Histology Flashcards
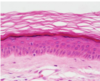
Name the three layers of the skin
- Epidermis
Keratinised stratified squamous epithelium
Keratinocytes = true epithelial cells
- Dermis
Dense irregular connective tissue
- Hypodermis
Addipose tissue

Explain how you would distinguish between thick and thin skin?
Thick skin
- lacks hair follicles
- nasal planum, footpads
- has both stratum lucidum and stratum corneum layers
Thin skin
- most frequent and is usually haired
- no strtum lucidum

Identify all five layers of the epidermis ?

- Stratum basale
- Stratum spinosum
- Stratum granulosum
- Stratum lucidum
- Stratum corneum

Identify and describe the Stratum basale ?

Stratum basale
- single row of cells sitting on a basement membrane
- stem cells undergo mitosis

Identify and describe the Stratum Spinosum ?

Spinosum
- cells have spines projecting (cytoplasmic extension) and attach to each other via desomeres

Describe and identify the Stratum Granulosum ?

Stratum Granulosum
- keratin accumulates in cells
- contains keratohyaline granules - start to bind keratin together and Lamella granules - water proofing

Describe and identify the Stratum Lucidum ?

Stratum Lucidum
- contains a protein which has a different staining affinity
- above granulosa layer, only in thick skin
- flattened dead cells of poor staining quality

Describe and identify the stratum corneum ?

Stratum Corneum
- consisting of dead accumulated, anucleated squamous cells containg keratin
- layers depend upon the site of tissue

Explain what the epidermis is composed of and where it is located ?
Epidermis
- the most superficial layer of squamous epithelium
- accompanied by other cell types for pigmentation, sensory perception and immune function
- derived from ectoderm layer of the trilaminar germ disc.
Keratinocytes = true epithelial cells
Describe Langerhans cells their location, function and structure ?
Langerhans cells
- found at the level of the stratum spinosum
- involved in immune function
- function as antigen presenting cells and may stimulate T cell responses in various allergic or inflammatory responses
- well characterised in humans and rodents

Describe what melanocytes do, their location and function ?
Melanocytes
- reside in the stratum basale layer of the epidermis
- originate in the neural crest of the ectoderm
- pigments may travel from basal layers to upper layers through specific processes - eventually phagocytosed by keratinocytes
They function to absorb and scatter UV radiation thus decreasing mutagenic effects

Describe the dermis, its location, composition and two layers ?
Dermis
- Located beneath the epidermis
- able to withstand certain mechanical stressers as it is both flexible and elastic
- thick layer of connective tissue
- dense irregular connective tissue
- contains blood vessels, lymphatics and inflammatory cells (histamine and heparin).
- develops from mesoderm of the trilaminar disc
Papillary layer = fine collagen fibres richly supplied with cappillaries
Reticular layer = Highly thick collagen bundles

Describe the location and composition of the Hypodermis ?
Hypodermis

The majority of the tissue is composed of adipose
but there are also, sweat glands, hair follicles, large vessels, nerves and lymphatics, skeletal muscle, mammary glands etc
Sebacious glands what do they produce, where are they located and what are they derived from ?

Sebacious glands (holocrine)
- derived from the epidermis
- solidly packed cells with a foamy appearance
- produce sebum an oily product that waterproofs or softens the hair
- glands empty into upper regions of hair follicles
- all the contents of the cell are lost to the cells surface

Describe hair follicles origin, and accompanying cells.

Hair follicles
Specialised down growth of the epidermis that extends deeply into the dermis and hypodermis
- hair growth originates at the bulb
- melanocytes provide pigment to matrix cells which are eventually formed into hard keratine
- arrector pilli muscles = smooth muscle attached to root sheath allow hair to become erect when cold

Identify the dermal root sheath, external root sheath, internal root sheath, hair and cuticle in a hair follicle ?

Describe the three stages of hair growth Anagen, Catagen and Telogen ?
Anagen
- Growth phase
- Dermal papilla (uppermost layer of the dermis) reattaches to a new hair follicle
- older hair pushed out by the growth of a new hair follicle
Catagen
- The dermal papilla detaches and rests, while the hair shaft is freed from the blood suplly and pushed upward
Telogen
- Dermal papilla reattaches to new hair follicle (Dose not grow)

Describe Apocrine glands and what they produce ?
Apocrine glands
- located throughout the skin of most domesticated animals
- empties into upper part of hair follicle
- simple cuboidal epithelium, coiled glands
- not true sweat glands produce = viscous fluid, sexual attraction, communication, territorial marking
- excretes a small portion of the cell contents and secretion

Describe Merocrine sweat glands and what they produce ?

Merocrine sweat glands ?
- simple cuboidal or columnar epithelium
- produce aqueous sweat for thermoregulation
- open directly onto the surface of the skin
- only secretion is lost to the cell surface
Found
- footpad of dog and cat (picture attached)
- frog of horse
- planum rostrale and carpal glands of pig
- nasolabial region in cattle

Describe the blood supply to the skin ?

Describe the formation of hooves, horns and claws ?
Hooves, horns and claws

Same structures as thick skin
They differ through the shape of the papillae / lamellae that extend from the dermis
Flat papillae = form flattish thick skin
Shaped papillae = form keratinised columns hooves, horns and claws
The hoof/ horn is held to underlying tissues through laminae
Identify the three layers of skin in a pigs ear, what features make this a thin skin classification ?

Pig ear thin skin
Thin skin as it lacks a stratum lucidum layer and contains many hair follicles
- blue = hypodermis
- pink = dermis
- purple = epidermis
Identify the four layers of the epidermis in the thin skin of a pigs ear ?

Epidermis
yellow = stratum basale
blue = stratum spinosum
green = stratum lucidum
orange = stratum corneum
Identify the five skin layers in a dogs paw pad, what characteristics make this thick skin ?

Dog paw pad
This is thick skin as it has an incredable thick keratinous layer composed of stratum lucidum and stratum corneum (usually lacks hair follicles)
yellow = stratum basale
blue = stratum spinosum
green = stratum granulosum
purple = stratum lucidum
orange = starum corneum

Describe the nasal cavity regions and what structures maintain its shape ?

Nasal cavity
The structure is maintained by bone and cartilage of the nasal bones (maxillary, incisive, ethmoid and frontal) with the cartilage of the chonca. The left and right side is divided by the nasal septums.
Three regions of the nasal cavity
- Rostral (Cutaneous) - comprised of stratified cuboidal to non - ciliated pseudostratified columnar
- Respiratory (caudal to thirds) ciliated pseudostratified columnar epithelium
- Olfactory (dorsocaudal) ciliated pseudostratified columnar epithelium with olfactory epithelium
Describe the specialisation of the ethmoid choncae within the respiratory system ?

The ethmoid choncae contains specialised olfactory epithelium
- Respiratory epithelium specialised for olfaction
- located near the ethmoid and the roof of the nasal cavity
- Bowmans capsule = moistens olfactory mucosa
- Olfactory cells long cilia contain receptors
- Sustantacular cells = supportive cells of olfactory epithelium
- Basal cells = stem cells

Describe the histology and identifying features of the trachea ?

Trachea
- C rings of hyaline cartilage
- pseudostratified columnar epithelium
- Trachealis muscle contracts during coughing to increase intrathoracic pressure
- large submuscosa contains specialised glands (seromucous glands)
- goblet cells = secrete mucous
- Cilia = moves mucous cranially
- laminar prpria lie below the epithelium and is greatly vascularised.

Describe the distinctive histological features of the Bronchi?

Bronchi (primary to secondary)
- irregular plates of cartilage in wall
- smooth muscle which surrounds the laminar propar
- depper the cartilage plates become less regular
- the number of glands decrease with increasing depth into the long

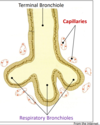
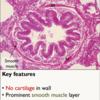
Describe the histological features of the Bronchioles ?

Bronchioles
- no cartilage in walls
- deeper at this level the epithelium becomes simple columnar
- contains club cells
- terminal bronchioles transition to respiratory bronchioles when alveoli begin to appear on the slide.
What do club cells do and where are they located ?

Club cells are located within the bronchioles
- dome shaped cells with short microvilli
- detoxifies cytochrome P450 enzymes which break down air born toxins
- act as stem cells to replenish bronchiloar epithelial cells

Describe the histological features of the alveolar, and the three cell types ?

Alveoli
- honeycomb arrangement
- abundant capillaries, supported by collagen and elastin fibres
Type one pneumocytes
- simple squamous cells
- thin to allow for diffusion
- close opposition to capillaries
Type two pneumocytes
- cuboidal cells
- produce surfactant to decrease surface tension
- stored in lamella bodies (granules)
- can also act as stem cells replacing type one and two pneumocytes
Alveoli Macrophages
- immunity against irritants, microbes and particulate matter via phagocytocis

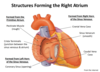
Describe the three layers of the heart wall ?

Heart wall
- Endocardium
simple squamous and dense irregular connective tissue
- Myocardium
cardiac muscle - striated, single centered nucleus, intercalated disks, branching
under involuntary nervous control + contains perkinje fibres
- Epicardium (visceral pericardium)
squamous epithelium
loose connective tissue and elastic fibres containing the blood supply and nerves which innervate the heart

Identify the layers of a artery ?

Tunica intima
endothelium - simple squamous lines the entire vascular system
subendothelial layer
internal elastic lamina
Tunica media
smooth muscle layer
external elastic laminar
Tunica adventitia
contains vaso vasorum

What is the vaso vasorum and where is it located ?
Vaso vasorum
- located in the Tunica adventitia
- network of small blood vessels which supply oxygen and nutrition to large blood vessels.
What are purkinje fibres, and where are they located ?
Purkinje fibres
- modified myocytes
- observed between the endocardium and myocardium of the heart (also in myocardium)
- transmit and distribute action potentials from the atrioventricular node
Describe the dfining histological features of an elastic artery ?

Type one, Elastic artery
- The largest arteries including the aorta, common carotid
- Tunica intima is thicker - than in other types of arteries (contains subendothelial layer)
- Tunica media 10-40 layers fenestrated layers of elastin
- Tunica adventitia contains vas vasorum.

Define the histological features of a muscular artery ?

Type two Muscular artery
- Main distributing branches of the arterial tree eg radial, femoral, coronary artery
- Tunica intima - very thin
- obvious internal elastic lamina
- Tunica media - contains alot of smooth muscle and less elastic fibres
- obvious external elastic laminar
- Tunica adventitia - variable thickness contains vaso vasorum

Define an arteriole through histological features ?
Arteriole
- similar histologically as a muscular artery but the small size makes the various layers difficult to discern.
- act as sphincters to regulate blood flow to various regions of the body
- tunica media only 1-2 layers of smooth muscle
- elastic laminae may be absent
- tunica adventitia is thin

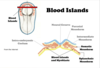
Define the histolical features of a capillaries?
Capillaries
- Tunica intima only
- endothelial cell enclosed by a basement membrane
- lacks tunica media and tunica adventitia
- slow blood flow
- huge cross sectional surface area
- caontain periocytes - contractive cell

Describe the three types of capillaries ?

Identify the histological features of a vein and how this compares to an artery.

Vein
- returns blood to the heart
- Tunica intima - contains endothelium and endothelial layer (connective tissue + basement membrane)
- Tunica media - smooth muscle much thinner than in an artery
- Tunica adventitia - layer of connective tissue containng the vaso vasorum in larger veins
- > 2mm veins contain valves
*

Describe the how various histological features varie as veins become closer to the heart ?

Variations
- thickness of wall
- pressence or absence of valves
- amount of elastin and smooth muscle

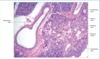
Identify the structures (7) ? and tissue ?

Lymph node
- afferent lymphatic vessels - entering the lymph node through the capsule
- efferent lymphatic vessels - receive lymph from the medullary sinus eventually rejoining the lymphatic system
- Subcapsular sinus - the space that encircles the lymph node beneath the capsule into which lymph from the afferent vessels drain
- Trabecule - extensions of the outer capsule projecting into the the substance of the lymph node
- lymphoid follicles
- medullary sinuses - located in the central region they receive lymph from the subscapular and cortical sinusesand converge on the hilum of the node
- hilum

What is a periocyte ?
Periocyte
Periocytes surround the endothelium of capillaries. They are contractile and regulate blood flow through the capillarie beds.

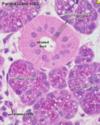
Identify the two layers of a lymphoid follicle ?

Lymphiod follicle
- Mantle zone - outer layer
- The darker staining periphery of the lymphoid follicle where there are numerous T - lymphocytes (cell mediated immunity)
- Germinal centre - inner layer
- The pale staining centre of the lymphoid follicle where B lymphocytes are stimulated to proliferate by contact with an antigen. (Humeral immune response produce antibodies.

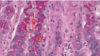
Identify this organ and all its histological features ?
The spleen
Is a large lymphiod organ that receives a rich blood supply. It provides a region where the blood can come into contact with lymphocytes - similar to the lymph nodes for lymph.
- Capsule - a thin fibroelastic coat surrounding the spleen
- Trabeculae - extension of outer capsule projecting into the substance of the spleen
- Red pulp - forms the bulk of splenic tissue filled with erythrocytes + rich in macrophages
- White pulp - pale staining lymphoid aggregates simlar to follicle in lymph node
Two types
- germinal layer - B lymphocytes
- mantle layer - T lymphocytes

Identify this tissue and its distinctive histological features ?

Tissue = muco-cutaneous junction
Orange = muco-cutaneous junction
yellow = orbicularis oris (skeletal muscle)
green = hair follicle
Blue = keratinised stratified squamous epithelium
purple = non keratinised stratified squamous epithelium and seromucous salivary gland.

Describe the muco-cutaneous junction, and where is this found ?
Muco-cutaneous junction
Junction between the integument and the digestive system
- found lips, nose, eyes and nose
- in ruminants unlike other species the oral cavity is lined by keratinised stratified squamous epithelium - due to the large amounts of roughage in their diet

Identify this tissue, and its defining histological features ?

tongue
It is a muscular organ covered by a mucosa and can move in all directions.
- dorsal thick keratinised stratified squamous epithelium
- Ventral thin keratinised stratified squamous epithelium
- intrinsic muscle fasicles run in all different directions.
Four types of lingual papillae
- Filiform - mechanical
- Fungiform
- Foliate
- Circumvallate
Describe structure, location and function of Filiform papillae ?

Type 1 = Filiform papillae
Covering dorsal surface of the toungue most common type
- purly mechanical and protective
- assist with prehension and grooming
- move and shape food bolus for swallowing

Describe the structure, function and location of fungiform papillae ?
Type 2 Gustatory = Fungiform papillae
- mushroom shaped
- rise above the surface of the tongue
- scattered amongst the filiform papillae on the dorasal surface of the tongue.
- non-keratinised stratified epithelium

Describe the structure, location and function of Foliate papillae ?
Type 2 Gustatory Foliate papillae
- These are leaf shaped
- They are located around the sides of the tongue (parallel folds)
- absent in ruminants, no taste bud contained within in the cat

Identify the structure, location and function of the Circumvallate papillae in the toungue ?

Type two gustatory Circumvallate papillae
- surrounded by a mote
- largest type of papillae
- 3-6 rostral to the root of the tongue
- taste buds located in the wall of the papillae
- contains the majority of the taste buds

Provide the general structure of a tooth ?

Tooth
Outerlayer enamel
- produced by ameloblasts (96% mineral hydroxyapatite crystals + 1% proteins amelogenins enamelins)
Inner layer dentine
- avascular, acellular connective tissue - type one collagen
- produced by odontoblasts external to the hard dentine
- surrounds pulp cavity of the tooth
- odontoblasts
Below the gum Cementum
- cementoblasts
- covers the root dentine
- similar to bone
Periodontal ligament
- anchors the tooth to the alveolar bone and absorbs shock

Describe the difference between a Brachydont and Hypsodont tooth ?
Brachydont
- short
- stop growing post eruption
- carnivore, human
- low crown
- narrow canal
Hypsodont
- long teeth
- grow for a portion or throughout the entire life of the animal
- high crown
- horses, cheek ruminant

Describe the development of the teeth ?

Tooth development
Enamel can not be repaired but dentin is repairable
Ameloblasts
- produce enamial
- lie external to the enamel
- degenerate when tooth erupts, so repair to damaged enamel later in life is impossible
Odontoblasts
- are external to the hard dentine
- have long slender cytoplasmic processes that penetrate the width of the dentin and run in canals (tubules)
- these processes are embedded in the secreted matrix
Cementoblasts
- cementocytes live with in the lucunae within the lower root
- cementum is laid down through out life
- collagen fibres laid down with in the cementum which eventually forms the peridontal ligamnet.