Phillips - Pregnancy Flashcards
What things need to happen to make L and D successful?
- Review records for medical problems, risk factors: ex, GBS+ patient will get penicillin during labor
- Routine labs: CBC, type/screen for blood products
- IVF: D5LR for fluid replacement
- Anesthesia consult for epidural: discuss this prior to delivery (bedridden following administration)
1. NO total pain relief, so pts should be ready for some degree of pain and discomfort - Pitocin (dilute solution) almost routine: promotes normal contraction pattern (pts may abstain)
- NPO in labor process, but frowned upon in some more “natural” settings: DEC risks w/ anesthesia
- Comfort, and questions answered
What kind of monitoring is done during a typical L and D?
-
Fetal monitoring: external monitors continuously
1. Freq review of fetal heart tracing: most units have central monitoring capacity via a screen w/all laboring pts and fetal HR at that time - Periodic exams (of cervix) for progress: try to keep these at a MINIMUM because more exams lead to INC risk of infection
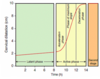
What do you see here?

- Intrapartum fetal (top) and contraction monitoring
-
FHR: baseline 132 bpm; moderate variability (normal: external monitoring)
1. Qualitative, not quantitative if external
2. Quantitative FHR on time: variability normal, even acceleration (going way above baseline) -
Contraction pattern: q3-4 minutes (normal)
1. Dark, vertical bars designate 1 minute so you can count how frequent the contractions are
2. #’s on vertical axis give you some basic info concerning contraction strength -> this can’t be measured via external monitor (body habitus), so internal monitoring via catheter in uterus can be used for better values
What is the typical recovery time for a vaginal birth?
- Recovery 24-36 hours on floor, then discharge
- Depends on pt energy level, and what kind of help she has at home
What is the estimated blood loss in vaginal birth?
- 500cc
- Very normal, considering that pt goes into labor process with 40-50% excess cardiac volume
What is an episiotomy? Is it routine in vaginal birth?
- Episiotomy: incision in vagina to allow room for baby to come out
- NOT routine, although it was in the past
What happens to the baby post-L and D?
- Baby in room with mom!
- Mom should be responsible for caring for baby from delivery on (with exception of small amount of time in nursery for routine blood work, etc.)
- Breastfeeding IMPORTANT
What are the indications for Cesarean birth (10)?
- Malpresentation of the fetus (breech): anything other than the head
- Failure to dilate/descend: understand labor curve, and have same person examine pt time and again (pt can’t be in labor forever)
-
Abnormal fetal heart tones: might predispose baby to lack of oxygen and acidemia, which pose risks of cerebral palsy and brain damage
1. Monitor to prevent these, and do cesarean earlier rather than later (malpractice, yo; cerebral palsy actually more complicated) - Some birth defects: NTD babies better off with cesarean delivery; gastroschisis babies CAN be born vaginally (doesn’t matter)
- Previous C-section or scarred uterus: MOST COMMON REASON -> safe to attempt vaginal birth after 1 C-section, but risks to fetus and mother of uterine rupture (risk 1%, so women given choice)
- Triplets or higher: twins can be born vaginally or cesarean, depending on presenting fetus -> if 1st is vertex, vaginal delivery; if breech, then cesarean
- Active herpes simplex virus at due date: neonatal herpes happens as baby is passing through vagina where lesion is present, producing virus -> women given prophylactic anti-virals at 26 wks gestation, so less likely moms will have outbreak near term
- High viral load and HIV: if comes in with labor or ruptured membranes, fetus already exposed, and no advantage to cesarean birth
- Placenta previa: usually implants high, but if low, then covers cervical os, and C-section necessary -> high risk for bleeding, and can be emergency, requiring hysterectomy, or causing maternal death (placenta can bleed as cervix dilating)
- Patient request: remind pt there are risks assoc w/major sx, but most physicians honor this request
How common is C-section?
- Quite common:
1. <1/4th at public hospitals
2. May be up to ½ in some private hospitals - INC rate in previous decades
What do you see here? What do you want to do?
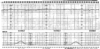
- FHR w/baseline of 170 bpm, minimal variability
-
Late deceleration: following contraction, slight downward trend of FHR, then slope upward
1. Indication that fetus might be becoming hypoxic and acidemic
2. Indication for expedited cesarean delivery to get baby out as soon as possible
How are incision/closure decided in C-section?
- Abdominal and uterine incision type depends on indication
- Type of closure and suture according to best evidence and surgeon preference
- Don’t really need to know details about these things yet
What MUST be given in the case of a C-section?
- ANTIBIOTICS REQUIRED to prevent surgical site infection
What is the estimated blood loss (EBL) in C-section? Recovery time?
- EBL: 1000cc
1. Some pts come into process with low Hct or anemic, and may need blood transfusion with this much blood loss (even though this is normal for this type of procedure) - Recovery time 24-48 hours: usually go home on post-op day 2
What are some complications associated with C-section?
- Hemorrhage
- Surgical injury to bladder/bowel: can occur
- Surgical site infection: give AB’s intra-operatively to try and prevent this
- Adhesions: prone to these, as are all pelvic surgeries
- Need for repeat CD: adhesions can present real problems in subsequent C-sections for both mom and baby (in terms of trying to get baby out)
- Try to avoid cesarean delivery if possible b/c great deal of morbidity and mortality associated
What counseling should happen post-partum (5)?
-
Lochia: vaginal bleeding/discharge persists 3-8 wks -> heavy + bloody initially, like a period; tell pt!
1. Occasionally a heavy bleed at day 7-14 pp b/c eschar (scab) at placental site sheds; warn pt this is NOT a menstrual period
2. Exercise, sex, driving, work can resume when pt is comfortable (except in extreme circumstances) - Birth control can be addressed, given in hospital
- Breastfeeding encouraged, supported in hospital and in post-partum period with lactation advisers
- Baby care: neonatology folks usually come by, and suggest 2-week return visit
- Warnings about depression: baby blues common, but depression a very serious issue -> seek attention if there are any concerns
What is post-partum depression?
- DSM-classified mental illness
- >10% of women have depression w/in first 3 mos post-partum
-
Different than ‘baby blues,’ which have to do with excitement of delivery fading, and “cheerleaders” leaving mom to fend for crying baby by herself
1. Women usually come to grips with this sort of scenario and recover just fine
What are the risk factors for post-partum depression?
- Previous episodes
- Inner city women
- Mothers of preterm babies
- Adolescent mothers
- NOTE: life stresses might make you more prone, but this illness affects people of ALL SES and ethnic gps
What kind of screening is done for PP depression?
- Routine screening on ALL moms: Edinburgh Depression Scale
- Pediatricians sometimes recognize this before OB/GYNs, who don’t see moms until about 6 wks (peds sees them at 2-4 weeks)
- Important for baby that the mom is not depressed, and care for/feeding of baby can be impacted
1. BONDING - Moms may also present to OB with specific complaints of trouble coping
What is the physiologic basis for PP depression?
- Withdrawal of hormones at delivery may be what pushes people into these depressive episodes
- People with predisposing mental illness more prone to these types of problems
What are the symptoms of PP depression?
- Crying
- Helplessness
- Exaggerated worry about baby: may stay awake to watch baby breathe
- Sleeplessness: exhaustion, crying, feeling of helplessness
- Different than baby blues, which is a realization that life is forever changed, frustrated with new duties or lack of support
What are the biggest concerns in PP depression?
- Biggest concern for baby is lack of bonding at a critical time
- Psychosis, suicide, even homicide are the biggest concersn for the mom
1. This is extreme, but it has happened
PP depression dx and treatment?
- SSRIs (Sertraline): works, safe, can be used during breastfeeding -> benefit far outweighs the risk
- Continue breast-feeding: crucial for bonding process to continue, and mom to climb out of this “helpless” state
- Frequent OB visits: seldom need psychiatric care, unless severe or has pre-existing disease, in which case they would get back with routine counselor
- Hospitalization sometimes necessary: pt will often tell you that she needs this to detach completely, recover, and come back
-
Symptoms usually remit around 8 weeks post-partum, but may continue to 3 months and beyond
1. Pt may need assistance with psychiatrist if anything out of the ordinary
Physiology of lactation during pregnancy?
- Progesterone influences growth in size of alveoli and lobes of breast tissue
- Estrogen stimulates the milk duct system to grow and differentiate
- Prolactin causes differentiation of the alveoli and ductal structures
- Human placental lactogen (HPL) produced by the placenta, and causes breast, nipple, areola to grow
What are the benefits of breast feeding for the infant?
- Passive immunity: fully functional IgA, IgG and IgM passed from mom to baby, preventing infections, and starting baby off on good foot
-
Nutrition: formula-fed have higher, faster weight gain in newborn period and INC # of fat cells (these never go away)
1. Protects against obesity - Protects against allergies/asthma
- Bonding: helps produce confident infant and child
What are the benefits of breastfeeding for the mother?
-
Natural contraception as long as mom is fully breastfeeding, even for months post-partum
1. Will not ovulate until starts supplementing, & PRL levels go down in intermediary periods - Weight loss
- Some evidence it protects against breast cancer
- Bonding
What is the physiology of prolactin in lactation/breast devo? Release? Function?
- Pregnancy: level of prolactin INC 10-20x
- Delivery: progestin, estrogen levels drop, and INH of PRL hormone removed -> milk production begins
- FUNCTION: promotes casein mRNA transcription
1. May stimulate syn of alpha-lactalbumin, the regulatory protein of the lactose synthetase enzyme system
2. INC mammary gland lipoprotein lipase activity
3. Regulates milk production via osmotic balance at the membrane - Levels DEC as nursing becomes established, but nursing itself stimulates episodic production of PRL to keep process of milk production going
What is the physiology of oxytocin in lactation?
- Produced by post pit; contracts smooth mm layer of band-like cells surrounding the alveoli to squeeze the newly produced milk into the duct system (out from the alveoli)
- INC maternal GI mobility and nutrient absorption so she can make the most of breast feeding (promotes nutrition)
- Necessary for milk ejection reflex, or let-down, in response to suckling
- Anti-stress effect: increase bonding (can relax and enjoy nursing)
What is the colostrum? Contents?
- Colostrum from breast in first few days of nursing, NOT breast milk -> low vol, high nutritional content
1. Perfect for immature gut of newborn b/c simple in construction and low-volume - CONTENTS:
1. Very rich in proteins, Vit A, and NaCl
2. Lower amts of carbs, lipids, and potassium than mature milk (simpler formulation)
3. Growth factors (stimulate devo of the gut), anti-microbial factors, Ab’s of passive immunity
What is breast milk composed of? Does maternal diet affect this?
- Glucose is the major substrate for breast milk
- Glucose, amino acids, and minerals delivered to the milk from maternal circulation
-
Lipid content rises throughout nursing episode: the longer the baby nurses, the higher the lipid content in the breast milk
1. Protein stays the same - Maternal diet variation causes NO variation in milk components (or their concentrations)
How does breast feeding affect mom?
- Nursing itself INC blood flow to the breast by 20-40% so more nutrition can get directly to the breast and into breast milk
- Maternal cardiac output goes up, and vasodilation occurs from oxytocin
When is breast milk present? What permits its release post-delivery?
- Breast milk is present by mid-pregnancy: women don’t lactate or leak breast milk until baby is born
- Progesterone drops at delivery, and PRL (from pit gland) increases -> milk production
- Breast engorgement: 2 days postpartum
How is oxytocin involved in milk let-down?
- Release from post pituitary gland causes breast myoepithelial cells to contract and release milk
1. Causes uterus muscle cells to contract too, involuting uterus, and reducing bleeding as the mother nurses - Released through a somatosensory pathway initiated by neonatal suckling -> breastfeeding begets milk production (when they stop feeding, milk production stops)
- Remember: pitocin (oxytocin) given to women in labor to help augment their contraction pattern
What has stimulated INC rates of breastfeeding in Memphis?
- Breast feeding coalition -> OB’s now educate the patients that breastfeeding is expected
1. No longer say, “would you like to breastfeed or bottle feed;” expectation is breastfeeding - Educate family members in spite of potential (-) comments or feedback: want mom to feel comfortable breastfeeding
- Provide support for new moms: teams of lactation consultants -> has worked!
Why is breastfeeding a “hard sell” for some communities? How can we change this?
- BARRIERS: stigma, fear, pressure to bottle feed, esp. with young women that are eager to get back to school or work
- EDUCATION: baby benefits from improved neonate nutrition, protection against obesity, some infections, allergies and asthma, BONDING
1. Benefits to mom include convenience, weight loss, protection against breast cancer, and BONDING
2. Requires support- antepartum by doctors (Not “are you breast or bottle feeding?” like it is an even choice; but. “Breast feeding is best for the baby, so I assume you are breast feeding.”)
3. Lactation nurses postpartum: in hospital and beyond
What is Sheehan syndrome?
- Postpartum hemorrhage rarely results in hypovolemic shock and necrosis of pituitary (if vascular system not supported, for example)
- Immediate result will be no prolactin production
1. First clue to dx is not able to breast feed - Very rare phenomenon now because we do so much to prevent and treat post-partum hemorrhage
What can you give to women who do not want to breast feed?
- NO medication to suppress breast milk production
- Good bra, breast binders, do not stimulate breast, and cycle of stimulation will break and production will cease
- Bromocriptine was used in the past, but not anymore because terrible side effects, including stroke
What are some of the complications of breastfeeding?
-
Mastitis: commonly caused by S aureus, Strep, or H. influenza -> introduced via baby’s mouth (baby giving it to mom)
1. Treat with antibiotics: Dicloxicillin
2. Continue breast feeding
3. Can be painful, so treat with some pain meds (Tylenol, in particular) - Occasionally an abscess results that requires surgical drainage (may cause pain)
1. Patient will feel ill, and have fever
2. Usually S. aureus via baby’s mouth
Describe fertilization.
- Occurs in the ampulla of the fallopian tube
-
Completes meiosis II, & zona pellucida becomes impenetrable so no other sperm can get in
1. Fails in polyploidy (69 chrom organism) - Pro-nuclei of sperm & oocyte fuse: 23 -> 46 chrom
- Cleavage of cells is rapid to form a morula, or mulberry-shaped embryo (12 or so cells via mitosis)
1. Blastocyst: morula cavitates -> inner cell mass (fetus) and outer layer (trophoblast and placenta)

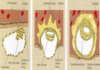
What are the steps from morula to implantation?
-
Day 4: morula enters the uterus, and cavitates, becoming blastocyst (day 5)
1. Trophoectoderm becomes the outer cell mass, and is destined to be the placenta
2. Inner cell mass destined to be the fetus - Day 8-9 post-fertilization: blastocyst actually implants

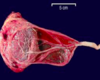
What is this?

-
Human blastocyst: can see the blastoceal cavity from the outside (area a little thinner, with mass-like appearance)
1. Inner cell mass: will become fetus
2. Outer cell mass: will become trophoblasts

What happens in implantation?

- Embryo travels to the uterine cavity day 5-6, and implantation occurs day 8-9
- Endometrium glycogen, lipid-rich: decidualization process promoted by progesterone produced by corpus luteum to nourish new embryo
1. Oftentimes, removal of an ovary will result in miscarriage b/c not enough progesterone -
Trophoblastic cells invade decidua: act much like cancer cells, attaching embryo to the endometrium
1. Invades so entire embryo can be nourished; uterine surface folds back over developing embryo - hCG produced by trophoblastic cells can be detected via blood testing
How are pregnancies dated?
- Based on first day of last menstrual period (LMP) b/c easier to establish than date of conception
1. Assumes idealized 28-day menstrual cycle - Due date always an estimate (EDD): normal 40 wks +/- 2 wks (or 40 wks gestational age)
1. Count back 3 mos from LMP and add 7 days: ex., LMP is May 10 -> EDD is February 17
2. +/- 2 weeks is considered term, or normal - This is important for potential EXPOSURES
Ms. L concerned about excessive alcohol use over NYE. First day of her LMP was Dec. 6th. When is her due date? What is your advice?
- Due date is September 13th
- She should be reassured -> embryo was likely just at an implantation stage where a teratogen would have no effect on organ development
- You can’t give her any guarantees, but you can certainly give her some advice
- NOTE: Accutane is the exception to problems with teratogen exposure in very early fetal development because may hang around a bit longer because it is a fat-soluble vitamin (A)
Trimesters (definitions)
- First: 0-14 weeks
- Second: 14-28
- Third: 28-40
1. 40 weeks is due date, but normal +/- 2 wks on either side
Fetus (definitions)
Unborn, regardless of gestational age
What is organogenesis?
- When organs forming: 2-8 wks after fertilization (4-10 weeks from LMP)
- Important for thinking about potential exposures and birth defects, i.e., from meds or environmental exposures
- Depends on precise ultrasound dating
Abortion (definitions?
- Medical term: by law, <20 wks or < 500 grams (pre-viable pregnancy loss that can be first or second term)
- Spontaneous: miscarriage
- Induced: medical/surgical procedure
Viability (definitions)
- Viability: > 23 weeks gestation
- Variable based on place of delivery
- Few miracle babies born at 21-22 weeks, but 23 weeks and above considered for possibility of viability
- No C-section if patient is <23 weeks b/c viability chance is practically 0
Pre-term, late-term, post-term (definitions)
- Preterm: <37 weeks gestation
- Late term: >41 weeks
-
Post-term: >42 weeks
1. Start to worry about adverse consequences after this date
What does G3P1011 mean?
- Pregnant now, one term birth, no preterm births, one abortion (not sure if spontaneous or induced), one living child
- Gravid: pregnant
- Parity: had a baby (dead or alive at birth)
What does G2P1002 mean?
- Pregnant now, one term birth, no pre-term births or abortions, two children living at home (twins)
- Gravid: pregnant
- Parity: had a baby (dead or alive at birth)
Why do we have prenatal care?
- To help achieve as good a maternal and infant outcome as possible
- Promote good health for mom and baby through the pregnancy
- Screening for and managing any complications that may develop during pregnancy or immediately post-op
- Identify needs for care beyond normal OB care: pts may have a number of other medical issues
What are the symptoms of pregnancy?
- Missed menses: the way many young women find out they are pregnant
- Nausea/vomiting: not sure why this happens; AM sickness generally happens early in pregnancy, but can continue throughout (meds to tx this)
- Breast tenderness: part of early symptomatology
-
Perceives fetal movement: primigravida 18 weeks; G2 or greater 16 weeks (i.e., if you have had more than one child, and you know what to look for)
1. NOT possible to feel this @ 8 wks b/c there are specific times when fetal movement is actually perceptible
How do pregnancy tests work?
- URINE detects: >25 mIU/mL -> 5-6 wks gestation (just missed a period); RELIABLE
- SERUM detects: >5 mIU/ml -> 3 wks LMP -> prior to pt knowing she’s pregnant (b4 missed menses)
1. Level doubles e/48 hrs in early pregnancy, and peaks at 10-12 weeks
2. Used to monitor in vitro fertilization - This hCG pattern critical for OB b/c they might be trying to determine if the pregnancy is a healthy one (reassuring that pregnancy is a healthy one, even if mom is having lots of cramping, bleeding)
How can the physical exam be used to diagnose pregnancy?
- Uterus soft (a little enlarged) at 6-7 wks gestation
- Cervix is bluish (blood engorgement)
- Can tell is enlarged at 7-8 weeks, and sometimes earlier, depending on the habitus
- Hear fetal heart tones w/battery operated Doppler at 10 weeks from LMP (depending on pt habitus)
- Used to rely on physical exam to diagnose early pregnancy before HCG levels and US to help
What are the PE landmarks for fundal height?
- Pelvic brim: 12 weeks -> should be able to feel the uterus abdominally
1. Umbilicus: 20 weeks
2. Beyond 20 wks: +1cm from pubic bone to fundus each week of gestation - In general, in spite of patient’s habitus, uterus for the most part grows in a predictable fashion
- Msmt in cm should be approx to wk of gestation -> important to be able to document normal growth

When should you be able to feel the uterus abdominally?
12 weeks