
o Rapid – instantaneous
o Decremental – get smaller as they travel
- PSPs do not travel more than a few mm from site of generation before degrading
Describe how integration of PSPs works
- Typical postsynaptic neuron receives signals from many presynaptic neurons at the same time
- Balance between excitatory/inhibitory PSPs determines whether action potential fires
- Integration = combining number of signals into one signal
- Threshold of excitement: usually -55mV
o If net sum of signals reaching axon initial segment (next to axon hillock) depolarises membrane to this level, then an action potential will fire
Define temporal and spatial summation
Spatial summation : integrating incoming signals over space
- Temporal summation: integrating incoming signals over time
Explain why an action potential fires
If integration of PSPs conducts/surpasses threshold of excitation at the axonal hillock – action potential will fire
Describe action potentials
Action potential
o Membrane potential is reversed (negative to positive)
o Very quick (1msec)
o All or none response
Describe the moving of ions from resting potential to hyperpolarisation
Resting potential: voltage gated ion channels closed
- Depolarisation: Sodium channels open, rapid influx of Na+ into cell
- Peak: Na+ channels begin to close, K+ channels open
- Repolarization: Na+ stops entering cell, K+ ions move out
- Hyperpolarisation: K+ channels start to close but some K+ ions continue to move out
Define refractory period and the types of RP
Potential after signal has been sent
- Absolute refractory period: brief period, impossible to generate an action potential
- Relative refractory period: higher than normal levels of stimulation required to generate action potential
Define refractory period and the types of RP
Potential after signal has been sent
- Absolute refractory period: brief period, impossible to generate an action potential
- Relative refractory period: higher than normal levels of stimulation required to generate action potential
Explain how refractory periods are responsible for direction of travel and rate of firing
RESPONSIBLE FOR:
o Direction of travel – soma to axon
Prevents action potential from travelling backwards
o Rate of firing – indicating strength of stimulus
Strong stimulus allows neuron to fire after absolute refractory period
Weak stimulus will note generate action potential until after relative refractory period
Describe and explain propagation
APs travel along axon depolarizing as it goes
- In grey matter – active process: none-decremental
- As with AP generation, conduction of AP along the axon occurs due to influx of sodium – requires opening of sodium channels
Explain how action potential conduction changes when axons are myelinated
Aps travel faster in white matter – axons myelinated
- Saltatory conduction: within myelination sections of axon the signal is conducted passively (decrementally) without needing the opening of channels – augmenting effect on efficiency and speed of transmission
Give the two types of neurotransmitters
Small molecule NTs
o Few components e.g single amine components/ short chains (amino acids)
2. Large molecule NTs
o Contain between 3-36 amino acid molecules
o Often known as neuropeptides
o 100+ identified, categorised into functional groups e.g pituitary peptides, opioids, brain-gut peptides
Define monoamines and describe the two types, giving examples
Singular components
- Catecholamines:
o Dopamine
o Norepinephrine
o Epinephrine
- Indolamines
o Serotonin (5H-HT) 5-hyproxytryptamine
Explain how dopamine and serotonin can be modulatory
Modulatory NTs: can be both excitatory and inhibitory – varies by receptor
o At least 5 dopamine subtype receptors
o At least 14 serotonin receptor types
- Prevalence of receptors with varying functions can form pathways
Give some of the major dopaminergic pathways and their functions
VTA = Ventral tegmental area
- Nigrostriatal: substantia nigra → striatum (motor control/movement)
- Mesolimbic: VTA → Limbic system (reward/reinforcement – addiction)
- Mesocortical: VTA → prefrontal cortex (working memory, planning)
- Tuberoinfundibular tract (hypothalamus → pituitary) (neuroendocrine regulation
Give some of the major serotonergic pathways and their functions
Dorsal raphe nuclei → cortex, striatum
- Medial raphe nuclei → cortex, hippocampus
- Roles in:
o Mood
o Eating
o Sleep/dreaming
o Arousal
o Pain
o Aggression
- Define Ex-vivo and give some en-vivo imaging techniques
Ex-vivo: after death
- En-vivo:
o Contrast x-rays (cerebral angiography)
o Computer tomography (CT)
o MRI
o PET
- Give the basics of MRI
- Strong magnetic field cases H atoms to align by orientation – lattice structure
- Radio frequency pulse passed through scanner
o Atomic nuclei emit EM energy - Scanner detects energy radiated from each spatial location in the chamber
- Computer reconstruction image a 3D model
- Advantages
o No ionizing radiation exposure
o Excellent spatial resolution - Disadvantages
o Cost
o No ferrous metals
- Describe the hardware of MRI machines
- MRI magnet is supercooled by liquid helium – very powerful and expensive
- 60,000X Earth’s magnetic field
- Describe how Structural MRIs work
- Records a signal from each part of the brain by segmenting it into small voxels (less than 1mm^3)
- Signal returned from each voxel differs depending on the water content of the regions imaged
- Fatty tissues (e.g myelin sheath around white matter) are lower in water than grey matter
o CSF has greatest water content - Generates one high resolution depiction of brains structure and usually takes 7-10 minutes to record
- Describe how functional MRIs work
- Measures the amount of activation in each voxel (less than 2-3mm^3)
- Uses same principal as SMRI but condition of magnet and radio pulse are adjusted
- Oxyhaemoglobin and deoxyhaemoglobin in blood have differing paramagnetic qualities
- FMRI targets a reading which differs according to relative balance at each voxel throughout the brain
- Low resolution images generated every 2 seconds and we can passively monitor the brain or run experimentation manipulation
. Define and explain BOLD signal
- Blood oxygen dependent signal
- In fMRI measured variable is called:
- Neural activity is not measured directly, but BOLD fluctuates during an fMRI scan can tell us that particular regions required more oxygen at certain times so can infer brain function
- Compare SMRI to FMRI
SMRI
- High resolution (1mm voxels)
- Good contrast between tissue types and spatial resolution
- Suitable for evaluating structural abnormalities but one scan can take several minutes
FMRI
- Low resolution (2mm voxels)
- Many images (every 2 sec for 5 min)
- Indirect measure of neural activity
- Low resolution image but can be updated frequently to evaluate activity changes
- Define and explain voxel based morphology
- VBM is a structural analysis technique
- Used to investigate differences in brain anatomy – grey matter density
- Results highlight regions of the brain which show significant differences in density
- Explain how MRI is illustrated in writeups
- Structural and functional MRI results are typically presented on top of a recognisable brain structure
- Illustrated by overlaying on top of a sample structural image which provides spatial context
- In FMRI only coloured blob data actually comes from study in question
- Explain why statistical methods are needed in MRI studies
- Studies give a rich data set – typical resolution gives 6000 voxels per 2 second scan
- 20 min experiment gives 7.2 million data points
- At p<0.05 we can expect 360,000 false positives > risk of type 1 error
- Need to perform many comparisons – good MRI methods compensate for this with statistical corrections
- Give research findings for plasticity in mirror box therapy
- Guo (2016) – showed enhanced bilateral somatomotor activation in patients following MBT
- Michielson (2011) – only deep limbic areas demonstrated changes following MBT
- Give research findings for plasticity in stroke recovery
Rehme and Fink et al (2011) – patients recovery correlated with the ability of contralateral cortex to activate during movement of affected limb
- Ipsilateral activation represents maladaptive plasticity
- Give research findings for plasticity in CBT patients
CBT may impact on brain structure and function
- Siegle and Carter (2006) – depressed patients demonstrate disrupted emotional regulation
o Also show enhanced brain activity (FMRI) in amygdala during emotional stimuli
o Patients with greatest degree of amygdala dysfunction benefited from greatest improvement post CBT
- Give research findings for brain training
Meta-analyses questioned the benefits of brain training
- Likely to be specific to the trained task
- Kable et al (2017) Brain imaging shows no reputable changes in brain function for wider cognitive tasks after training
- Better evidence for brain benefits of physical exercise
- Give some examples of hypothalamic releasing and inhibitory hormones and their functions
- Thyrotropin-releasing hormone = TRH
o stimulates secretion of thyroid-stimulating hormone in anterior pituitary - Gonadotropin-releasing hormone = GnRH
o stimulates secretion of LH and FSH in anterior pituitary - Corticotropin-releasing hormone = CRH (from paraventricular nucleus)
o stimulates secretion of adrenocorticotropic hormone in anterior pituitary - Growth hormone-releasing hormone = GHRH
o stimulates secretion of growth hormone in anterior pituitary - Growth hormone-inhibitory hormone = somatostatin
o Inhibits secretion of growth hormone in anterior pituitary - Prolactin-inhibiting hormone – PIH (dopamine)
o inhibits secretion of prolactin in anterior pituitary
- Give some of the hormone types released by the anterior pituitary
AP contains cells of different types specialised for secretion of different pituitary hormones:
• somatotropes
• corticotropes
• thyrotropes
• gonadotropes
• lactotropes
- Give some examples of hormones and their functions released from the anterior pituitary
- Growth hormone – somatotropin – GH
o stimulates body growth, cell multiplication and Differentiation - Adrenocorticotropic hormone – ACTH
o stimulates secretion of glucocorticoids and androgens in adrenal cortex - Thyroid stimulating hormone – TSH
o stimulates secretion of thyroid hormones - Follicle-stimulating hormone – FSH
o stimulates development of ovarian follicles and spermatogenesis in testis - Luteinizing hormone – LH
o causes ovulation and stimulates the corpus luteum; stimulates secretion of estrogen and progesterone in ovaries; stimulates testosterone in testis - Prolactin – PRL
o stimulates milk secretion and development of mammary glands
- Give the role of glucocorticoids
Hormones that help to cope with stress (trauma, cold, infection, surgery, psychological stress)
• increase glucose level (for muscles)
• supports genesis of new glucose
• mobilises free fatty acids (energy)
• mobilises amino acids (new proteins?)
• decreases immune responses
• increases proteins in liver and plasma (healing of injured tissues?)
• decreases inflammation
• strengthening of catecholamine effects
- What are glucocorticoids regulated by?
ACTH
- Give research findings of dexamethasone
- (Low-dose) dexamethasone suppression test informs about the strength of HPA feedback
- Dexamethasone (a potent glucocorticoid) is applied and the cortisol level is recorded. If HPA feedback works, cortisol level would decrease
- Give 4 ways of evaluated stress using cortisol as a marker
- Resting state cortisol levels, taken from blood or saliva, usually on more than one time point during the day
- Post-stress task increases in cortisol secretion
- Cortisol awakening response – using the natural morning increase in cortisol secretion
- Low-dose dexamethasone suppression test
- Give some types of pain
- Pain can be produced by nociceptors (free nerve endings) responding to heat, cold, chemicals and pressure= nociceptive pain.
- Pain can be caused by a lesion or in jury of a nerve = neuropathic pain.
- Pain can be also caused by dysregulation within central nervous, hormonal or immune system = nociplastic pain.
- Explain the difference between acute and chronic pain and give some chronic pain conditions
- Acute pain: pain lasting hours/days/weeks (e.g toothache, injuries)
- Chronic pain: pain lasting more than 3 months
o Chronic pain syndromes:
Fibromyalgia – widespread pain in soft tissues
IBS – painful sensations in abdomen
• Nociplastic pain
Lower back pain
Headaches – migraine (unilateral, pulsatile pain)
Arthritis – pain in the joints due to wear and tear (osteoarthritis) or autoimmune response (rheumatoid
- Define and explain allostasis
- Allostasis: achieving stability through change
- Active process aimed at achieving balance.
- Examples: turbulence during a flight, focusing on a difficult task, bereavement, finding food in extreme conditions, imprisonment.
- Define allostatic load and overload
- Allostatic load – cumulative effects of allostatic state. It is a sum of responses
sub-serving fulfilment of daily routines plus extra demands. - Allostatic overload – wearing and tearing of allostatic resources if:
- the stress is too strong or prolonged (chronic)
- the coping resources diminish, e.g., due to unrelated disease or ageing
• Leads to a dysregulation of physiological systems including the brain and can lead to a chronic condition such as psychiatric disturbances, chronic fatigue syndrome or chronic pain.
• Dysregulation of the HPA and brain neurotransmitter systems due to allostatic overload is a probable cause of chronic diseases
- Describe the background of and findings of stress induced analgesia
- Based on observation of Col. Henry
o Beecher (1946) on soldiers sustaining major injuries in combat zones of WW2.
o 73% of wounded soldiers did not require any morphine. - “Stress-induced analgesia is a built-in mammalian pain suppression response that occurs during or following exposure to a stressful or fearful stimulus” (Butler and Finn, 2009).
- Physical exercise, acute fear or conditioned fear typically induce stress analgesia.
- SIA– part of fight or flight response, improves chances of survival
- Give the two models of stress-induced analgesia
- Unconditioned SIA – analgesia during concurrent exposure to an unconditioned stressor (e.g., cold, strenuous exercise, presence of predator, infantile isolation)
- Conditioned SIA (Fear-conditioned analgesia)– re-exposure to the context or environment at which the animal had experienced an unconditioned stressor
- Example: A rat exposed to forced swimming in cold water will show analgesia when brought again to the same water tank
- Give animal research findings of SIA
- Rodent animals selectively bred to show high or low pain suppression during stress reveal (see Butler and Finn, 2009):
- High-SIA animals show greater sensitivity to opioids (morphine) and their antagonists (naloxone) than low SIA animals.
- High-SIA animals have abundance of m-opioid receptors in their brains.
- Administration of naloxone blocks the SIA.
- Descending inhibition via the endogenous opioid system of spinal cord transmission of nociceptive impulsive is the main mechanism of SIA.
- Describe the neuronal pathways in SIA
- Glucocorticoid receptors are in abundance in prefrontal cortex, hippocampus, amygdala and hypothalamus =corticolimbic system
- Prefrontal cortex, hypothalamus, amygdala and hippocampus project to periaqueductal grey matter
- PAG sends impulses to rostro-ventromedial medulla (RVM) via endogenous opioids
- RVM activates nucleus coeruleus (noradrenergic), serotoninergic and cannabinoid (CB1) neurons to exert descending inhibition onto nociceptive processing in the spinal cord
- Explain how naloxone can attenuate SIA
Repetitive electrical stimuli to a peripheral nerve at the ankle under the stress showed a progressive increase in thresholds of the defensive twitch response. Naloxone reduced the stress-induced increase in pain thresholds.
- Do corticoids strengthen SIA?
Rats after hypophysectomy do not show SIA when swimming in cold water (Bodnar et al., 1979, in Butler and Finn, 2009).
• Administration of metyrapone (a drug that stimulates secretion of ACTH) caused increased SIA in rats during exposure to hot plate (pain stimulus) after swimming in cold water (stress) (Moussa et al., 1981).
• Systemic administration of dexamethasone which blocks the HPA reduced the strength of SIA in rats (see Butler and Finn, 2009).
- Give some of the neurotransmitter systems involved in SIA
Endogenous opioid peptides and their receptors (mu, kappa, delta)
• Systemic administration of naloxone and other antagonists of endogenous opioids attenuates SIA and FCA
• Administration of morphine strengthens SIA
• The opioid neurons exert their effects via GABA and glutamate
• GABA (gamma amino-butyric acid)
• Glutamate (NMDA receptors)
• Monoamines (noradrenaline, dopamine, serotonin)
• Cannabinoids (CB1 receptors)
- Describe and explain stress-induced hyperalgesia
Enhanced pain experience in the presence of stress
- SIH – when stressors are mild, prolonged, repetitive
- Examples of SIH-type stressors in animals:
- exposure to cold, immobilisation, air stress, holding, anticipation of aversive stimuli
- In humans: anxiety, bereavement, chronic illness, difficult tasks spanning over long periods of time, redundancy, marital problems
- Stressor time scale: days-weeks-months
- SIH likely in presence of a continuously heightened arousal
- Explain research findings of anxiety and pain
Anxiety increases while fear decreases pain
- Patients with joint pain (arthritis) showed stronger pain during stress periods, especially those with a history of depression. Zautra et al., J. Behav. Med., 2007
- Patients with abdominal pain (irritable bowel syndrome) show increases in pain and no recovery if they experience a life threatening stress (Bennett et al., 1998)
- School children reporting frequent harassment in school reported an increased occurrence of abdominal pain and headaches.
- Alfven et al., J. Psychosom. Res., 2008.
- Give research findings of links between CRPS and anxiety
A one-year prevalence in: chronic patients general population
depression 20.2% 9.3%
anxiety disorder 35.1 18.1%
- Types of anxiety: dysthymia (mild, prolonged state), post-traumatic stress disorder, social phobia, agoraphobia
- Chronic pain generates further stress : loss of life activities, job, income, loss of social contacts, marital problems
- Brain regions mediating the links among stress, anxiety and pain:
- Give some of the brain regions mediating the links among stress, anxiety and pain
- Brain regions mediating the links among stress, anxiety and pain:
o Amygdala
o Hippocampus
o Prefrontal cortex
o Hypothalamus
- Describe the relationship between the amygdala, cortisol and stress
- Amygdala has glucocorticoid and CRH receptors
- It shows increased activation in stress, fear or threat.
- Acute (1 day) and chronic (10 days) administration of corticosterone caused prolongation of dendrites in basolateral nc. of amygdala and increased in anxiety evaluated by the number of explorations made. (Mitra and Sapolsky, 2008).
- Similarly, acute (1 day) or chronic (10 day) immobilisation stress in rats caused increase in the number of dendritic spines in basolateral amygdala and increased anxiety – after 10 days (Mitra et al., 2005).
- Injection of corticosterone extends the size of dendrites in amygdala after 10 days
- Explain how glucocorticoids affect the hippocampus
- Has receptors for both mineralo- and glucorticoids.
- Glucocorticoids affect hippocampus in neurotoxic ways:
- Decreased neuronal firing, decreased LTP and increased LTD within
- minutes (non-genome effect).
- Further decreases in neuronal excitability later (genome effect).
- Impaired neurogenesis in the dentate gyrus of hippocampus which projects to
- amygdala.
- Loss of neurons, shrinkage of neuronal bodies and retraction of
- dendrites (these effects are reversible) in CA1-3 regions (learning, attention)
- (McEwen, 1999; McEwen, 2006; Lupien & McEwen, 1997)
- Give research findings of corticoids and stress on the hippocampus
- Stress causes degeneration in hippocampus
- Distressed monkeys in subordinate positions showed enlarged adrenal glands, stomach ulcers, and degenerative changes in hippocampus – reduced number of pyramidal neurons and reduced volume.
- This study illustrates further the degenerative changes in hippocampus due to chronic stress. The study analysed the structure and number of neurons in hippocampus in 8 monkeys living in captivity for years and were either in dominant or subdominant roles. A subdominant status was recognised by seeing many healed wounds from bites etc., basically a subordinate monkey was bullied by dominant monkeys.
- The degenerative changes in subdominant monkeys were much more abundant compared to dominant monkyes. Degeneration was mostly seen in cornu ammonis (CA) regions 1-4 and it was evidenced in the reduced number of pyramidal neurons and reduced volume of hippocampal subregions. There were no similar reductions outside hippocampus and subdominant monkeys also showed other changes signifying presence of stress, such as stomach ulcers and enlarged adrenal glands.
- Electrical stimulation of hippocampus decreases secretion of corticoids in humans
- Reduced volumes of hippocampi in chronic back patients and neuropathic pain patients
- Give research findings of the prefrontal cortex and HPA/stress
- Prefrontal cortex has abundance of glucocorticoid receptors.
- (e.g. Meaney and Aitken’s (1985) study in rats)
- Activity in vmPFC decreased during acute stress in healthy people (Sinha et al., 2016) and correlated negatively with cortisol increases.
- Daily injections of corticosterone for 3 weeks or 10 min/day restraint stress caused shortening of dendrites in PFC pyramidal neurons
o (Brown S.M., et al., Cerebral Cortex, 2005, 15: 1714-1725). - A number of cognitive deficits observed in rats and people after a long-term exposure to cortisol or stress (learning, decision making, slow extinction of fearful memories) suggesting evolutionarily based suppression of higher order cognitive and executive functions in stress
- Lesions in vmPFC increase ACTH and corticosterone during restraint stress in rats
o Results suggest an inhibitory role of vmPFC in HPA feedback loop during stress.
- Explain corticolimbic regulation of HPA
- Mineralocorticoid receptors respond
- to normal level of glucocorticoids,
- mainly in PFC and hippocampus.
- Glucocorticoid receptors respond to elevated levels of glucocorticoids,
- predominantly in hippocampus.
- Hippocampus projects glutamatergic neurons to inhibitory cells in PVN.
- Amygdala projects both glutamatergic and GABergic inputs to PVN.
- Give some sources of stress in chronic pain patients
• Stress may have existed before an injury or disease and contribute to
pain
• “wear and tear” precipitates chronic pain. Example: stress may
trigger migraine attacks which become chronic if stress continues
• Chronic pain itself adds to stress to create allostatic overload
• Sources of allostatic load in chronic pain: lack of sleep, depression,
anxiety, loss of many instrumental activities (sport, sex), financial
insecurity, potential loss of job or even break-up of family bonds.
- Pre-existing life stress:
- Dysregulation of HPA as a sign of allostatic overload
o Structural and functional brain vulnerabilities in regions controlling HPA
- Pain-related stress:
o Anxiety, depression, PTSD, lack of sleep – allostatic overload leading to dysregulation of HPA – chronic pain
- Explain who Mendel was and what he found
- Monk, initially performed experiments on mice before moving to pea plants
- Studied dichotomous traits and began his experiments by crossing the offspring of true breeding lines
- Define dichotomous traits and true-breeding lines
- Dichotomous traits: traits that occur in one form or the other, never in combination, e.g eye colour in humans or pea colour in peas.
- True breeding lines: breeding lines in which interbred members always produce offspring with the same trait, generation after generation e.g green seed or yellow seeds.
- Define phenotype and genotype
- Phenotype: an organism’s observable traits
- Genotype: the traits an organism can pass on to it’s offspring through its genetic material
- Describe Mendel’s theory of inheritance
- Mendel devised a theory to explain his results with four ideas
o Idea 1: There are two kinds of inherited factors for each dichotomous trait – today the inherited factor is called gene.
o Idea 2: Each organism possesses two genes for each of its dichotomous traits. In the case of widow’s peak the genes would be W and w
Alleles: two genes that control the same trait
Homozygous: organisms that possess two identical
o Idea 3: One of the two genes for each dichotomous trait dominates the other in heterozygous organisms.
o Idea 4: Dichotomous trait, each organism randomly inherits one of its father’s two factors and one of its mother’s two factors.
- Explain what chromosomes are
- Not until the early 20th century – genes were found to be located on chromosomes.
- Chromosomes occur in matched pairs (with ONE exception), and each species has a characteristic number of pairs in each of its body cells.
- 23 pairs.
- The two genes that control each trait are situated at the same location (loci), one on each chromosome of a particular pair.
- Describe sex chromosomes and sex-linked traits
- There is one exception to the rule that chromosomes always come in matched pairs.
- Traits that are influenced by genes on these chromosomes are sex linked.
- Traits that are controlled by genes on the sex chromosomes occur more frequently in one sex than the other.
- If the trait is dominant it will occur in females because females have twice the chance of receiving the X chromosome.
- Define gene, chromosome and genome
- Gene: one set of instructions for how to make one protein
- Chromosome: thousands of sets of instructions for how to make thousands of proteins
- Genome: All of the sets of instructions for how to make all of the proteins we need
- Define and describe meiosis
- The process of cell division that produces gametes is called meiosis.
- Chromosomes divide, and one chromosome of each pair goes to each of the two gametes that result from the cell division.
- Sperm + egg = zygote.
- As a result genetic recombination, each of the gametes that formed the zygote that developed into you contained chromosomes that were unique.
- In contrast to the meiotic creation of the gametes, all the cell division in the body occurs by mitosis.
- Describe chromosome structure and replication
- Each chromosome is a double stranded molecule of deoxyribonucleic acid (DNA).
- Each strand is a sequence of nucleotide bases attached to a chain of phosphate and deoxyribose.
- There are four bases.
- The two strands that compose each chromosome are coiled around each other and bonded together by the attraction of adenine for thymine and guanine for cytosine.
- Replication if a critical process of the DNA molecule. Without it, mitotic cell division would not be possible.
- The process needs to be accurate. Sometimes mistakes happen, they are a called mutations.
- In most cases, mutations disappear from the gene pool within a few generations because the organisms that inherit them are less fit.
- In rare instances, mutations increase fitness and in so doing contribute to rapid evolution.
- Mutations can be divided into two types:
- 1- Chromosome mutations: Change in chromosome number or chromosome structure : Down’s syndrome.
- 2- : Single-gene mutations: change in DNA structure within a particular gene: sickle cell disease.
- Describe the mechanism of gene expression
- Mechanism of gene expression:
- 1- Strand of DNA unravels
- 2- Transcription: Messenger RNA (mRNA) synthesised from DNA
- 3- mRNA leaves nucleus and attaches to ribosome in the cell’s cytoplasm
- 4- Translation: Ribosome synthesises protein according to 3-base sequences (codons)
- Describe the role of enhancers in gene expression
- Structural genes comprise only a SMALL portion of the chromosome.
- Enhancers are stretches of DNA whose function is to determine whether particular structural genes initiate the synthesis of proteins and at what rate.
- This determines how a cell will develop and how it will function once it reaches maturity.
- Proteins that bind to DNA and influence the extent to which genes are expressed are called transcription factors.
- Transcription factors control the enhancers. Transcription factors are influenced by signals received by the cell from its environment.
- Explain the human genome project
- Began in 1990.
- Its purpose was to compile a map of the sequence of all 3 billion bases in the human chromosomes.
- It was assumed that once the human genome was described it would be relatively straightforward to link variations in the genome to particular diseases and then develop treatments.
- The three major contributions of the project were:
- Development of new techniques to study DNA.
- The discovery that humans have a relatively small number of genes (20,000).
- Only about 2% of chromosome segments contain protein-coding genes.
- This discovery led to the rapid growth of epigenetics research
- Describe the growth of epigenetics research
- Epigenetics focuses on mechanisms that influence the expression of genes without changing the genes themselves.
- It refers to modifications of DNA and DNA packaging that alter the accessibility of DNA and potentially regulate gene expression WITHOUT changing the sequence of DNA itself.
- Assumed to be the means by which a small number of genes are able to orchestrate the development of humans in all their complexity.
- It is focuses on the role of experiences in genetic expression.
- Many epigenetics mechanisms have been discovered, two of the most widely studied are:
o DNA methylation
o Histone remodelling
- Define and explain DNA methylation
- DNAm is most commonly studied in human populations for two major reasons:
- 1- It is easily quantifiable, and relatively stable.
- 2- Does not require complex processing of samples after collection.
- One of the main roles of DNAm is in cellular differentiation. As stem cells divide and gradually differentiate into specific cell types, DNAm patterns become increasingly cell type specific.
- This explains how cells with the same genetic sequence, such as neurons and white blood cells, have very different functions.
- Thus in contrast to genetic information, DNAm is highly tissue specific.
- Define and explain epigenetic mechanisms
- These mechanism allows for the cell-to-cell transmission of epigenetic patterns associated with the cell’s past exposures —they create a form of cellular memory that can be passed along to daughter cells.
- It is these patterns that can be detected in studies examining associations between current DNAm and exposures or events in the past.
- Describe and define epigenetic inheritance
- We used to think that a new embryo’s epigenome was completely erased and rebuilt from scratch.
- Reprogramming is important because eggs and sperm develop from specialised cells with stable gene expression profiles.
- In other words, their genetic information is marked with epigenetic tags. Before the new organism can grow into a healthy embryo, the epigenetic tags must be erased.
- The belief was that a new embryo’s epigenome had to be completely erased and rebuilt from scratch.
- This needs to be done in order for an embryo to make every type of cell in the body.
- However this is not entirely true. Some epigenetic tags remain in place as genetic information passes from generation to generation, a process called epigenetic inheritance.
- Epigenetic inheritance is an unconventional finding. It goes against the idea that inheritance happens only through the DNA code that passes from parent to offspring.
- It means that a parent’s experiences, in the form of epigenetic tags, can be passed down to future generations.
- In mammals, about 1% of genes escape epigenetic reprogramming through a process called imprinting
- Define and explain transgenerational epigenetics
- These mechanisms can be induced by particular experiences such as neural activity, hormonal state, changes to the environment.
- These changes can last a lifetime.
- The interesting question is: Can those experience-induced changes be passed to your offspring?
- Yes, it was first observed in plants but now also evidenced in mammals: Mice trained to associate electric shock to odour. This effect is passed to offspring.
- Explain why making a case for epigenetic inheritance in humans is challenging
- Making a case for epigenetic inheritance in humans remains especially challenging because:
- Humans have long life spans, making it time consuming to track multiple generations.
- Humans have greater genetic diversity than laboratory strains of animals, making it difficult to rule out genetic differences.
- Ethical considerations limit the amount of experimental manipulation that can take place.
- Describe research findings of transgenerational epigenetics in humans
- Geneticists analysed 200 years worth of harvest records from Överkalix, a small town in Sweden.
- They saw a connection between food availability (large or small harvests) in one generation and the incidence of diabetes and heart disease in later generations.
- The amount of food a grandfather had to eat between the ages of 9 and 12 was especially important. This is when boys go through the slow growth period (SGP), and form the cells that will give rise to sperm.
- Grandsons of Överkalix boys who had experienced a “feast” season when they were just pre-puberty died (often of diabetes) on average six years earlier than the grandsons of Överkalix boys who had been exposed to a famine season during the same pre-puberty window.
- When a statistical model controlled for socioeconomic factors, the difference in lifespan became 32 years, all dependent simply on whether a boy’s grandfather had experienced one single season of starvation or gluttony just before puberty.
- As sperm cells form, the epigenome is copied along with the DNA.
- Since the building blocks for the epigenome come from the food a boy eats, his diet could impact how faithfully the epigenome is copied.
- The epigenome may represent a snapshot of the boy’s environment that can pass through the sperm to future generations.
- Describe twin study findings of epigenetic effects
- Twin studies
- Fraga et al 2005: tissue samples from 40 pairs of MZ twins, age range 3-74y:
- Screened tissues for DNA methylation and histone modifications.
- MZ twins were epigenetically indistinguishable in early life but differences accumulated as they aged
- Give research findings of the interaction of genetic factors and experience
- Selective breeding of “maze bright” and “maze dull” rats
- Early psychologists assumed that behaviour develops largely through learning.
- In 1934 Robert Tryon (Behavioural psychologist) trained a large heterogenous group of laboratory rats to run a complex maze. The rats received a food reward when they reached the goal box.
- Then mated the females and males that least frequently entered incorrect alleys during training : maze bright, and bred the females and males that most frequently entered incorrect alleys during training: maze dull.
- Then accessed the performance of offspring and kept mating brightest and dullest for 21 generations.
- By the eighth generation, there was almost no overlap in the maze learning performance of the two groups.
- Describe the findings of the Minnesota study of twins reared apart
- In the development of individuals the effects of genes and experience are inseparable.
- In the development of differences among individuals they are separable.
- How would you assess the relative contributions of genes and experience in the development of individual differences in psychological attributes:
- Study individuals of known genetic similarity
- Adoption studies: the most extensive study is the Minnesota Study of Twins Reared Apart
- 59 pairs on monozygotic and 47 pairs of dizygotic twins who had been reared apart and as many pairs that had not.
- Age range: 18-69 years.
- Each twin was brought to University of Minnesota for approximately 50 hours of testing: intelligence and personality.
- In general adult monozygotic twins were more similar to one another on ALL dimensions than dizygotic twins regardless how they were reared.
- This takes us to the contribution of genetic variation to this study.
- Heritability estimate: numerical estimate of the proportion of variability that occurred in a particular trait in a particular study as a result of genetic variation.
- Define and explain heritability estimate
- Heritability estimate: Numerical estimate of the proportion of variability that occurred in a particular trait in a particular study as a result of genetic variation.
- Numerical estimate (between 0-1). Sometimes represented as percentages (100% would be 1).
- Basically you MUST have VARIATION in a trait to be able to get a value above 0
- This means that:
- A) It cannot be studied in one individual
- B) The trait that you are exploring has to show variability in the population
- The estimate depends upon which population you examine.
- Numerical estimate of the proportion of variability that occurred in a particular trait in a particular study as a result of genetic variation
- The magnitude of a study’s heritability estimate depends on the amount of genetic and environmental variation from which it was calculated and it CANNOT be applied to other situations.
- Give research findings of twin studies on the effect of experience on heritability
Twin studies on the effect of experience on heritability
- Turkheimer et al 2003: heritability of intelligence in upper-middle class 75%
- Heritability intelligence in 7y old twins: families from low SE status: 10% and high SE status 70%
- This effect was replicated and extended to other age groups
- Implications: intelligence develops from the interaction of genes and experience, one can inherit the potential to be of superior intelligence but this potential is rarely realised in a poverty stricken environment
- This has implications for the programs to help to develop individuals in low SE status.
Describe the origin of species
Fusion with Mendelian genetics, and then, by considering Natural Selection at the level of the gene, Bill Hamilton developed Inclusive Fitness Theory
The biological problem of altruism explained for related individuals: Robert Trivers
The flip side of inclusive fitness theory: one form of brood reduction?
Brain and behavioural complexity: some behavioral ecology
Back to the problem of altruism: unrelated individuals
The social brain hypothesis
Some puzzles for your social brains
Contemporary efforts to extend the modern synthesis: more puzzles for your brains
Describe and explain natural selection
Natural selection is one of the central mechanisms of evolutionary change and is the process responsible for the evolution of adaptive features.
Without a working knowledge of natural selection, it is impossible to understand how or why living things have come to exhibit their diversity and complexity.
An understanding of natural selection also is becoming increasingly relevant in practical contexts, including medicine, agriculture, and resource management.
Unfortunately, studies indicate that natural selection is generally very poorly understood, even among many individuals with postsecondary biological education.
This paper* provides an overview of the basic process of natural selection, discusses the extent and possible causes of misunderstandings of the process, and presents a review of the most common misconceptions that must be corrected before a functional understanding of natural selection and adaptive evolution can be achieved.
Fundamental logic of D’s NS merged with Mendelism -> modern synthesis
Selection at level of the gene –
“Good of the species” argument – even used at first by ethologists - fallacious
Population thinking – alternative alleles in a population
Social living - benefits mostly lowered risk of predation but also shared info in foraging and more complex instances of co-operation – understandable in win-win situation. But what if one individual, in helping another, appears to lose out in respect of its own fitness?
We saw an example of helpers at the nest – if they do really help – sometimes better than fruitless independent attempts, given it is their own parents they are helping
Bill Hamilton – inclusive fitness theory – how behaviour of an individual may impact upon close relatives –
rb-c < 0
Where r = coefficient of relationship/kinship, b= benefit in terms of Darwinian fitness to recipient, c= cost in same terms to donor
Social insects extreme case of altruism – sterile castes – but all honeybee workers daughters of the queen – sometimes workers lay eggs which are not fertilised à males (drones)
Haplodiploid inheritance system – one set of chromosomes males – double set females – since large group of female workers may all have been fathered by same drone they receive identical set of chromosomes from father – choice between two sets from queen – sterile sisters related to each other by r = ¾
Termites have normal inheritance but male as well as female workers. See Gardner & Ross 2013 (More on termites in you-tube clips with the late John Maynard Smith)
Describe the flipside of inclusive fitness theory
Of course in social living you get many conflicts, and modes of resolving these, often without fatal damage. These are to be expected between unrelated individuals…
Kittiwakes typically have two chicks ± 1
How many chicks should you have?
May adjust projected brood size to prevailing conditions but what if conditions change? (Pettifor, Perrins, & McCleery, 2001)
Can’t easily add, but what about brood reduction?
Describe and explain reciprocal altruism
Here, unlike kin selection in the Hamilton equation the donor and recipient of an altruistic act need not be related. The cost should be small in relation to the benefit.
In one encounter the altruist may bear a small cost if, in similar circumstances likely to arise in the future in which the roles of donor and recipient were reversed: a small cost now is worth incurring if it increased the likelihood of a greater benefit later.
This is a situation highly susceptible to cheating, of two kinds:-
Gross cheating: the beneficiary of the first altruistic event simply does not reciprocate in comparable situations where the potential roles are reversed
Subtle cheating: all sorts of ways in which a beneficiary reciprocates in a sub-standard way, not giving as much now as was received before
Describe and explain cheater detection
can become very valuable since it enables withdrawal from costly contracts, and honing this ability in ever more subtle ways may constitute a powerful evolutionary trend in relevant cognitive “machinery” in the human case
Wason’s paradox with the cards is simply a demanding intellectual puzzle, the failure to solve which (by the majority of people) is reminiscent of Kahneman’s “fast” thinking.
Where essentially the same problem is perceived in a social context more people get it right.
Similar superiority in social contexts characterizes performance on several Piagetian tasks
Describe and explain comparative cognition
What drives expanding brains and behavioural repertoires in phylogeny?
Complex social relations?
Robin Dunbar:The social brain hypothesis
Demonstrated that the neocortical ratio in the brains of various species of primates* increased with increasing size of the social group in which members of a species typically lived.
This principle did not apply in the same way to birds** however, where intensive parental care
Describe and explain foraging
Optimal foraging: the problem of when to leave a dwindling resource patch and move on to a fresh one.
A natural example would be berry bushes. As you pick them from a particular bush, the individual berries become harder and harder to find. When should you quit and begin a search for a fresh bush (which may be some way away)?
The optimal time spent in a patch is given by the tangent to the resource intake curve that departs from the expected transit time value.
Any other line crossing the resource intake curve has a shallower slope and thus a sub-optimal resource intake rate.
Describe what happens during the fight or flight response
Muscles need energy – rather than stored away for future project.
Rapid mobilisation – inhibition of storage.
Glucose, proteins, fats pour out of fat cells, liver, and muscles into bloodstream and muscles to save your neck.
Heart rate, blood pressure, and breathing rate increase, all to transport nutrients and O2 at greater rates.
Digestion, growth and tissue repair, sexual drive, immunity – all inhibited. Concentrate on task in hand.
Pain is blunted, cognition sharpened.
Describe the order of events in the fight or flight response
Muscles need energy – rather than stored away for future project.
Rapid mobilisation – inhibition of storage.
Glucose, proteins, fats pour out of fat cells, liver, and muscles into bloodstream and muscles to save your neck.
Heart rate, blood pressure, and breathing rate increase, all to transport nutrients and O2 at greater rates.
Digestion, growth and tissue repair, sexual drive, immunity – all inhibited. Concentrate on task in hand.
Pain is blunted, cognition sharpened.
Distress signal to the hypothalamus (command centre).
Sympathetic nervous system – triggers the fight-or-flight response
Adrenal glands pump epinephrine and norepinephrine into bloodstream
Heart beats faster, pushing blood to the muscles, heart, other vital organs
Epinephrine - release of blood sugar (glucose) and fats – these supply working muscle.
Phase 2 starts - HPA axis [hypothalamus, pituitary gland, adrenal glands.
If the brain continues to perceive something as dangerous, the hypothalamus releases corticotropin-releasing hormone (CRH), which travels to the pituitary gland, triggering the release of adrenocorticotropic hormone (ACTH). This hormone travels to the adrenal glands, prompting them to release cortisol. The body thus stays revved up and on high alert.
Parasympathetic nervous system — the “brake”.
Define and explain allostatic load
Allostasis is an essential to maintaining homeostasis.
Allostatic systems are:
Overworked
Fail to shut off after stressful occasions
Fail to respond adequately to challenge
Other systems have to react.
Cardiovascular system, metabolic machinery, immune system and central nervous system – large range of activity (allostasis).
Most useful when they can be rapidly mobilised and turn off suddenly (when not needed).
Inability to activate is also a problem – doesn’t offer protection afforded by the system.
Give the four conditions that lead to allostatic load
Four conditions that lead to allostatic load:
Repeated “hits” from multiple novel stressors
Lack of adaptation
Prolonged response due to delayed shut down
Inadequate response that leads to compensatory hyperactivity of other mediators, e.g., inadequate secretion of glucocorticoid, resulting in increased levels of cytokines that are normally counter regulated by glucocorticoids).
Give some examples of health effects of long-term stress
Survivors of concentration camps (long-term stress) – poorer health than others further down the line.
Subway train drivers more likely to suffer illness after tragedy.
Air traffic controllers – especially busy airports greater incidence of high blood pressure.
Describe the effects of stress on the cardiovascular system
HR = 180/120 not suffering from high BP. Saving your life.
HR = 180/120 every time you’re in traffic. Stress induced hypertension.
Damage CV system over time
More complex.
Tube (arteries). Fluid moving through tube.
Fluid moving with force (HBP).
Fluid turbulence pounding on walls of blood vessels.
Pitting, scaring, tearing - inflammation. Glucose, cholesterol and fat want to glam onto.
Describe the transactional model

Describe the effect of personality on heart health
Type A behaviour (hotheaded, quick decisions) pattern associated with increased prevalence of clinical coronary heart disease.
Describe the effect of stress on child growth
Established a long time age (1947).
Do it tomorrow, do it tomorrow.
Children are long-term building projects.
Limited growth hormone in circulation.
Return to normal levels once removed from stressful environment.
Saenger et al – Somatomedin and growth hormone in psychosocial dwarfism
Child assigned to nurse - became attached.
Stress dwarfism - not a problem of insufficient food.
Eating more at the time he entered the hospital than a few months later, when his growth resumed.
Calcium deposit related to proximity to loved one
Describe the link between ulcers and stress
Psychological causal role. Gastric ulcers one of the first classified as psychosomatic.
However, are these caused by bacteria; Helicopter pylori?
Helicopter pylori alone insufficient to produce ulcer (see Plummer et al. 2014; Testerman & Morris, 2014).
Antibiotics and psychological treatments improve gastric ulcers; so stress must be important?
Also, stomach wall more damaged from Helicopter pylori in presence of stress.
More common in people living in stress situations + evidence in laboratory rats.
Describe and explain psychoimmunology
Stress can increase susceptibility to infectious disease. Led to a new field (1970’s).
Emotion, immunity and disease (Soloman & Moss, 1964)
Psycho – psychological processes
Neuro – neuroendocrine system (i.e., nervous and hormonal systems)
Immunology – immune system
Interaction between nervous and immune systems and relations with behaviour + health
Stress increases the secretion of glucocorticoids – these hormones directly suppress immune system.
Depends on the kind of stress (caring for elderly or unemployment
Give research examples of adverse effects of healing
Slowing of wound healing by psychological stress
Puncture biopsy wounds in participants (harmless procedure).
Long-term carers for those with Alzheimer’s disease.
Control group – same age and income.
Carers took longer to recover
• Hostile marital interactions, proinflammatory cytokine production and wound healing
Couples’ blister wounds healed more slowly following marital conflicts than after social support interactions
Psychological stress and susceptibility to the common cold
Given nasal drops containing cold viruses.
More likely to develop colds if reported stressful event and felt threatened/out of control.
Psychological stress was associated in a dose-response way with an increased risk of acute infectious respiratory illness.
describe and explain conditioning of the immune system
Ader and Cohen
While studying taste aversion in mice, Ader and Cohen discover that the immune system can be conditioned in the same way Pavlov’s dogs learned to salivate in response to a bell.
In their study, mice prone to Lupus are offered a saccharin-flavoured drink at the same time they are injected with a potent immune-supressing drug to treat their Lupus. Once the association is learned, the taste alone (with no injection at all) reduces inflammation and symptoms of Lupus almost as much as the drug alone.
Explain the role of mediators on stress
Such as alcohol, comfort eating, smoking, sleep
Less likely to participate in health enhancing behaviours.
Sleep is an important component of human homeostasis. Frequently being in a heightened state of alertness can delay the onset of sleep and cause anxious thoughts to occur at night. Insufficient sleep can then cause further stress.
The majority of the literature finds that the experience of stress impairs efforts to be physically active. This behaviour would likely result stress – vicious circle.
Explain how physical activity can have an effect on stress and mood
Physical self worth
Self-esteem
Mastering new tasks
Personal control (sense)
Time away from –ve place
Social interaction
Social support
Reduced social isolation
Mood
Happiness
Feel good factor
Describe social determinants of health
Not just about lifestyle behaviours.
Unemployment, low-paid work, inadequate benefit entitlements, and lack of affordable housing. “ Causes of the causes”
A negative cycle can exist between poverty and health.
Unemployment and poverty contribute to poor mental and physical health, which in turn makes it more difficult to find work.
explain the links between poverty, stress and ill health
Income, occupation, housing conditions, education.
Manual labour and a greater risk of work-related accidents.
Two/three exhausting jobs.
Chronic sleep deprivation?
Walk to work [no choice], launderette, supermarket [heavy groceries].
Can’t buy new mattress/hot water.
Lack of control, lack of predictability. Career spent taking orders/temporary work [precariat].
Unemployment – predictability - will money stretch?
No resources in reserve [no buffer – reactive. Loan shark].
Marked lack of outlets [mediating factors; exercise, diet, holiday].
Crime riddled neighbourhood with few amenities.
Lack of social support [time to mix with others].
Describe some alternate theories of stress
Diathesis-stress model – interacting factors jointly determine susceptibility to stress and illness.
Predisposing factors (person’s vulnerability; genetic)
Precipitating factors (environmental).
Tend-and-befriend theory – women are more likely than men to display a social response during stressful situations.
Protecting offspring (tending)
Seeking others for mutual defense (befriending).
Men (fight-flight; hunting defending against danger)
Women (foraging food and child care)
Define the stress continuum
Chronic stress occurs if buffers not available
Anxiety becomes depression if stress is chronic
Levels of
Dopamine
Glucocorticoids
Epinephrine
Change accordingly
Rats can feel pleasure in mastering pressing a lever to avoid a shock
Increase in dopamine levels
Dopamine levels decrease when pressing the lever no longer avoids a shock
Heightened levels of glucocorticoids and epinephrine
As coping proves elusive, hypervigilance is replaced by passivity and depression – learned helplessness
Heightened levels of glucocorticoids and epinephrine
Describe the link between mental health and income
Most countries have experiences a profound increase of income inequality in recent decades
Greatest risk of depression in populations with higher income inequality relative to populations with lower inequality
Subground effect
Social capital hypothesis: higher levels of income inequality increase status differentials between individuals, reduce social mixing across groups, thereby reducing levels of interpersonal trust
Quality of social relationships not the amount of funds allocated to health systems/care
Describe how to measure behavioural changes in sleep
Electroencephalogram (EEG) – electrodes attached to the scalp record electrical activity of the brain
Electromyogram (EMG) – electrodes attached to the chin monitor muscle activity
Electro-oculogram (EOG) – monitors eye movements
describe the changes in brain activity during sleep (awake to stage 2)

describe the changes in brain activity during sleep (stage 3 to REM sleep)

Describe the types of brain activity during sleep
Awake: Alpha activity, beta activity
Stage 1 sleep: Theta activity,
Stage 2 sleep: Spindle, K complex
Stage 3: Delta activity
Stage 4: Over 50% delta activity
REM: theta activity, beta activity (most similar to awake EEG)

Describe brainwave cycles during sleep
Along the night the proportion of REM increases and NREM decreases
REM periods increase in length and frequency towards the morning
Deep sleep only present in first and second cycles
Describe the finding of brain areas involved in sleep regulation
Discovered in the early 20th century
Baron Constantin Von Economo (Vienese neurologist)
Patients with a viral disease called encephalitis letargica (epidemic between 1915-26. Affected over 5 million people and 1 million died
Although it was first officially recognised as a separate disease entity in 1917, there are several historical epidemics that resembled encephalitis lethargica, including the English sweats (England, 1529), mal mazzuco (Italy, 1597), Kriebelkrankheit (Germany, 1672–75), Rafania (Sweden, 1754–57), and nona (Italy, 1890–91).
The last epidemic most likely started in Romania
Disease disappeared a decade after and the cause was never identified: virus, toxic or autoinmmune
Some sporadic cases still occur.
Describe Von Economo’s encephalitis
Damage to anterior hypothalamus or posterior hypothalamus
Excessive sleep: damage in the posterior hypothalamus
A minority of patients had difficulty sleeping: Damage in the anterior hypothalamus
Name some of the areas involved in sleep regulation
Anterior hypothalamus
Posterior hypothalamus
Reticular formation
Nuclei in caudal reticular formation
Describe the role of the reticular formation in sleep and how it was found
In 1937 Bremer experimented in cats severing the brain stem in several areas
Between the superior and inferior colliculi (Cerveau isolé “isolated forebrain”) resulting in continuous SWS
Transsection caudal to the colliculi, (Encéphale isolé “isolated brain”) resulting in normal sleep cycle
Wakefulness depends on the function of the reticular formation, or “reticular activating system”
Describe the role of nuclei in the caudal reticular formation in sleep
Similarities between REM and wakefulness suggest that the same brain area might be involved in controlling both.
REM sleep is controlled by nuclei in the caudal reticular formation, each controlling a different aspect of REM
Atonia (loss of muscle tone)
Rapid eye movements
Cardiorespiratory changes
Describe neurochemical control of sleep
Sleep is regulated – suggesting a monitoring mechanism
Do sleep-promoting substances or wakefulness promoting substances exist?
Substances do not appear to circulate in the blood
Controlled by chemicals that are produced and act within the brain
Because REM and NREM sleep are regulated independently there might be two substances
Describe the role of adenosine in sleep
Astrocytes maintain a small stock of nutrients in the form of glycogen
In times of increased brain activity this glycogen in converted into glucose to fuel neurones
A decrease on glycogen (energy depletion) increases extracellular adenosine
Adenosine inhibits neural activity
Adenosine promotes sleep
During SWS neurones in the brain rest and the astrocytes renew their stock of glycogen
If wakefulness is prolonged even more adenosine accumulates, adenosine inhibits neural activity producing the cognitive and emotional effects seen during sleep deprivation
Coffee is an adenosine antagonist
Describe the neurochemical control of arousal
Acetylcholine (Ach)
Noradrenaline (Norepinephrine)
Serotonin (5-HT)
Histamine
Orexin (Hypocretin)
Describe the role of acetylcholine
One of the most important neurotransmitters in arousal
Antagonists decrease EEG arousal and agonists increase it
Two groups of neurones : Pons and forebrain
Levels highest in striatum, hippocampus and cortex in active animals
Electrical stimulation of pons increases release by 350% and activates cortex
Describe the role of noradrenaline in sleep
Located in the locus coeruleus of the pons
Noradrenaline agonist such as amphetamines produce arousal and sleeplessness
Activation of LC neurones increases vigilance
Describe the role of serotonin in sleep
Produced by raphe nuclei (located in the pontine and medulary regions of the reticular formation)
Stimulation causes movement and arousal
One specific contribution of serotonergic neurones to activation is facilitation of continuous, automatic movements such as:
Pacing
Chewing
Grooming
Serotonergic neurones are involved in facilitating ongoing activities and suppressing the processing of sensory information
This prevents reactions that might disrupt the ongoing activities
WHEN the animal engages in orienting responses the activity of serotonergic neurones decrease
Describe the role of histamine in sleep
Histaminergic neurones are in tuberomammillary nucleus of the hypothalamus
Directly and indirectly increases cortical activity and arousal
Indirect actions via acetylcholine neurones
Activity is high during waking and low during sleep
Blocking activity of histamine neurones increases sleep
New antihistamines do not cause drowsiness
because they do not cross the blood brain barrier
new antihistamines are non-drowsy as they don’t cross the blood-brain barrier
Describe the role of Orexin in sleep
Orexin neurones (only 7000) are located in lateral hypothalamus
Project to almost all areas of the brain: cortex and areas relevant to all of the previous neurotransmitters
Orexins have a wakefulness promoting effect
Active during wakefulness and inactive during sleep
Narcolepsy has been associated to problems with orexin signalling.
degeneration of orexin neuron in humans and hereditary absence of orexin receptors in dogs
Describe the homeostatic control of slow-wave sleep
If we go without sleep for a long time we eventually become sleepy
Once we sleep, we will be likely to sleep longer than usual
This control of sleep is homeostatic
The control of sleep is homeostatic in nature and follows the principles that regulate our eating and drinking
Controlled primarily by adenosine
Describe the allostatic control of slow wave sleep
Under some circumstances is important to stay awake (i.e: dehydrated). This control of sleep is allostatic in nature
This refers to reactions to stressful events in the environment (danger, lack of water)
This overrides the homeostatic control (remember the lethargic encephalitis patients?
Mediated by hormonal and neural responses to stressful situations and neuropeptides involved in hunger and thirst
Describe the control of slow wave sleep by circadian factors
They tend to restrict our period of sleep to a particular portion of the day
Describe the neurochemical control of slow wave sleep
When we are awake and alert, most of our neurones, especially in the forebrain are active
Anterior hypothalamus now called preoptic area
The ventrolateral preoptic area (VLPA) contains neurones that inhibit the arousal neurones
Either the VLPA area is inhibited, or it is inhibiting.
When the VLPA neurones (sleep neurones) become active they supress the activity of the arousal neurones
We fall asleep
What happens if you destroy the VLPA?
Total insomnia in rats
Animals fall into a coma and die after 3 days
The majority of sleep neurones are located in the VLPA
They secrete GABA and send axons to brain regions involved in arousal
Neurones in VLPA are inhibited by histamine, noradrenalin and serotonin
Describe how orexin contributes to the waking state
Orexin stabilises and tips the system towards the waking state
Mutated orexin gene: same amount of sleep and waking but a lot more transitions between asleep and awake
During the day orexin neurones receive excitatory input from biological clock that controls circadian rhythms
Also from brain areas that monitor the animal’s nutritional state: What would you expect here?
Hunger signals _____ orexigenic neurones
Satiety signals______orexigenic neurones
Accumulation of adenosine overcomes excitatory input from other areas and sleep happens
Conclusion: orexigenic neurones are involved in all three factors that control sleep and wakefulness: homeostatic, allostatic and circadian
Describe the neurochemical control of REM sleep
Brain metabolism during REM sleep is as high as in wakefulness
REM sleep is also controlled by a flip-flop mechanism
The sleep waking flip-flop determines when we wake and when we sleep
Once we fall asleep the REM flip-flip flop controls the SWS/REM cycles
Acetylcholine neurones in the pons fire at high rate during REM (similar to wakefulness)
They are responsible for cerebral activation during wakefulness and REM sleep
During waking the REM off receives excitatory input from OREXIN, noradrenergic and serotonergic neurones tipping the switch to the off state
Excitatory activity to REM off decreases, this tips the switch to REM on
Emotional stimuli activate the amygdala which in turn flips the REM switch on
Describe the circadian control of sleep
Our daily pattern of sleep and wakefullness is regulated around a 24 hr cycle
These cycles are called circadian rhythms
Circadian ryhthms are kept on schedule by temporal cues in the environment
Temporal cues = zeitgebers
Most important zeitgeber = daily cycle of light and dark
Give examples of cognitive and hormonal zeitgebers
Time – a cognitive zeitgeber
Clocks, work and travel schedules place demands on the body to remain alert for certain tasks and social events.
Cognitive pressure to stay on schedule.
Melatonin – a hormonal zeitgeber
Melatonin is released in a daily light-sensitive cycle
Levels of melatonin begin climbing after dark and ebb after dawn.
Melatonin induced drowsiness
Melatonin-deficient insomnia
Blind people lacking synchronising effects of light-dark cycle
Explain free running circadian sleep-wake cycles
Zeitgebers entrain circadian rhythms
Circadian rhythms persist when devoid from day-light cycle
Rhythms = free-running rhythms
Duration = free-running period
Constant illumination = 24.2 hours
Constant darkness = 25 hours
Describe and explain the effects jet lag
Zeitgebers are
Accelerated (phase advance) during east bound flights (going to Thailand).
Delayed (phase delay) during west bound flight (going to America).
Results in sleep disturbances, fatigue, mood changes, deficits on tests of physical and cognitive performance.
Temporary problem treatable with light exposure or melatonin administration.
Describe and explain the effects of shift work
Similar to jet lag (exposure to light/dark out of phase)
Long lasting condition
1 day for circardian rhythm to adapt to 1 hour change in light/dark cycle
Shift work disorder being recognised as formal sleep disorder
Related to fatigue, poor performance and poor memory
Risk of other ongoing health problems eg CVD, depression, diabetes
Measures to mitigate effects are available but rarely adopted
Describe insomnia
Affects 25% of the population occasionally and 9% regularly
Defined in relation to a person’s particular sleep needs
Sleeping medication is one of the main causes (drug dependency insomnia)
Sleep apnea (causes insomnia) – inability to sleep and breath and the same time
Restless leg syndrome
Describe and explain NREM parasomnias
Confusional arousals:
Disoriented behaviour during arousal from NREM sleep
Last for seconds to minutes
Often accompanied by vocalisations in infants and toddlers
Poor recall of events the following day.
Sleepwalking:
Up 17% in children and 4% of adult population
Combination of moving with the persistence of impaired consciousness
Linked with anxiety, fatigue, alcohol, medications and mental disorders
Sleep terrors:
The most disruptive arousal disorder
Episodes of intense fear initiated by a sudden cry or loud screams
Accompanied by increased autonomic nervous system activity.
Prevalent in those who suffer from PTSD
Sleep related eating disorder:
Combination of a parasomnia and an eating disorder
Sleepwalking that includes behaviours connected to a person’s conscious wishes
Describe and explain REM parasomnias
REM Sleeping behaviour disorder
Loss of normal atonia: dream enactment behaviour.
More frequent in males >50years old.
Associated to neurodegenerative disorders (Parkinson’s, dementia).
Some genetic component.
Treated with clonazepam, a benzodiazepine.
Isolated sleep paralysis
Paralysis is maintained after waking from REM sleep.
Can also occur when falling asleep.
Fully aware of what is happening
Lasts for seconds to minutes
Sometimes accompanied by hallucinations
First appears during teens but most often in 20s and 30s
Describe and explain narcolepsy
Characterised by four symptoms:
Sleep attacks – overwhelming urge to sleep for a few minutes
Cataplexy – sudden paralysis during which a person remains conscious
Sleep paralysis – similar to cataplexy but occurs just before sleep and on waking
Hypnagogic hallucinations – dreams that occur during periods of sleep paralysis
Describe the link between neurochemical control and narcolepsy
Narcolepsy is associated with
a lack of orexins
a gene coding for an immune factor
This suggest narcolepsy in an autoimmune disease
Streptococcus bacteria appears to be the trigger for the autoimmune attack
Occurrence of events at a vulnerable age (childhood) make an immune attack on the orexin system more likely
Describe the relationship between sleep and memory
Sleep is a period where the brain consolidates memories.
Areas of the brain – the hippocampus, neocortex and amygdala – that are important in memory are active during sleep
The quantity and quality of sleep affect a person’s ability to remember
Sleep deprivation impairs attention and working (short term) memory, but it also affects as long-term memory and decision-making.
Hypersomnia (typically results in poor sleep quality) is linked with poor memory
Describe the effect of sleep deprivation on memory
Researchers believe that sleep affects learning and memory in two ways:
Lack of sleep impairs the ability to focus and learn effectively
Sleep is necessary to consolidate a memory so that it can be recalled in the future
How might sleep affect memory?
Blood flow problems could hinder brain functioning
Beta amyloid deposits are linked to decline in memory and risk of dementia
Name some of the most important brain areas for memory
- Hippocampus
- Neocortex
- Amygdala
are particularly important in the storage of memories
Describe the role of the hippocampus on memory
HIPPOCAMPUS
Where episodic memories are formed and indexed for later access
CASE STUDY
Henry Molaison, 1953
Hippocampus surgically removed
Only able to form episodic memories lasting a matter of minutes
Unable to permanently store new information
Could remember events that occurred before surgery
Conclusion:
Hippocampus is the sight for laying down memory
It is not the site of permanent storage
FMRI, HIPPOCAMPUS AND MEMORY
Sleep deprived students asked to view and remember images
Performed as much as 40% worse on recall two days later
Activity was significantly decreased in the hippocampus
Analogous to a lesion on the hippocampus
Memory impairment rather than concentration
Memories ‘jammed’ in the hippocampus
Describe the role of the neocortex in memory
Largest part of the cerebral cortex
Involved in higher functions
Important in long term storage of memory
Memories transferred from hippocampus
to neocortex during sleep
Deep sleep, slow wave and REM sleep
describe the role of the amygdala in memory
Attaches emotional significance to memories
Strong emotions are difficult to forget
Interaction between hippocampus, neocortex and amygdala determine stability of a memory
Forms new memories related to fear
Fearful memories formed after only a few repetitions
Relevant to PTSD
Describe how sleep is important for learning and memory
However, there are still some open questions regarding the underlying neural mechanisms of sleep:
How NREM and REM sleep influence learning and memory?
Is learning acquired before sleep enhanced or stabilized after sleep, or does sleep protect what was learned from being “overwritten” by learning something new?
is the facilitation of learning learning-specific or learning-independent?
In this study the trained participants in a visual learning task
Then they had a 90 minute nap in Magnetic resonance spectroscopy machine which picks up neurotransmitters.
They measured GABA and glutamate in visual areas while they slept, also had EEG
The were woken up and tested on task again
Findings
1- In NREM sleep there is a release of glutamate, which was called an excitatory shift
2- In REM sleep there was a release of GABA which. Was called and inhibitory shift
3- Individuals with more NREM and excitatory shift, did better, the bigger the shift the bigger the improvement
4- Participants that had more REM sleep had an inhibitory shift which seemed to be less associated to getting better on the task
Second part of study
Same participants learning a different task that interfered with the original task and tested them in the original task
Findings
The participants that did better were the ones that had some NREM but also the inhibitory REM
Interpretation
During NREM the excitatory shift, or increase in glutamate enhances learning through brain plasticity , the brain forms new connections
The inhibitory shift (release of GABA) during REM stabilises the newly formed connections
describe findings around napping
Napping can be helpful for improving memory
Dreaming about a task can boost memory for that task
Some considerations:
Limit napping to short bursts
Target to natural dips in alertness
Long naps may interfere with a normal night’s sleep
Two groups of participants completed online virtual maze goal reaching destination
After completing half were allowed to nap, those who napped were quicker.
In the students that napped they recorded brain activity and asked if they had dreamt.
Those who dreamed or had EEG evidence of dreaming were the quickest.
You can’t control dreams but you can nap.
Good times for napping is after lunch, some Universities are introducing napping pods in exam times.
describe the effect of too much sleep
Sleep quality also important for memory formation
Hypersomnia typically linked with poor sleep quality
Nurses’s Health study:
Compared to those who slept 7-8 hours:
Worse memory performance in those sleeping
<5 hours or >9 hours
Undersleepers and oversleepers were mentally
two years older
describe research findings of poor sleep quality in the elderly
Poor sleep quality linked to memory loss and brain deterioration in the elderly
Compared to 20 year olds, 70 year olds demonstrate
55% decrease in memory
75% reduction in quality of deep sleep
Deterioration of frontal lobe linked with impaired slow wave activity
Memories retained in hippocampus and do not reach neocortex
Describe some negative influences on memory
CORTISOL
High levels disrupt the transfer of information between hippocampus and neocortex
ADENOSINE
Build up of adenosine has been identified as a link between sleep deprivation and poor memory
Caffeine is an adenosine receptor antagonist
SLEEP INTERRUPTION
Makes new memory formation difficult
SLEEPING PILLS
Inhibit the consolidation of memory
describe how sleep can be a revision technique
One of the primary benefits of getting a good regular night’s sleep is that it aids and improves memory and recall.
Recent research suggests that when we sleep new connections are formed between our brain cells.
It appears that sleep actually ‘prioritises memories that we care about’ (something that is particularly handy during revision).
An undeniable part of success in exams is the ability to recall knowledge – something that sleep can clearly help with.
Describe how low levels of sleep can affect the immune system
Teenagers and young adults who don’t get enough sleep are more likely to fall ill
Trend for ill health after a few nights of reduced sleep
Headaches, sniffles, colds all signs of not getting enough sleep
Sleep removes toxins from the body that have built up over the day
Give advantages of sexual reproduction
Sexual reproduction mixes genes whereas asexual reproduction relies on mutation alone.
Within a species, advantageous traits can quickly be bred in (as disadvantageous ones can be bred out). Therefore more chance for adaptation.
Give advantages of asexual reproduction
All of the parent’s genes are passed on to the next generation (i.e. offspring are clones of parent).
In a stable population and environment, advantageous as all they need do is survive to reproductive maturity rather than having to compete for a mate.
Define sexual dimorphism
Most obvious sexual dimorphism is the larger body size of males in many vertebrate species.
Difference in male and female gametes (sperm vs ova) – profound effect on vertebrate sexual behaviour.
Describe the influence of sexual dimorphism on sexual behaviour
MALES:
Produce sufficient sperm to inseminate millions of females
Less selective – rarely dangerous
FEMALES:
Nuture their ‘egg investments’ by choosing mate
Need healthy male
Define and explain parental investment theory
Purports that “the relative investment in offspring by males and females is a key variable in sexual selection”.
In most species (but not seahorses!):
females invest more in offspring and are the choosier sex
males invest less and compete more over reproductively available females
In humans:
Female minimal investment = pregnancy and lactation
Male minimal investment = fertilization (but greater care = greater chance of survival of progeny i.e. true reproductive success)
Define and explain animal mating systems and strategies
Strategies related to differences in investment in offspring.
PROMISCUITY: animals mate with more than one partner and do not establish long-term relationships.
POLYGAMY: ‘many spouses’.
Common feature of animal kingdom is adopting male/female promiscuity as a reproductive strategy.
Male to Male competition for dominance
The strongest male ensures:
In communal groups (herds) almost exclusive access to females (maximise opportunity to pass on genes).
In seasonal bonding species, the territory needed to attract females.
Benefits to female:
Ensures any offspring will be the ‘fittest’ (dominant) i.e. male offspring will be able to pass on her genes).
Ensures access to resources (i.e. food) meaning offspring most likely to survive to reproduce and pass on her genes.
Define and explain monogamy
Monogamy:
One male and one female forming a breeding pair.
Appears to be the norm across all civilisations.
Promiscuity (especially in women) frowned upon.
Human infants are frail and need prolonged care.
Not always permanent.
Give examples of facial cues to attractiveness and their anthropological origins
Symmetry
people prefer symmetrical faces – indicative of good genes and health
skin pigmentation
preference for varying skin pigmentation – indicates health, diet, ability of body to transport oxygen
facial sexual dimorphism
implies levels of hormones flowing (indicates good genes and fertility)
Explain research findings on detecting sexual orientation from facial images
Gay men and lesbians marginally more accurate than heterosexuals (Brambilla et al 2013)
Artificial intelligence using ‘deep neural networks’ that learn to recognise patterns in multi-layered data
Extracted data on facial features from 35,000+ facial images
Fixed features (e.g. nose shape)
Transient features (e.g. grooming style)
Gay men and women tended to have gender-atypical facial morphology, expression and grooming style
AI able to correctly distinguish between gay and heterosexual men (81% of cases) and women (71% of cases)
Describe research findings for a social explanation of homosexuality
Bell, Weinberg and Hammersmith 1981
Large scale study of several hundred male and female homosexuals.
No evidence that homosexuals had been raised by domineering mothers or submissive fathers.
Best predictor of adult homosexuality was a self-report of homosexual feelings.
Conclusion: Data did not support social explanation for homosexuality, but were consistent with biology offering at least a partial explanation.
Describe research findings for a biological explanation of homosexuality
Levels of sex hormones in adulthood
Meyer-Bahlburg, 1984
Levels of sex steroids in male homosexuals are similar to those of heterosexuals.
Variations in sex hormones cannot explain male homosexuality.
BUT
30% of female homosexuals have elevated levels of testosterone.
Whether differences are related to biological cause or differences in lifestyles increasing release of testosterone is not known.
Prenatal androgenisation
Congenital adrenal hyperplasia (CAH)
Adrenal glands secrete excessive amounts of androgens.
Boys born with CAH develop normally, females show masculinisation of genitals.
Money, Schwartz and Lewis (1984)
30 women with CAH asked to describe sexual orientation
48% = bisexual or homosexual.
Conclusion: Exposure of a female foetus to excessive androgens does influence sexual orientation.
Fraternal birth order effect
Probability of male homosexuality increases as a function of number of older brothers (Alexander et al., 2011).
Maternal immune hypothesis
some mothers may become progressively more immune to masculinising hormones in male foetuses? Immune system might deactivate masculinising hormones in younger sons.
Interference with prenatal androgenisation
Maternal stress
Suppressed androgen production in male foetuses.
Less likely to display male sexual behaviour.
More likely to display female sexual behaviour.
Play behaviour also resembles that of females.
Reduces size of sexually dimorphic nucleus (SDN).
In one study (LeVay, 1991) INAH was larger in heterosexual men than homosexuals (not consistently replicated).
Heredity
Identical twins have identical genes whereas fraternal twins average 50% identity.
Bailey & Pillard (1991) Male twins
52% of identical twins – both twins were homosexual.
22% of fraternal twins – both twins were homosexual.
Bailey (1993) Female twins
48% of identical twins – both twins were homosexual.
16% of fraternal twins – both twins were homosexual
Define sexual desire in humans
Defined as:
“A biological process involving steroid hormones acting in the brain of two sexually distinct organisms leveraging on sexual reward”
Relies on steroid hormones, neurotransmitters, vasoactive agents and other molecules acting through specific receptors, at both the brain and peripheral level
It is a complex process, involving both cognitive and peripheral physiological mechanisms, leading to sexual arousal
Sexual arousal = the cerebral activation occurring in both male and female, aiming to prepare genital organs for copulation
Describe the phases of sexual desire
COGNITIVE PHASE
Sexual stimuli (real interaction or pornographic images etc) – activate cognitive state, appraised and categorized as sexual, neural activity increases in specific cortical areas (slightly different between the sexes).
PHYSIOLOGICAL PHASE
Changes in cardiovascular and respiratory functions until the genital response (penile blood flow, erection, swelling, female genital lubrication, cervix and uterus elevate to expand vagina).
Driven by hormones which are affected by
Environmental factors (light and dark), cultural (beliefs about sexual behaviour), psychological (attitudes and cognitions) and relational factors (connection with partner).
Describe the role of testosterone in males
In animals, positive correlations found between testosterone levels and sperm motility, and negative correlations with fat measurements and ejaculation latency time, revealing the hormone’s impact on reproductive traits.
In humans, also affects sexual desire and cognitive phase of arousal.
Visual sexual stimuli are involved in:
Sexual
Emotional
Motivational
arousals which modulate the activity of specific brain regions
Describe the role of testosterone in pre-menstrual females
Relationship with sexual arousal is less clear.
Probably because of complexity of endocrine systems in females, and importance of psychological factors in female sexual desire (emotional attachment, pair bonding).
Anticipation of sexual activity can increase testosterone in females.
BUT hormonal contraceptives can reduce serum testosterone without impairments in sexual interest.
HOWEVER lower testosterone found in breast-feeding mothers complaining of low sexual desire.
May be androgen sensitivity, not level, that is important?
describe the changes that occur with female menopause
Ceasing of menstruation and fertility in females, usually occurs around 45-55y.
Complex body transition and psychological change.
Bodily changes include:
Weight, shape, skin, hair, physical symptoms (e.g. bloating, flushes), sexual function
Describe the endocrinology of menopause

describe the effects of lower testosterone on sexual behaviour
What is known is largely based on symptoms of women who are androgen-deficient because of other reasons – e.g. they have lost their ovaries due to surgery, chemotherapy, or radiation therapy.
Typically, the symptoms of androgen insufficiency include reductions in the following: sexual motivation, sexual fantasies, sexual enjoyment, sexual arousal, vaginal lubrication, vasocongestion, pubic hair, bone mass, muscle mass, and quality of life.
describe changes in sexual behaviour after menopause
76% of middle aged women reported that sex was moderately or extremely important to them
Sexual activity and function decline with age
Significant decline (74% - 56%, p< 0.001) in sexual activity reported between early postmenopausal women and late postmenopausal women
Sexual dysfunction also increased from 42% to 88%
Hormonal, physiological and social changes
define gender dysphoria in childhood
A marked incongruence between one’s experienced/expressed gender and assigned gender, of at least 6 months duration, as manifested by at least 6* of the following (one of which must be criterion A1):
A strong desire to be of the other gender or an insistence that he or she is the other gender (or some alternative gender different from one’s assigned gender)
In boys, a strong preference for cross-dressing or simulating female attire; in girls, a strong preference for wearing only typical masculine clothing and a strong resistance to the wearing of typical feminine clothing
A strong preference for cross-gender roles in make-believe or fantasy play
A strong preference for the toys, games, or activities typical of the other gender
define gender dysphoria in adolescents and adults
Criterion A. A marked incongruence between one’s experienced/expressed gender and assigned gender, of at least 6 months’ duration, as manifested by at least two of the following:
A strong desire to be rid of one’s primary and/or secondary sex characteristics because of a marked incongruence with one’s experienced/expressed gender (or in young adolescents, a desire to prevent the development of the anticipated secondary sex characteristics).
A strong desire for the primary and/or secondary sex characteristics of the other gender.
A strong desire to be of the other gender (or some alternative gender different from one’s assigned gender).
A marked incongruence between one’s experienced/expressed gender and primary and/or secondary sex characteristics (or in young adolescents, the anticipated secondary sex characteristics).
A strong desire to be treated as the other gender (or some alternative gender different from one’s assigned gender).
A strong conviction that one has the typical feelings and reactions of the other gender (or some alternative gender different from one’s assigned gender).
Criterion B. The condition is associated with clinically significant distress or impairment in social, occupational, or other important areas of functioning
describe the aetiology of gender dysphoria
No robust scientific accounts of aetiology
Many theories:
Psychological/developmental – social learning
Trauma-genic/attachment
Neuroanatomical
Sociocultural
Most likely multifactorial with different combinations of causative factors for different children
describe the treatment pathways for gender dysphoria
Psychosocial
Watchful waiting/containment (particularly for under 12s)
Family & individual therapy/support
Parents/teenagers group
Family days
Network meetings/consultation
Referral to adult services
Medical
Hormone blocker treatment
From early puberty (on strict criteria)
Cross sex hormone treatment (testosterone/oestrogen)
From around age 16 only if at least 12 months on blocker and continued therapeutic engagement
No surgery (only in adult services)
describe social relationships and emotional responses with GD
Longstanding feelings of difference/not fitting in
Isolation from/exclusion by peers
Trans* identity as a potential solution – global peer group – story of identity shifts from failure/unhappy misfit to victim of oppressive social structures – opportunities for action
Parents can often be sceptical about GD – particularly expressing that pubertal onset GD has been “downloaded wholesale from the internet”
Impaired Theory of Mind/awareness or concern re societal expectations/norms – enable gender variant expression
Social isolation and reality testing – naivety
Different way of expressing emotion – often describe very clear gender dysphoria but the emotional component doesn’t “ring true”
Describe the relationship between autistic spectrum and gender dysphoria
Both historically pathologised
Now there is an increasing emphasis on difference rather than disorder
Diversity of gender identities – politicised challenge to the gender binary; celebration of the exploration of multiple genders; “unhooking gender from anatomy”
Neurodiversity in autism – differences in styles of brain functioning rather than normal/abnormal binary; politicised challenge to deficit-laden stories of autistic identities – “Aspies”, Nerd culture
Define
- homeostasis,
- metabolism,
- hunger,
- satiation,
- satiety,
- peripheral appetite control
- central appetite control
Homeostasis – The ability to maintain a relatively stable internal state.
Metabolism – The process by which your body converts what you eat and drink into energy
Hunger - The drive to consume, elicits a behavioural response (eating) to a biological need.
Satiation - Processes during a meal that generate negative feedback leading to its termination (within-meal inhibition).
Satiety - The end state of satisfaction. The further suppression of the drive to consume and post-meal intake (between-meal inhibition).
Peripheral appetite control – Includes motor functions of the stomach (e.g. rate of emptying) and release of peptides and hormones from the gut and fat tissue.
Central appetite control – Brain and central nervous system.
describe homeostasis and energy balance
Negative feedback systems:
Feedback from changes in one direction elicit compensatory changes in the opposite direction.
Act to maintain homeostasis – a stable environment.
Energy balance (EB):
Energy intake (EI) minus energy expenditure (EE).
In an ideal homeostatic energy system an organisms energy intake should equal energy expenditure.
Describe the homeostatic control of energy
A biological need to maintain the body’s energy stores.
Depletion of energy stores → drive to eat.
Repletion of energy stores → negative feedback signals to terminate eating.
Co-ordinated by the hypothalamus.
Define asymmetry of homeostatic control
Defends well against energy deficit. However, defence against energy excess is weaker.
→ More sensitive to under-eating than over-eating.
→ We can gain weight more than easily than losing weight.
“Eat more” command is dominant over the “Stop eating” command.
describe the mechanism of starting a meal

Describe the mechanism of ending a meal

Describe the role of CCK and GLP-1
Duodenal Brake
CCK’s response to fat in the duodenum.
Decreases rate of gastric emptying
Satiation and early satiety
Further down the small intestine…
Ileal Brake
GLP-1 responds to fat.
Post-meal satiation and reduced hunger at the next meal
Describe the mechanism of CCK and glp-1
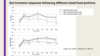
Describe the control and actions of leptin
Produced by adipose tissue (the body’s fat stores) when ‘full’.
Reduces food intake.
Long term (“tonic”) signal.
Genetically obese mice (ob/ob) cannot produce leptin because they are born without required gene code.
Give evidence for weaker regulatory control in people with obesity
Weaker gastric distention (Geliebter, 1988).
Blunted satiety hormone response to eating (PYY, GLP-1) (Lean & Malkova, 2016).
Rare cases of human obesity where leptin cannot be produced due to gene defect.
However, most people with obesity people do not possess a leptin deficiency. In fact, they produce excess leptin
→ leptin insensitivity or leptin resistance?
Describe how the CNS controls appetite
CNS regions receive signals from the body (e.g. gut, liver).
Receptors within the CNS also detect circulating levels of nutrients.
Substances, such as glucose, can cross the blood-brain barrier.
Specific neuronal populations recognise and integrate energy-relevant signals and act in a network to integrate multiple signals and determine energy intake and expenditure.
Describe which and how CNS structures are involved in appetite regulation – lower
Vagal Nerve
Afferent fibres from gastrointestinal tract and liver up to brain stem
Brain stem (Hind Brain)
Relays afferent vagal signals associated with eating to the hypothalamus. Key sites are:
Nucleus Tractus Solitarius - NTS.
Area Postrema - AP (adjacent to NTS).
Describe how CNS structures are involved in higher appetite regulation
Hypothalamus
Key hypothalamic sites:
Arcuate Nucleus (ARC)
Ventro-Medial Hypothalamus (VMH).
Lateral Hypothalamus (LH).
Paraventricular Nucleus (PVN).
Describe how CNS structures are involved in appetite regulation – neuronal populations
The ARC contains functionally discrete populations of neurones:
Orexigenic (stimulate food intake): Anorexigenic (inhibit food intake):
Neuropeptide Y (NPY) Pro-opiomelanocortin (POMC)
Agouti-related peptide (AGRP) Cocaine and amphetamine-regulated transcript (CART)
The ARC has extensive reciprocal connections with other hypothalamic regions including the PVN, VMH, and LH.
These regions receive afferent information via the NTS/AP.
Describe how the CNS is involved with the mechanism of satiety
5-HT (Serotonin):
A key CNS satiety signal in the short-term (“episodic”) regulation of food intake.
5-HT drugs are successfully used as appetite suppressants to treat obesity.
The 5-HT drug Lorcaserin hit the headlines last year, hailed as a “magic bullet”.
Describe the mechanisms of reward-motivated eating
Eating for pleasure or to feel better
Cues associated with the intake of tasty foods (e.g. the sight and smell of food) acquire strong motivational properties and become highly wanted.
Describe the anhedonia theory
Wise, 1982
Dopamine mediates pleasure, based on observation of rat behaviour:
Disruption of brain dopamine systems lead to failure to eat or drink.
Dopamine receptor antagonists reduce working for food.
Argued that apparent loss of motivation to eat is due to loss of reward – or hedonic consequences – that are normally mediated by dopamine.
Explain why the anhedonia theory is wrong
Dopamine blockade prevents animals from attending to food, and working to obtain it – but this reflects motor incapacity not motivational deficit.
Stimulating dopamine activity can increase responding for food – but doesn’t increase how much is eaten!
Critical experiments show that dopamine is not required for the experience of pleasure from eating.
Describe Berridge’s theory of food reward
Food reward contains distinguishable psychological components that are controlled by separate neurobiological systems.
Key distinction is between processes associated with affective vs. motivational consequences of consuming food.
→ Core processes of Liking and Wanting.
Liking represents the pleasure or affective aspect of food. Liking may activate, but does not require, wanting
Wanting is the motivational component – also known as “incentive salience”. Wanting without liking adds the compulsive element to eating.
Describe the role of dopamine in liking
Chemical lesions of brain dopamine systems using 6-hydroxydopamine (6-OHDA)
Aphagia (rejection of food)
Adipsia (absence of thirst)
but NORMAL taste reactivity
Hedonic evaluation of food (“liking”) is therefore independent of dopamine.
Describe the link between dopamine and incentive salience
Dopamine does play a role in:
Recognizing motivationally important stimuli.
Energizing of goal-directed behaviour.
Learning of associations between psychological state/experience, environmental stimuli and behaviour.
Effort
Dopamine thus serves alerting and activating functions related to wanting.
Describe what mediates liking
Natural opioid (opiate-like) chemicals occur in the brain.
Morphine increases food intake.
Opioid antagonist drugs reduce food intake.
Naloxone reduced hedonic preference for sweet, high-fat foods in humans (Drewnowski et al. 1992, Physiology & Behavior, 51, 371-9).
Evidence for a specific role for opioids in liking (but not wanting).
Define cue reactivity
Learned associations between food cues (e.g. the sight and smell of food) and the rewarding consequences of eating.
These cues elicit conditioned responses such as:
Increased desire and craving for food.
Attentional bias.
Physiological changes (e.g. increased salivation).
Food-seeking behaviours.
Define and explain craving
Food craving - an intense desire which is directed towards a particular food, drink or taste (Hill, 2007, Proceedings of the Nutrition Society, 66, 277-285).
Explain what is happening in the brain when we crave chocolate
Chocolate cravers vs non-cravers
Sight and flavour of chocolate, plus their combination
fMRI
Greater activation in medial OFC and ventral striatum in cravers
Describe the link between obesity and cue regulation
Exposure to sight and smell of pizza increased desire to eat and salivary response in participants with obesity relative to participants who were healthy weight (Ferriday & Brunstrom, 2011).
→ increased motivation to consume food.
People with obesity showed a greater attentional bias to food images, but only when they were satiated (Castellanos et al., 2009).
Give neural evidence for differences in cue reactivity by weight status
Rothemund et al. (2007), NeuroImage, 37, 410-421.
fMRI study assessed responses to pictures of high-calorie foods, low-calorie foods, eating-related utensils and neutral images, following abstinence from eating for at least 1.5 h.
Women with obesity (BMI > 30) showed greater activation to high-calorie foods vs. neutral images in the caudate/putamen (reward/motivation), anterior insula (taste, interception, emotion), hippocampus (memory) and parietal cortex (spatial attention).
This was in relation to a control group of women who were lean (BMI 19–24)
Describe cognitive control of appetite
Without higher level control/executive control, we would be slaves to our reward system.
But we do not always respond to the presence of food cues by initiating eating. Some individuals are very successful at controlling their food intake.
An appetitive response to a tasty food may be inhibited if the individual has a long term goal for health (for empirical support see Yokum & Stice, 2013).
Goals, values and expectations.
Inhibitory control.
Memories.
Involvement of ventromedial-prefrontal cortex (vmPFC) and a network that includes dorsolateral prefrontal cortex (dlPFC).
Obesity is characterized by lower gray matter volume in brain areas important for executive control (García-García et al., 2018) https://www.nature.com/articles/s41366-018-0164-4
Describe cognitive control increases during satiation
Thomas et al (2015):
16 healthy participants were scanned on 2 separate test days, before and after eating a meal to satiation or after not eating for 4 h.
Satiation reduced activity in reward-related brain regions.
Satiation increased activity in the dorsolateral prefrontal cortex (dlPFC),
→ “top down” cognitive influence on satiation.
Describe the link between memory and eating
Case of RH
R.H. had bilateral damage to the medial temporal lobes which resulted in severe amnesia.
He was able to eat multiple meals:
Ate three meals in a short space of time. Rejected a fourth meal because his “stomach as a little tight”.
→ R.H was unable to remember his recent eating and continued to eat as a result.
A large number of studies with neurologically intact participants indicate that memories about recent eating episodes are an important determinant of food intake (Higgs, 2005, Physiology & Behavior, 85, 67-72).
Describe practical applications of gastric distension
Intra-gastric balloon – silicone balloon placed in stomach and filled with a sterile saline solution. Balloon partly fills the stomach → Fullness.
Balloon is left in place for up to six months.
Balloon helps to control appetite and reduce food intake. Leads to weight loss when combined with appropriate diet and behavioural modifications.
Gastric discomfort, nausea, and vomiting are common short-term side-effects. Longer-term side-effects include pain and/or heaviness in the tummy or back, gastro-oesophageal reflux and indigestion.
describe and define sensory-specific satiety
the decline in the pleasantness of a food as it is eaten relative to an uneaten food.
the dessert effect
An adaptive mechanism.
Makes it easy for us to over-eat when there is a lot of variety.
Define addiction
The official diagnostic labels are currently:
‘(substance) use disorder’ (e.g. ‘alcohol use disorder’) (DSM V)
‘harmful use’ and ‘dependence syndrome’ (ICD-10)
Define A/T/SUDS
Often described as a chronically relapsing disorder characterized by
Compulsion to seek and take substance
Loss of control limiting intake
Emergence of a negative emotion state when access to substance is prevented (e.g. withdrawal)
Give some of the DSM-5 criteria for SUD/AUD
A problematic pattern of alcohol use leading to clinically significant impairment or distress, as manifested by at least two of the following, occurring within a 12-month period:
- Alcohol is often taken in larger amounts or over a longer period than was intended
- There is a persistent desire or unsuccessful efforts to cut down or control alcohol use
- A great deal of time is spent in activities necessary to obtain alcohol, use alcohol, or recover from its effects
- Craving, or a strong desire or urge to use alcohol
- Recurrent alcohol use resulting in a failure to fulfil major role obligations at work, school, or home
- Continued alcohol use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of alcohol
- Important social, occupational, or recreational activities are given up or reduced because of alcohol use
- Recurrent alcohol use in situations in which it is physically hazardous
- Alcohol use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by alcohol
- Tolerance, as defined by either or both of the following: (a) A need for markedly increased amounts of alcohol to achieve intoxication or desired effect; (b) A markedly diminished effect with continued use of the same amount of alcohol
- Withdrawal, as manifested by either of the following: (a) The characteristic withdrawal syndrome for alcohol; (b) Alcohol (or a closely related substance, such as a benzodiazepine) is taken to relieve or avoid withdrawal symptoms
Describe how compulsion is characterised in alcohol use disorder
Characterises alcohol use disorder as follows:
A problematic pattern of alcohol use leading to clinically significant impairment or distress, as manifested by at least two of the following, occurring within a 12-month period:
- Alcohol is often taken in larger amounts or over a longer period than was intended
- There is a persistent desire or unsuccessful efforts to cut down or control alcohol use
- A great deal of time is spent in activities necessary to obtain alcohol, use alcohol, or recover from its effects
- Craving, or a strong desire or urge to use alcohol
- Recurrent alcohol use resulting in a failure to fulfil major role obligations at work, school, or home
- Continued alcohol use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of alcohol
- Important social, occupational, or recreational activities are given up or reduced because of alcohol use
- Recurrent alcohol use in situations in which it is physically hazardous
- Alcohol use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by alcohol
- Tolerance, as defined by either or both of the following: (a) A need for markedly increased amounts of alcohol to achieve intoxication or desired effect; (b) A markedly diminished effect with continued use of the same amount of alcohol
- Withdrawal, as manifested by either of the following: (a) The characteristic withdrawal syndrome for alcohol; (b) Alcohol (or a closely related substance, such as a benzodiazepine) is taken to relieve or avoid withdrawal symptoms
Describe how loss of control is characterised in alcohol use disorder
A problematic pattern of alcohol use leading to clinically significant impairment or distress, as manifested by at least two of the following, occurring within a 12-month period:
- Alcohol is often taken in larger amounts or over a longer period than was intended
- There is a persistent desire or unsuccessful efforts to cut down or control alcohol use
- A great deal of time is spent in activities necessary to obtain alcohol, use alcohol, or recover from its effects
- Craving, or a strong desire or urge to use alcohol
- Recurrent alcohol use resulting in a failure to fulfil major role obligations at work, school, or home
- Continued alcohol use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of alcohol
- Important social, occupational, or recreational activities are given up or reduced because of alcohol use
- Recurrent alcohol use in situations in which it is physically hazardous
- Alcohol use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by alcohol
- Tolerance, as defined by either or both of the following: (a) A need for markedly increased amounts of alcohol to achieve intoxication or desired effect; (b) A markedly diminished effect with continued use of the same amount of alcohol
- Withdrawal, as manifested by either of the following: (a) The characteristic withdrawal syndrome for alcohol; (b) Alcohol (or a closely related substance, such as a benzodiazepine) is taken to relieve or avoid withdrawal symptoms
Describe how negative emotional state is characterised in alcohol use disorder
A problematic pattern of alcohol use leading to clinically significant impairment or distress, as manifested by at least two of the following, occurring within a 12-month period:
- Alcohol is often taken in larger amounts or over a longer period than was intended
- There is a persistent desire or unsuccessful efforts to cut down or control alcohol use
- A great deal of time is spent in activities necessary to obtain alcohol, use alcohol, or recover from its effects
- Craving, or a strong desire or urge to use alcohol
- Recurrent alcohol use resulting in a failure to fulfil major role obligations at work, school, or home
- Continued alcohol use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of alcohol
- Important social, occupational, or recreational activities are given up or reduced because of alcohol use
- Recurrent alcohol use in situations in which it is physically hazardous
- Alcohol use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by alcohol
- Tolerance, as defined by either or both of the following: (a) A need for markedly increased amounts of alcohol to achieve intoxication or desired effect; (b) A markedly diminished effect with continued use of the same amount of alcohol
- Withdrawal, as manifested by either of the following: (a) The characteristic withdrawal syndrome for alcohol; (b) Alcohol (or a closely related substance, such as a benzodiazepine) is taken to relieve or avoid withdrawal symptoms
Describe how development of an AUD/SUD typically follows a pattern
Experimental drug use – casual drug use – heavy drug use – compulsive drug use (dependence) – AUD/SUD
Describe the prevalence and impact of AUD/SUDs
AUD/SUDs are one of the largest contributors to the global burden of mortality and premature death.
Also a high economic burden
Importantly, they are preventable (i.e. non-communicable disease)
Disability Adjusted Life Years (DALYs): The sum of years of potential life lost due to premature mortality and the years of productive life lost due to disability
ALCOHOL
Approx. 18.4% of the population (39.6% of the drinking population) report heavy drinking (bingeing)
DALYS: 85 m
Cirrhosis, traffic accidents, cancers
ILLICIT SUBSTANCES
Cannabis 3.8%
Amphetamine 0.77%
Opioids 0.37%
Cocaine 0.35%
Injecting drugs 0.25%
DALYS: 27.8 m
Cirrhosis, HIV, liver cancer
Harms and prevalence etc are much more difficult to keep track of when drug use is unsanctioned
TOBACCO
15.2% of the adult population smoke daily (approx. 933.1 million people)
DALYS: 170.9 m
Cancers, chronic respiratory disease, chronic obstructive pulmonary disease
Describe differences in alcohol/substance use between countries
Countries with predominantly Muslim populations: lower rates of alcohol problems, higher rates of tobacco smoking.
Tobacco smoking is declining in Western countries but increasing in developing countries.
Other regional trends, e.g., methamphetamine in some states of the USA
Describe how trends in alcohol/substance use change over time
In the UK:
Rates of smoking are declining (taxation and the smoking ban have helped)
The number of people who drink alcohol has declined, but among drinkers the number of people who drink too much has increased (pricing and availability probably played a role again)
New drugs become fashionable (e.g. mephedrone), others fall out of favour (e.g. ecstasy)
E-cigarettes seemed to come out of nowhere and have divided opinion
Describe addiction as a choice
Historical account: Moral failure, lack of willpower or a weakness of self.
Drug use as a cost-benefit analysis (West, 2006)
Benefits Costs
Pleasurable high Hangover
Increased alertness Illness
Social aspects Death
Describe consequences of a free choice model of addiction
‘Addicts’ are stigmatised (don’t use the term ‘addict’!)
Funding and research is unnecessary - a punitive response to the problem is required
Doesn’t really account for the preference shift in addiction
Describe addiction as a disease and the potential consequences of viewing it this way
Key claims:
All drugs of abuse effect (directly or indirectly) a pathway deep within the brain.
Both acute and prolonged drug use causes pervasive changes in brain structure and function that persist long after the individual stops taking the drug. The ‘addicted’ brain is different than the non addicted brain in terms of structure and function.
‘A metaphorical switch in the brain seems to be thrown as a result of prolonged use’ Leshner (1997)…. That addiction is tied to changes in brain structure and function is what makes it, fundamentally, a disease’
Implications: We shouldn’t marginalize those with an A/SUD, but rather we should be trying to treat them. Similarly, incarcerating individuals won’t work.
Give the key brain regions of addiction
Mesolimbic dopamine system: the ventral tegmental area and areas that project to and from it.
All drugs of abuse stimulate dopamine release in the mesolimbic system (directly or indirectly) (Nestler, et al 2005).
Also stimulated by food, sex, warmth, and other “natural” rewards.
Describe key steps in synaptic transmission
The key steps in fast synaptic transmission.
An action potential, initiated at the axon hillock of the presynaptic cell, propagates to, and depolarizes the presynaptic terminal.
Voltage-gated calcium channels in the presynaptic terminal are activated by this depolarizing wave, allowing a rapid and localized increase in calcium at the active zone.
This increase in calcium results in the rapid fusion of neurotransmitter-filled vesicles to the presynaptic membrane which then release their contents via exocytosis.
The neurotransmitter molecules diffuse across the synaptic cleft where they bind to ligand-gated ion channels which gate the influx of ions into the postsynaptic dendritic bouton.
This influx of ions generates an excitatory or inhibitory postsynaptic potential depending on whether the channels are excitatory (glutamatergic) or inhibitory (GABAergic).
The neurotransmitter molecules are then taken back up into the presynaptic terminal by active mechanisms.
This entire process, from the initiation of the action potential in the presynaptic terminal to the generation of a postsynaptic potential, takes only a couple of milliseconds.
describe animal models of addiction
Rats will self-administer most drugs directly into Nucleus accumbens (NAc)
Rat self-administration model is a valuable tool for assessing abuse potential/liability (O’Connor 2011)
If the Nac is destroyed, rats will reduce self-administration (respond less)
Conditioned place preference
A rat experiences a drug in environment A and nothing in environment B. In a drug-free state the rat will choose to spend time in environment A.
describe dopamine as a reward
Over-simplistic view.
Natural rewards (food, sex, water) also stimulate the mesolimbic pathway. So why are we more likely to become addicted to drugs?
Different magnitudes of dopamine release? Not likely.
Both addicted and non-addicted persons may experience pleasurable effects equally.
Similar magnitudes for natural-rewards
describe incentive sensitisation theory
Robinson & Berridge
Repeated drug administration = sensitization
Brain mesolimbic dopamine system becomes ‘hyper-responsive’ to the drug.
Not hyperactive, hyper(RE)active.
Sensitization = drug effects increase over repeated use (opposite of tolerance)
However, not everything is sensitized just:
Psychomotor effects (e.g., blinking, vigour)
Incentive motivational effects (incentive salience)
Robinson & Berridge argue that the most important psychological change is ‘sensitization’ (i.e. hypersensitivity) to the incentive motivational effects of drugs and drug-associated stimuli
describe incentive salience
Robinson and Berridge (1993, 2003)
Repeated drug use leads to a sensitized (increasing) spike in DA activity in the mesolimbic pathway
Importantly, this is not only seen when the drug is ingested but ALSO when they are exposed to drug related cues (Pavlovian conditioning)
Exaggerated dopamine response manifests as incentive salience. Drug cues have strong motivational properties
Exposure to drug-related cues increase ‘wanting’
describe incentive sensitisation theory - the paradox
As incentive sensitization develops, drugs are wanted more but liked less.
Although to begin with most drugs produce positive effects (e.g., euphoria) which can maintain drug use, over time these effects seems to decrease (as addiction develops - tolerance).
The incentive sensitization theory: repeated drug use sensitizes the neural systems that mediate the motivational process of incentive salience (wanting), but NOT the neural systems that mediate the pleasurable effects of drugs (liking).
Therefore, drugs will be wanted more but liked less over time.
Individuals who are dependent on drugs often report they ‘want’ drugs but no longer ‘like’ them.
Think back to the DSM 5 criteria. :Craving, strong urges… despite wanting to cut down, no longer finding the drug appealing.
The incentive salience model therefore has considerable intuitive appeal
describe wanting vs liking in alcohol consumption
Hobbs et al 2005
Experiment 1: Separated individuals into heavy and light drinkers and examined liking ratings of a variety of drinks (alcoholic and non-alcoholic).
No interaction between drinking status and type of drink on liking.
Experiment 2: Manipulated ‘wanting’ by a small priming dose of alcohol.
Again, no changes in liking for the alcoholic drink. But an increase in wanting.
describe incentive sensitisation theory: withdrawal and relapse
The sensitization process lasts a long time (longer than tolerance or physical withdrawal).
Even after the negative effects of withdrawal have diminished, the brain’s neural system underlying ‘wanting’ is sensitized.
This long-term sensitization results in enhanced, long-term risk of relapse.
For example, if the circumstances are right, relapse may be likely even after years of abstinence.
Sensitization is a long-term adaptation. Remember addiction is a ‘chronic relapsing disorder’, IS can help to explain this.
Describe incentive sensitisation theory and learning
We focus on drugs because of an interaction between incentive salience and associative learning mechanisms which usually directs our motivation to appropriate targets (e.g., food, sex).
Although learning processes identify the stimulus of interest, it is sensitization of brain circuits that mediate Classical conditioned incentive motivational processes (i.e., incentive sensitization) that result in pathological drug-related motivation
Associative learning processes are important because they can determine where, when, and how sensitised behaviour is expressed.
This helps explain why pathological drug behaviour can be restricted to certain environments (i.e., those that have been previously associated with drug taking)
So there is contextual control over the expression of sensitization, and this stems from associative learning.
Null research findings may be due to absence of CSs
describe IST and cognitive dysfunction
Cognitive Dysfunction
Drug addicts show significant cognitive impairment; executive function, decision making, inhibitory control etc are all affected (via adaptations to prefrontal cortex).
Incentive Sensitization Theory: impairment of executive function has an important role in addiction, esp. the bad choices about drugs. Combine this with the pathological incentive motivation for drugs (via incentive sensitization) and the result is addictive behaviour.
Chronic drug use is associated with volumetric loss of frontal lobes
describe hedonic homeostatic dysregulation theory
George Koob
Drug addiction: chronically relapsing disorder characterized by
compulsion to seek and take the drug
loss of control in limiting intake
a negative emotional state reflecting a motivational withdrawal syndrome when access to the drug is prevented
Both sensitization and opponent-processes contribute to ‘hedonic homeostatic dysregulation’: dysregulation of brain reward (DA) that gets progressively out of control.
Sensitization occurs in the early stages of addiction and causes increased liking for drugs (results in bingeing). Represents a break from homeostasis.
Counteradaptation (e.g., opponent-processes) occur in the latter stages to produce withdrawal and negative affect.
describe the addiction pathway
3 stages:
binge / intoxication
withdrawal / negative affect
preoccupation /anticipation
The development from recreational to dependent use is due to brain adaptations.
Animal models can be used to represent the withdrawal/negative affect stage of Koob et al’s (2009) addiction cycle.
Conditioned place aversion (animals avoid environments paired with withdrawal)
Increased motivation for self-administration in dependent animals (animals are motivated to take drugs to remove withdrawal state)
Anxiety-like responses (e.g. freezing, burying)
describe the findings of Koob and Volkow 2010
Impulsivity and compulsivity are important
Impulsivity tends to be more important in earlier stages
Both impulsivity and compulsivity are important in later stages
Impulsivity: behavioural disposition for fast, unplanned actions triggered by ext/int stimuli with no regard to potential negative consequences. Impulsivity is a core deficit in SUD.
Measured:
1) choice of small immediate over large delayed reward
2) Inability to inhibit behaviour by changing or stopping a behaviour once initiated (i.e. response inhibition).
Compulsivity: persevere in responding despite adverse consequences, and incorrect responding in choice situations. Persistent reinitiation of habit-like acts. DSM-V: persistent use despite knowledge of negative physical/psychological problems; lots of time spent in activities trying to obtain the substance.
Addiction: a cycle of spiralling dysregulation of brain reward/antireward mechanisms that progressively increases, resulting in the compulsive use of drugs.
describe koob and allostasis
The brain works to maintain homeostasis. Counter adaptation is one mechanism of maintaining homeostatic regulation.
Over prolonged drug use, the brain tries to adapt and counter adaptations / opponent processes alter set-points
Deviation from normal brain-reward threshold regulation is described as an allostatic state.
Allostasis: stability through change.
Allostasis is more complex than homeostasis and it results in changes to reward mechanisms in an attempt to achieve stability.
The brain tries to respond to the continued presence and effects of drugs and so alters set-points (so drugged brain is ‘normal’)
Sensitization and counteradaptation processes cause further attempts to maintain mood at this new set point (allostasis) > but with increasing drug use, it becomes more difficult to maintain this set point…
At some point, allostasis breaks down and the individual cannot maintain a set point > ‘spiralling distress’, or mood disturbance
Hedonic homeostatic dysregulation drives dependent drug use.
Hedonic homeostatic dysregulation is an negative emotional state which is apparent when drug use is prevented (which creates craving etc)
Hedonic homeostatic dysregulation is a result of a combination of decreased reward system function and increased brain stress response system function
Hedonic homeostatic dysregulation lasts a long time (into protracted withdrawal), therefore there is a residual negative state which is an ongoing relapse risk
Describe Koob’s research on brain adaptations
Koob identifies 5 circuits which change as addiction progresses
- Mesolimbic dopamine system (incentive salience and reward)
- Ventral striatum (increase in DA activates the VS)
- Ventral striatum/dorsal striatum/thalamus circuits(activity shifts from ventral to dorsal striatum (fMRI). Corresponds with drug use going from acute/goal-directed to chronic/habitual)
- Prefrontal cortex /hippocampus circuits (impaired executive function, poor decision making, e.g. choose reward now [drug] rather than longer term reward)
- Extended amygdala (stress system activated, leads to a negative states which drives use of natural reinforcers)
describe the brain model of addiction and treatment
Pharmacological strategies that target specific clinical components of addiction are developing. These may target alcohol/substance-induced euphoria (e.g. naltrexone), hedonic dysregulation, cue- or stress-induced craving (e.g. acamprosate??) etc.
For instance, naltrexone may work by reducing opiate and alcohol-induced reward, modafinil may reduce cocaine-induced euphoria (e.g. Anton (2008) Naltrexone for the Management of Alcohol Dependence)
Research suggests vaccines may be possible which blocks the drug entering the brain (e.g. Kosten (2005) Future of anti-addiction vaccines)
Disulfiram disrupts the metabolism of alcohol to induce sickness, so people avoid drinking (serious side effects, including death can occur if a person persists in drinking heavily/regularly on disulfiram)
give consequences of a disease model
It has led to over investment: 41% of addiction funding is for basic neuroscience with a further 17% developing ‘biological cures’.
But are we any closer to really understanding and treating addiction?
A good theory of alcohol/substance use should be able to inform development of interventions/treatment.
The disease model has supported development of new pharmacotherapies BUT few new drugs have been developed based on neurobiology.
The most widely used drugs in addiction?
Methadone Replacement Therapy
Nicotine Replacement Therapy
What about spontaneous remission / unassisted recovery?
Recovery is a social process – we change our identity, we become empowered.
It’s argued to have helped reduce stigmatization of ‘addicts’(but see Buchman et al (2010
Give a brief overview of treating SUDs
Alcohol use disorders
Treatments like naltrexone block opioid receptors, reducing the release of dopamine, and making alcohol consumption less pleasurable
Opioid use disorders
As with alcohol, treatments focus on blocking opioid receptors, by prescribing a less addictive opioid, such as methadone or naltrexone
Smoking cessation
Treatment focuses on replacing the nicotine smokers receive from smoking with nicotine delivered in a different form (e.g., nicotine patches or gum, e-cigarettes)
Describe the biopsychosocial model of drinking alcohol
Cox and Klinger (1988) argue that people drink alcohol for various reasons:
biological (drinking is rewarding),
psychological (drinking is enjoyable)
social/environmental (peer drinking)
describe the biological basis of treatments for AUDs
Because alcohol affects multiple aspects of brain activity, treatments have been developed that work in different ways:
Blocking the opioid receptor system (Naltrexone)
Pairing drinking with negative biological effects (Disulfiram)
evaluate the effectiveness of naltrexone
Rosner et al. (2010) reviewed 50 RCTs with 7793 patients. Naltrexone reduced the risk of heavy drinking to 83% of the risk in placebo (Risk Ratio = 0.83; CI[0.76;0.90) - Gives likelihood of something happening between groups
The authors conclude that although small treatment effects these should be valued against the relapsing nature of alcoholism
Describe the use of disulfiram and evaluate its effectivness
Disulfiram blocks the enzyme aldehyde dehydrogenase (ALDH)
When a patient who has taken Disulfiram has an alcoholic drink there is a build up of acetaldehyde which leads to a Disulfiram ethanol reaction (DER)…
Nausea
Vomiting
Tachycardia
Dizziness
Knowing that drinking leads to unpleasant effects quickly—because Disulfiram blocks the liver’s ability to break down the ALDH into acetaldehyde—changes patients’ beliefs about the effects of alcohol…
Disulfiram combines a biological mechanism of action with a psychological mechanism of action
EFFECTIVENESS OF DISULFRAM
Skinner et al. (2014)’s systematic review compared the efficacy of Disulfiram to various control groups.
They included 22 trials (N = 2414) patients
Patients given disulfiram did better than control groups on a range of outcomes
Skinner et al. also tested the effect of knowing you are receiving disulfiram (open label) compared to being blind to condition on treatment effectiveness
BLIND/OPEN LABEL DESIGNS
Blind design (K = 7) = patients don’t know they are on Disulfiram
Open label design (K = 15) = patients know they are on Disulfiram
For blind designs, there was no difference in outcomes between the Disulfiram groups and control groups
For open label designs, there was a difference between the Disulfiram groups and control groups
describe research findings for why people smoke and why it is hard to quit
Shahab & West (2010) argue that people smoke for various reasons:
biological (nicotine is rewarding),
psychological (smoking is enjoyable)
social/environmental (peer smoking)
The main biological reason for smoking is that inhaling nicotine alters the balance of dopamine (neurotransmitter) and noradrenaline (hormone)
These changes can be perceived as pleasurable and this is a key explanation as to why people smoke
WHY IS IT HARD TO QUIT SMOKING?
Inhaling nicotine is associated with dopamine release, which is reinforcing
Over time nicotine receptors attach themselves to neurons in the brain, leading smokers to crave nicotine to promote dopamine release
Quitting smoking is hard because smoking stimulates dopamine release, which is rewarding
Can lead to heart disease, common obstructive pulmonary disorder, cancer (espec. Lung/cervical)
Evaluate the effectiveness of smoking cessation methods
NHS STOP SMOKING SERVICES
NHS Stop Smoking Services comprises several elements designed to support smokers to quit:
Smoking cessation medications: Nicotine replacement therapy, bupropion, varenicline
Group or one-to-one meetings with a stop smoking advisor
EFFECTIVENESS
Bauld et al. (2009) reviewed 20 studies that tested the effectiveness of NHS stop smoking services
They found a quit rate of 53% at four weeks…
…which dropped to 15% at 1 year
While this is a dramatic fall over time, it is estimated that quitting without support only leads to 5% success!
NICOTINE REPLACEMENT THERAPY
Nicotine Replacement Therapy (NRT) is used to help smoking cessation – replaces the nicotine inhaled from cigarettes
NRT products were first licensed in the USA in 1984
EFFECTIVENESS
Hartmann-Boyce et al.’s (2018) Cochrane review of RCTs analysed 133 studies (N = 64,640) to compare quitting among groups receiving any form of NRT (gum, patches etc.) with non-NRT control group.
They estimated that the Risk Ratio (RR) of quitting for any form of NRT, relative to control, was 1.55 [1.49;1.61]
This means that smokers using NRT have a 55% higher chance of quitting relative to smokers not given NRT
Describe barriers to nicotine replacement therapy
WHY IS NRT UNPOPULAR?
Side Effects of gum
Nausea
Hiccups
Irritation of the mouth
Side effects of the patch
Skin irritation
Dry mouth
‘Weird’ dreams
PATIENT BELIEFS ABOUT ACCESS TO NRT
Vogt et al. (2008) Study 1 found that patients believed there were several barriers to accessing NRT
NRT perceived to be expensive (not all patients were aware that NRT is available on prescription)
Patients were concerned about how long it would take to make a GP appointment to get a prescription
Others believed they would be wasting time waiting around for GP appointments
PATIENT BELIEFS ABOUT THE DESIRABILITY OF NRT
Vogt et al. (2008) Study 1 found that patients associated taking NRT with the following side effects:
Skin reactions
Feeling unwell
Mouth pain
Bad taste
Bad dreams
Some patients believed taking NRT would be like swapping addiction to cigarettes smoking to addiction to NRT
Some patients viewed quitting using NRT as admitting to being ‘weak-willed’, and quitting in this way would diminish the achievement
PATIENT BELIEFS ABOUT THE EFFECTIVENESS OF NRT
Vogt et al. (2008) Study 1 reported that patients were unsure NRT would stop them craving cigarettes
“I am slightly unsure [NRT] would actually work…because I know people who had nicotine patches but then have gone back to smoking because…it has not stopped the cravings”
They also found that patients were certain NRT would not address psychological reasons for smoking cigarettes
“It [NRT] would cut down the craving…but other times out of boredom or stress…when you want to do something with your hands…I can’t see it helping”
evaluate research findings on counselling as a treatment for smoking cessation
Bauld et al. (2009) on group vs. 1-to-1 counselling
Included in Bauld et al.’s (2009) where two studies that compared group vs 1-to-1 counselling
Judge et al. (2005) found smokers who received group counselling more likely to quit (OR = 1.38; CI [1.09;1.76])
McEwan et al. (2006) found that 30% of clients receiving group treatment vs. 19% of clients receiving 1-to-1 treatment were abstinent at 4 weeks
Bauld et al. note that group sessions are not attractive for many smokers and may not be feasible to deliver in rural areas.
Stead et al. (2017) review of group vs. self-help
Stead et al.’s (2017) Cochrane review compared group therapy with (1) self-help, (2) brief support from a healthcare professional and (3) individual counselling,
Outcome was abstinence at 6 months
13 trials (N = 4395) compared group programmes to self-help (Risk Ratio = 1.88; CI [1.52;2.33])
Smokers who received group therapy were 88% more likely to be abstinent at 6 months than those who used self-help
Stead et al. (2017) review of group vs. 1-to-1 counselling
14 trials (N = 7286) compared group programmes to brief support from a healthcare provider (Risk Ratio = 1.22; CI [1.03;1.43])
Smokers who received group therapy were 22% more likely to be abstinent than those receiving brief support from HCP
6 trials (N = 980) compared group programmes to intensive individual counselling (Risk Ratio = 0.99; CI [0.76;1.28])
No difference between group and intensive individual counselling
evaluate pharmacological treatments for alcohol use disorders and smoking cessation
PHARMALOGICAL TREATMENTS FOR ALCOHOL USE DISORDERS – BLOCKING THE SUBSTANCE EFFECTS
Pharmacological Treatments for alcohol use disorders block the effects of alcohol on the body: naltrexone blocks alcohol’s effects on the opioid system; disulfiram blocks the enzyme ALDH
However, there are also psychological, social/environmental reasons for why people drink; this explains why pharmacological treatments are not particularly effective at reducing drinking
Disulfiram works psychologically as well as biologically; unless patients know they are taking disulfiram it does not work
PHARMACOLOGICAL TREATMENTS FOR SMOKING CESSATION – REPLACING THE SUBSTANCE
Pharmacological treatments for smoking cessation have a clear mechanism of action NRT replaces the nicotine that smokers get from smoking cigarettes
However, there are also psychological, social/environmental reasons for why smokers smoke; reviews show the effectiveness of pharmacological treatments is increased when delivered in combination with counselling
Stead et al. (2017) show that group counselling significantly increased abstinence rates relative to trying to quit alone.


