PHD - Hypersensitivity (Self) Flashcards
Which mast cell mediators promote cellular infiltration?
Leukotriene B4, chemokines, TNF, and eosinophil and neutrophil chemotactic agents
Viral hepatitis is associated with what type of hypersensitivity reaction?
Type IV (T-cell-mediated/Delayed) Hypersensitivity
Rheumatoid arthritis is associated with what type of hypersensitivity reaction?
Type IV (T-cell-mediated) Hypersensitivity T-cells against collagen or citrullinated self-peptides are present that lead to chronic inflammation and damage to joints
Which mediators of mast cells promote vasodilation?
Histamine Leukotrienes C4, D4, and E4 Prostaglandin D2 Platelet Activating Factor (PAF)
Rheumatic fever is a condition that is a result of what type of hypersensitivity reaction?
Type 2 (Antibody-mediated) Hypersensitivity Patients who have been infected with Streptococcus pneumoniae will develop antibodies to the Strep cell wall antigens. These antigens have similar epitopes to cardiac myocytes, which causes the antibodies to attack cells of the heart. This concept is known as molecular mimicry
What is the function of TNF and IFN-y in inflammation? From what type of cells are they produced? In what type of hypersensitive reaction is this noted?
Tumor necrosis factor (TNF) and Interferon gamma (IFN-y) are produced by CD4+ T-cells. These cytokines are responsible for activating macrophages, which will induce an inflammatory response. This is an example of type IV (T-cell mediated) hypersensitivity.
Outline the mechanism through which a type III hypersensitivity reaction occurs.
Type III hypersensitivity is mediated by immune complexes. 1. Free antibody binds free antigen in circulation, forming an immune complex. 2. Immune complex deposited in vessel wall 3. Neutrophils recruited to site via Fc receptor and complement (C5a) and activated 4. Inflammation damages vessels and tissues
What are the key factors of the early and late phases of Type I Hypersensitivity?
Early phase:
- Th2 response induces production of IgE to antigen
- Allergen binds IgE on mast cells and cross-links
- Release of histamine, protease, and chemotactic factors –> leaky vessels and vasodilation
Late Phase
- Mediated by eosinophils
- Release of leukotriene B4, C4, D4 and E4 –> recruitment of neutrophils and damage to vessels
The histological sample below is due to what condition? What type of hypersensitivity reaction is it associated with?
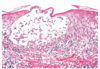
Contact dermatitis caused by a type IV (T-cell mediated) hypersensitivity
Image annotation: Separation of epidermis from dermis. Filled with edematous fluid (spongiosus). Notice ring of inflammatory T-cells surrounding the fluid pocket.
What signal causes a mast cell to degranulate?
Allergen binding to IgE and cross-linking on a mast cell membrane
Systemic lupus erythematousus (SLE) is associated with what type of hypersensitivity reaction?
Type III (Immune complex-mediated) Hypersensitivity
Remember that one of the hallmarks of SLE is having anti-nuclear, anti-smith, and anti-DNA antibodies that complex and get deposited in tissues.
Mast cell degranulation leads to the production of which eicosinoids?
- Leukotrienes
- B4 - recruits lymphocytes
- C4, D4, and E4 (aka slow-reacting substances of anaphylaxis, SRS-A) - induce late phase bronchoconstriction and endothelial cell damage
- Prostaglandin D2
Explain the mechanism of how pernicious anemia is a condition induced by a type II hypersensitivity reaction.
Type II (antibody-mediated) Hypersensitivity is characterized by the presence of antibodies to certain antigens.
In this case, the patient contains an antibody that binds to intrinsic factor, and causes it to malfunction or to be eliminated. Lack of intrinsic factor inhibits absorption of vitamin B12 in the terminal ileum, which leads to macrocytic anemia.
What type of hypersensitivity reaction is associated with Th2 response inducing IgE and mast cell release?
Early phase of type I (immediate) hypersensitivity
What is the mechanism of action of the Type IV hypersensitivity reaction?
Type IV hypersensitivity is mediated by T-cells
Antigens must be presented to T-cells via APCs in order to activate an immune response. Presentation activates both CD4+ and CD8+ T cells. CD8+ T-cells directly kill target cells. CD4+ cells produce interferon gamma and TNF, which activate macrophages and produce inflammation.
Myasthenia gravis is a result of what type of hypersensitivity reaction?
Type II (antibody-mediated) Hypersensitivity
Myasthenia gravis (MG) is a disease that causes hypotonia of muscles due to inhibition of the nicotinic acetylcholine receptor (nACHR) in the motor end plate. This process occurs when antibodies bind to the nACHR and prevent acetylcholine from binding.
Explain the mechanism of how myesthenia gravis is a type II hypersensitive reaction.
Myasthenia gravis (MG) is a disease that causes hypotonia of muscles due to inhibition of the nicotinic acetylcholine receptor (nACHR) in the motor end plate. This process occurs when antibodies bind to the nACHR and prevent acetylcholine from binding.
What are the contents of a mast cell granule?
-
Histamine
- Causes contraction of endothelial cells –> leaky vessels
- Contracted endothelial cells produce nitric oxide (NO) –> vasodilation and hypotension
- Causes broncoconstriction in 2 ways:
- Binds directly and causes smooth muscle contraction
- Induces vagus nerve to release ACh to cause smooth muscle contraction
-
Proteases
- Convert cell membrane lipids into leukotrienes and prostaglandins
-
Chemotactic factors
- Recruits lymphocytes
What is the skin condition causing blisters to form that is associated with a type II hypersensitive reaction? What immunoglobin drives this disease?
Bullous pemphigoid and pemphigus vulgaris
Remember that type II hypersensitivity reactions are mediated by antibodies. These conditions are caused by IgG that attacks cell-cell junctions, leading to blistering of skin.
Explain how immune thrombocytopenia (ITP) is a type II hypersensitive reaction.
Immune thrombocytopenia occurs when antibodies bind antigens directly on platelets, leading to destruction.
What is the mechanism that is associated with an early Type I hypersenitivity reaction?
Th2 response that leads to increased production of IgE and mast cell degranulation
Hashimoto’s thyroiditis is associated with what type of hypersensitivity reaction?
Type IV (T-cell mediated) hypersensitivity
Hashimoto’s Thyroiditis occurs when T-cells lead to the destruction of thyroglobulin and other proteins AND to the killing of thyroid epithelial cells. This causes hypothyroidism.
Which mast cell mediators promote smooth muscle spasms?
- Slow-reacting substance of anaphylaxis (SRS-A):
- Leukotrienes C4, D4, and E4
- Histamine
- Prostaglandins
- Platelet activating factor (PAF)
What are the “slow reacting substances of anaphylaxis” SRS-A?
Another term for leukotrienes C4, D4, and E4. They are called slow-acting because they must be produced by enzymatic conversion after proteases cleave membrane lipids. These proteases are released with mast cell granules.
Histamine is the “fast-acting” bronchoconstrictor
MS is associated with what type of hypersensitivity reaction?
Type IV (T-cell mediated) Hypersensitivity
MS is characterized as T-cell mediated destruction of cells that contain myelin. This leads to demyelination of CNS neurons, which can lead to paralysis.
Explain how Grave’s disease is mediated through a type II hypersensitivity reaction.
Grave’s Disease is characterized by the presence of autoantibodies to TSH receptors on thyroid cells. These autoantibodies activate thyroid cells to increase production of T3/T4, which leads to hyperthyroidism.
What are urticaria?
Hives

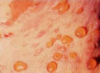
The histological sample below is indicative of what type of hypersensitivity reaction?

Type IV (T-cell mediated) Hypersensitivity
Notice the presence of T-cells within the dermis.

What granular cell is the tissue marker of a hypersensitivity-type reaction?
Eosinophil
The skin rash in poison ivy is due to:
A. Cross reacting antibodies against intercellular junctions
B. IgE antibodies against urushiol
C. Immune complexes deposited along the dermal-epidermal junction
D. T-cell derived cytokine-mediated inflammation
D. T-cell derived cytokine-mediated inflammation
Remember that poison ivy is a form of contact sensitivity caused by exposure of skin to urushiol. This causes a T-cell mediated response in the dermis of the skin.
Choice A describes pemphigus vulgaris/bullous pemphigoid (type II)
Choice B describes a type I (immediate)
Choice C describes a type III
Explain the pathway in which IgE is produced during a Type I anaphylactic hypersensitivty reaction.
- Antigen is presented to T-cells via APC
- T-cell binds B-cell and secretes IL-4, 5, and 13 to induce a Th2 response
- Th2 response causes isotype switching and production of IgE
- Fc portion of IgE binds FcER1 receptors on mast cells
A six-year-old boy develops hematuria, hypertension, and renal failure two weeks after a strep throat. The renal damage is caused by:
A. Anti-glomerular basement membrane antibodies
B. Immune complexes deposited in kidney
C. Streptococcal pyelonephritis
D. Thrombosis of renal artery
B. Immune complexes deposited in kidney
Streptococcal infections lead to antibodies produced against the cell wall antigens of the bacteria. These antigens share epitopes with cardiac myocytes and glomerular cells. Antibodies bind antigen and complex in the glomerulus, leading to kidney damage and streptococcal glomerulonephritis.
Choice A describes Goodpasture’s Syndrome (type II)
Choice C is the name of the condition this boy has, not how it was caused
Choice D would lead to coagulative necrosis
What condition is diagnosed using HEP-2 tissue cell cultures?
Systemic Lupus Erythematosus
Remember that HEP-2 cells are mixed with patients antibodies. Anti-IgG conjugated with fluorescent markers is added (indirect immunofluorescence) to determine presence or absence of autoantibodies typical in SLE. HEP-2 cells are derived from HeLa cells (from Henrietta Lacks)
What is the most severe symptom of immediate hypersensitivity? Why?
Anaphylaxis. Systemic mast cell degranulation causes massive vasodilation and bronchoconstriction, leading to hypotensive shock and hypoxia, respectively.
What are the outcomes of a type IV hypersensitivity reaction? By what cell is each outcome mediated?
- Inflammation - mediated by CD4+ T-cells (Th1 or Th17)
- Cytolysis - mediated by CD8+ T-cells
What two classes of drugs are used to treat bronchial asthma?
- Corticosteroids
- Downregulation of inflammatory cytokines and leukocyte migration factors (ICAM-1 and ELAM-1) - prevents immune cells from being recuited to area where allergen is
- Downregulation of phospholipase A2 production - decreases production of protaglandins and leukotrienes
- Upregulation of lipocortin-1 - inactivates pre-formed phospholipase A2
- Phosphodiesterse (PDE) inhibitors
- Inhibit degradation of cGMP –> smooth muscle relaxation (bronchodilation)
Goodpasture’s syndrome is a condition that is what type of hypersensitivity reaction? What does this condition target as an antigen, in which two organs of the body?
Type II Hypersensitivity
This syndrome is characterized by an antibody that targets type IV collagen in the basement membrane of the glomerulus and lungs.
This activates the complement pathway to cause damage
Which type of hypersensitivity reaction is associated with IgG bound to tissue, inducing activation of the complement system or leukocytes?
Type II (antibody-mediated) hypersensitivity
Which type of of hypersensitivity is associated with activation of T-cells and cytokines?
Type IV (T-cell mediated/Delayed) Hypersensitivity
What are the four types of hypersensitivity reactions?
- Type I - Immediate
- Type II - Antibody-mediated
- Think of the two antigen binding regions on an antibody (2 = antibody)
- Type III - Immune complex-mediated
- Think of how the roman numeral III looks similar to an “M” –> “M”mune complex
- Type IV - T-cell mediated/Delayed
- This is fourTh in the list, so remember that type IV is a Th-cell mediated response
A four-year-old develops anaphylaxis after consuming a peanut butter cookie. The underlying process involves:
A. Cross-linking IgE antibodies on the surface of mast cells
B. Deposition of immune complexes in vessels and activation of complement
C. Direct activation of complement
D. IgG anti-peanut antibodies which cross-react with endothelial cells
A. Cross-linking IgE antibodies on the surface of mast cells
Remember that anaphylaxis is associated with a type I (immediated) hypersensitivity reaction. Type I reactions are mediated by cross-linking of antigen with IgE on mast cells, causing degranulation and massive histamine release.
B describes type III
C describes type II
D describes molecular mimicry
Pernicous anemia is a condition associated with what type of hypsersensitivity reaction?
Type II (antibody-mediated) Hypersensitivity
Pernicious anemia is caused by a lack of B12 absorption secondary to lack of intrinsic factor. Intrinsic factor normally binds B12 and is absorbed in the terminal ileum. However, patients with this condition have antibodies against intrinsic factor.
Hay fever is a condition that is a result of what type of hypersensitivity reaction?
Type I (Immediate) Hypersensitivity
Hay fever causes allergic rhinitis and edema, and can lead to anaphylaxis. Allergies are mediated by IgE and mast cells (a type I characteristic)
Type I diabetes mellitus is associated with what type of hypersensitivity reaction?
Type IV (T-cell mediated/Delayed) Hypersensitivity
Type I DM is characterized by the destruction of pancreatic beta cells, which leads to insulin-deficiency. CD8+ T-cells kill these cells and prevent insulin from being produced, leading to diabetes.
A patient with an immediate hypersensitivity reaction will have what clinical manifestations?
- Angioedema
- Urticaria (hives)
- Pruritis (itching)
- Smooth muscle constriction
- Bronchoconstriction –> wheezing and hypoxia
- In GI tract –> vomiting and diarrhea
- In bladder –> involuntary urination
- Shock (in severe cases) - due to hypotension
What condition is likely to be observed in a patient recovering from strep? What type of hypersensitivity reaction is this?
Streptococcus glomerulonephritis
Antigen-antibody complexes (type III) are deposited in the glomerulus –> inflammation and renal damage
Inflammatory bowel disease (Crohn’s disease) is associated with what type of hypersensitivity reaction?
Type IV (T-cell mediated/Delayed) Hypersensitivity
Recognition of surface antigens on platelets in the body is a hallmark trait of what condition? What type of hypersensitivity reaction is this?
Immune Thrombocytopenic Purpura (ITP)
This is a type II reaction because it is caused by antibodies binding to surface antigens on platelets.


