Physiology 1 22 Flashcards
There are two components to respiration what are they ?

The two compenents of respiration = Internal and External
External respiration = external environment to tissue
- Ventilation = bulk transport of external media across a gas exchange surface
- respiratory exchange - diffusion
- circulation
- cellular exchange
Internal respiration = cellular metabolism

What is Dalton’s law ?
Daltons law
- the partial pressue of gas
- the total pressure of a gas is equal to the sum of the partial pressures of the individual gases in a mixture
With altitude as the total pressure decreases, the partial pressure of a particular gas will decrease.
Partial pressure of oxygen = PO2
The partial pressure of any gas will change with environment.
What is Henry’s law ?
Henrys law
The amount of gas dissolved in a liquid is afftected by the gases partial pressure and solubility coefficient of that gas.
gas dissolved = pressure of gas in the media * solubility coefficient
- gas and liquid are in equilibrium
- only free gas molecules (physically dissolved contribute to the partial pressure of gas in liquid)
- gases will always diffuse down their partial pressure gradients.

What is Fick’s law, and what four factors affect the rate of diffusion ?
Describes the net diffusion rate of a gas across a fluid membrane.
- gases move down their partial pressure across a semi permeable membrane
Rate of diffusion
- surface area
- thickness or distance (T)
- pressure gradient (P)
- Diffusion coefficient (D)
What is Boyle’s law ?
Boyle’s law
For a fixed amount of an ideal gas kept at a fixed temperature, pressure and volume are inversly proportional.

What is tidal breathing and flow through breathing ?

Flow through breathing
- unidirectional flow of media, yeilds greater O2 uptake
- birds, fish and some crocodiles
Tidal breathing
- relatively inefficient as external medium moves in and out through the same opening
- mammals (bidirectional).
- fresh media is mixed with depleted media

Describe concurrent, cross current and countercurrent gas exchange ?
Concurrent exchange
- external medium and blood flows in the same direction
- partial pressure gradient declines
- does not exist in a biological system
Cross current exchange
- external medium and blood travels at right angles to each other
- diffusion occurs through-out declines gradually
- PO2 is higher in blood then external medium at the end
- birds
Coutercurrent exchange
- external medium and blood flows in the opposite direction and parallel to each other
- partial pressure gradient is maintained and diffusiin is constant
- fish highly efficient

Describe gas exchange in fish through the use of gills ?2
Gills
- countercurrent exchange system
- flow through
- at every point O2 is diffused into blood - great efficiency in gas exchange
- four gill arches - filaments - lamella
- large surface area which is proportional to how active the fish is
Buccal pressure pump - fish opens and closes mouth
Opercular suction pump - fish open and close opercular flaps

Describe the upper and lower respiratory tract, what are these systems purpose?

Upper respiratory tract
- located outside the chest cavity
- no gas exchange anatomical deadspace
- covered with mucus and ciliated epithelium
- trachea and bronchi supported by cartilage
- smooth muscle lines trachea, bronchi and bronchioles.
Function = conditioning of air (warm, humidification), and filtration muco-ciliary escalator
Lower respiratory tract
- alveolar surface thin layer of squamous epithelial cells (type one)
Contains three cell types
- Type one alveolar cell - assist in gas exchange
- Type two - large cuboidal produce surfactant
- Alveolar macrophage - phagocytic patrol the alveolar surface.

Hoe does air move into the lungs ?
By creating negative pressure. Increasing volume by contraction of the diaphragm and external intercostal muscles.
Describe the histological sections of the upper respiratory tract ?
Trachea = C shaped cartilage
Bronchi = cartiliginous plates
Bronchioles do not have cartilage
The amount of smooth muscle increase from the trachea to the bronchioles.

Describe the histology of the alveolar ?
Alveolar
- Alveolar surface covered by a dense capillary surface, lung interstitium has mast cells, connective tissue and elastic tissues to hold the alveolar open.
- mainly composed of type one alveolar cells - single layer of a single layer of sqaumous epithelial cells.
- Type two alveolar cells are cuboidal and secrete surfactant and the fluid layer which lines the lungs
- Alveolar macrophage

What effect does the parasympathetic and sympathetic nervous system have on the lungs ?
Sympathetic
- air way relaxation
- blood vessel constriction
- inhibition of glandular secretion through beta 2 receptors
Parasympathetic
- air way constriction
- blood vessel dilation
- increased glandular secretion
- vagus nerve

Describe the intrapleural space and the intrapleural pressure, and what they do?

Intrapleural space
- pleura anatomically seperates the lungs from the thoracic wall
- enables friction free movement between the lungs and the thorax
- lung is mechanically connected to the thoracic cage and pleura by the pleural fluid
- pressure of fluid is negative (intrathoracic pressure) holds the lungs open
- -3mmhg
- intrapleural space of the two lungs is seperated in most species
- cause for negativity is the mechanical interaction between the lungs and chest wall.
During quiet inspiration the intrapleural pressure becomes more negative, while during expiration it becomes less negative.

What is the intrapulmonary pressure (Palv) ?
Alveolar or intrapulmonary pressure is the pressure of the air inside the lung alveoli
Normal respiration alveolar pressure decreases to about -1 mmhg (inspiration) and rises to about 1mmhg during expiration.

What is the transpulmonary pressure ?
Transpulmonary pressure
Is the difference between the alveolar pressure and the pleural pressure (distending pressure)
- the more positive the distending pressure ptp becomes the more the lungs are distended or inflated
- ptp= Palv -Ppl

Describe Pulmonary ventilation in mammals ?
Inspiration
- diaphragm and intercostal muscles contract
- lung volume increases
- lung pressure decreases belwo atmospheric pressure
- air flows down its concentration gradient
- inspiration is always active as it requires muscle contraction
- 1-2% of the total energy metabolism
Expiration
- diaphragm and intercostal muscles recoil
- lung volume decreases
- lung pressure increases
- internal intercostal muscles may contract to assist with expiration
- passive process in rest

What is eupnea ?
normal quiet breathing
What is Hyperpnea ?
increased depth and frequency of breathing during exercise
What is Tachypnea ?
excessive rapidity of breathing
What is bradypnea ?
abnormal slowness of breathing
What is polypnea ?
rapid shallow breathing, as occurs during panting
What is dyspnea ?
Difficult, painful or laboured breathing - pathological
What is apnea ?
cessation of breathing, in clinic refers to transient state of cessation of breathing
What are adventitious sounds ?
crackles and wheezes abnormal sound superimposed on normal breath sounds.
Why do birds need a more efficient gas exchange system when compared to mammals ?
Birds are exothermic with a higher body temperature - 40-41 degrees
Highly active - flying high altitudes where the partial pressure of oxygen is lower.

How do birds achieve a greater efficiency in respiration when compared to humans ?
Greater efficiency of respiration in birds
- narrow diffusion distance air capillaries
- flow through breathing unidirectional
- cross current breathing

How does the bird’s respiration system work ?
Bird
- During inspriration both the anterior and posterior air sacs expand
- During expiration both the anterior and exterior air sacs deflate
- allows for flow through breathing
- lung relatively rigid and the air sacs act as bellows
- both inspiration and expiration are active even at rest
- respiratory muscles act upon the sternum to reduce or increase pressure within the air sacs
- air exchange occurs in the parabronchi ( air capillaries)
Requires two cycles to move a single bolus of air through the entire system.

What is lung compliance ?

Lung compliance is a measure of how much force is required to distend the lung.
- the greater the change in volume, with a smaller force = greater compliance
- lung and thoracic structures
- alveolar surface tension

Why is the surfactant produced by type two alveolar cells so crucial ?

Surfactant
Surface tension acts to reduce the surface area collapsing the alveolar.
Surfactant reduces surface tension .
- prevents alveolar from collapsing
- reduces effort to expand lungs
- prevenst adhesion of adjacent respiratory surfaces
Barker syndrome = in piglets and horses is caused by too low a production of surfactant during gestation. The animal requires excessive force to extend lungs and rapid expiration.

What is a restrictive disease of the lungs, provide an example and type of breathing pattern this will generally cause ?
Restrictive disease
- results in restriction of lung expansion
- pulmonary fibrosis - progressive scarring of the lungs seen in older terriers
- causes rapid shallow breathing
What is an obstructive lung disease, provide an example and what type of breathing pattern this will generally cause ?
Obstructive lung disease
- Causes obstruction within the airways - decreasing airway diameter
- decrease in airway diameter occurs during expiration (due to positive intrapleural pressure)
- expiratory dyspnoea
- animals abnormally slow and deep breathing pattern.
Examples
- Heaves in horses = hypersensitive to allergens
- Feline asthma inflammation and constriction of the bronchioles

In a spirogram we can obtain four lung volumes of TV, IRV, ERV and RV difine these volumes.
The four volumes obtained in a spirogram.

Tidal volume (TV or VT) = volume of air inhaled or exhaled per breath
Inspiratory reserve volume (IRV) = amount of additional air that can be taken into the lungs after a normal inspiration.
ERV = amount of additional air than can be taken from the lungs after a normal expiration.
Residual volume = amount of air remaining in the lungs after maximal expiration (can not be measured by spirometry).
Describe what will happen if lung compliance becomes abnormal ?

Higher than normal compliance
- Lung inflates easily but due to reduced elastic recoil it becomes difficult to expire
- emphysema
Lower than normal compliance
- Requires increased force to expand alveoli
- pulmonary fibrosis

Define the four lung capacites inspiratory capacity, functional residual volume, vital capacity and total lung capacity obtained in a spirogram ?
Four lung capacity
Inspiratory capacity = IRV + TV
Functional residual capacity = ERV + TV
Vital capacity = ERV + IRV + TV
Total lung capacity (TLC) = VC + RV
Define PEFR and PIFR ?
Peak flow rate can be taken as a quick measurement and is useful to monitor obstructive diseases.
PIFR = Peak inspiratory flow rate
The fastest flow rate achieved during inspiration
PEFR = Peak flow rate achieved with maximal force during expiration after a complete inspiration.
Define minute ventilation ?
Minute ventilation
Minute ventilation = The volume of air breathed in or out within one minute.
mV = RR * TV
- increases during physical activity
- gives the volume flow throughout the entire respiratory tract including lungs
Define respiratory dead space, anatomical dead space, and physiological dead space ?
Respiratory dead space = air that enters the lungs but dose not participate in gas exchange.

Anatomical dead space = air which fills conducting airways, conditioning, thermoregulation
Alveolar dead space = gases which enter the alveolar but do not participate in gas exchange eg no perfusion.
Physiological dead space = alveloar dead space + anatomical dead space
In a normal healthy lung the physiological dead space = anatomical dead space as a healthy lung has no alveoli dead space.
Define alveolar ventilation ?
Alveolar ventilation accounts for the fact that not all minute ventilation contributes to gas exchange
Alveoli ventilation = (TV - dead space volume) * RR
It is the rate at which the alveolar air is replaced by atmospheric air.
What is the Va / Q ration and why is it important in respiration ?a
For gas exchange to occur efficiently the ventilation of th lungs to perfusion ratio must be matched
Va / Q = 1 Maximum gas exchange
- If perfusion of the lungs increases the bronchioles, alveoli will dilate in response to increase ventilation: and vice versa
- local control mechanisms
- bronchiole dilates - arterioles dilate
- bronchiole constricts - arterioles constrict
Mismatching of the Va and Q are the main causes of hypoxemia

What happens during mismatching of ventalation and perfusion, and provide an example ?

Ventalation Va and perfusion Q mismatching occurs in abnormal conditions
- healthy perfusion ventilation ratio = 1
- as the degree of mismatching increases, O2 exchange becomes less efficient
- most common cause of hypoxemia decreased 02 in the blood
Eaxamples
- Shunt = blockage of the airway (mucous plug) so perfusion without ventilation
- embolism = blockage of an artiole ventilation without perfusion

Why would impairment of partial pressure gradient affect 02 but not CO2?
Diffusion coefficient is higher in CO2, than O2

Describe how O2, and CO2 are transported around the body and it what proportions ?
Blood needs to carry more gas than can dissolve in plasma.
Oxygen is carried in two forms
- bound to haemoglobin 98.5%
- unbound dissolved 1.5%
Carbon dioxide is carried in two forms
- carbaminohemoglobin (3) as bicarbonate form
Oxygen bound to hemoglobin dose not contribute to PO2
- this maintains oxygen gradient in the lung
- the amount of Hb in blood determines the oxygen carrying capacity of blood
- each HB molecule binds four O2 molecules when fully saturated

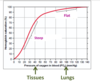
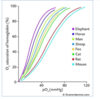
What shape is the hemoglobin oxygen disociation curve, why dose the flat part occur ?

The oxygen haemoglobin dissociation curve is sigmoid in shape.
The saturation of HB is related to the PO2 of the blood
The flat part
- Favors loading of oxygen and is due to a high PO2
- occurs in the lungs
- no significant change in % saturation between 60 - 100 mmHg
- at normal PO2 complete saturation of hemaglobin occurs
- large plateau of curve provides a large safety margin.
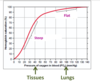
The sigmoid oxygen haemoglobin dissociation curve has a steep part why dose this occur.
Steep part
- curve shows steep decline in % saturation between 40 to 10 mmHg
- helps dissociate oxygen from the haemoglobin molecule
What four factors affect the affinity of Hb for O2, how would these facotors be changed to cause a decrease in affinity ?
The four factors
- temperature
- PH
- 2,3 DPG
- PO2
To cause a decrease in affinity
- temperature increases
- PH decreases
- 2,3 DPG increases
- PCO2 increases
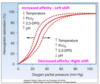
What is the BOHr affect ?
An increase in carbon dioxide in the blood and a decrease in PH results in a reduction of the affinity of haemoglobin for O2.

What affect will exercise have on the oxygen - haemoglobin dissociation curve why dose this occur ?

Exercise
right shift of sigmoid curve decreased affinity - favoring unloading of oxygen to the tissues
note = at rest only 25% of oxygen bound to HB is released to the tissues in one circuit - so there is a large reserve of oxygen for increased metabolic rate.
Factors
- PO2 reduced metabolically active tissues / reduced saturation of HB 10-40mmHG
- CO2 increases in tissues
- acidity increases
- when tissues need more they get more

Dose the form of haemoglobin vary, and why would this occur ?
Haemoglobin form varies between species and life stages
Animals have varying form of Hb suited to their metabolic rate and environment
- small animals with fast metabolism have HB with low affinity - favoring oxygen unloading in tissues
- animals at high altitudes - HB higher affinity of for oxygen as the partial pressure of oxygen is lower
- The effect of CO2, H+ causes different affects on HB depending upon its form
- effect of 2,3 DPG varys depending on form
- Fetal HB often has a lower affinity for oxygen than in its adult form.
Describe the diffusion of oxygen at the tissue level ?
O2 diffusion tissue level
- Tissue PO2 at rest = 40 mmhg
- partial pressure of O2 systemic 100 mmhg
- partial pressure gradient = 60 mmhg
Oxygen diffuses from blood into the tissue down its partial pressure gradient.
Tissues with a higher demand for oxygen will be more highly vascularised.

Describe the diffusion of CO2 at tissue level ?

Tissue diffusion of PCO2
- tissue partial pressure = 45mmhg
- systemic blood partial pressure = 40mmhg
CO2 moves into blood from the tissues down its partial pressure gradient

Describe the three forms carbon dioxide is transported in, within the blood ?
- Bicarbonate 60%
- Bound to HB 30%
- Dissolved 10%

What does carbonic anhydrase do?
Carbonic anhydrase located within red blood cells
- CO2 + H2O - H2CO3 - H+ and HC)3-
- Carbonic anhydrase converts CO2 into HCO3- within the red blood cell close to the tissue
- This liberates H+ ions (increasing acidity) which bind to HB causing the further release of O2 (Bohr effect)
Chloride shift = the HCO3- ions are transported out of the cell in exchange for CL-
Note the reverse happens at alveoli.

What is the Haldane effect ?
Haldane effect
- CO2 binds to a different site then oxygen = CO2 binds to the globin site where as O2 binds to the heme component.
- removal of oxygen from HB in tissues increases affinity for CO2 - favouring the loading of CO2 in tissues