Peds Flashcards
CHILD ABUSE
- What children are at greatest risk of child abuse?
- What are the orthopedic manifestations of child abuse?
- First-born children, unplanned children, premature infants, stepchildren, and handicapped children
- Single-parent homes, drug abusing parents, parents who were themselves abused, unemployed parents, and families of lower socioeconomic status
- Long bone fractures in nonambulatory child
- Multiple fractures in various stages of healing
* Occurs in 70% of abused children less than 1 year of age and more than 50% of all abused children - Rib fractures (posterior and posterolateral)
- Transphyseal fracture of the distal humerus
- Metaphyseal ‘corner fracture’ or ‘bucket handle fracture’
- Vertebral compression fractures
- Spinous process avulsions
TRANSPHYSEAL DISTAL HUMERUS
- What is the management of transphyseal distal humerus fractures?
- What is the most common complication of a transphyseal distal humerus fracture?
CRPP with arthrogram
- Arthrogram is performed and direction of displacement is confirmed
- Closed reduction is performed similar to supracondylar fractures
- 2-3 lateral pins – divergent, engaging opposite cortex and wide spread
- Pins removed at 3 weeks
- Cubitus varus
What are blocks to closed reduction of proximal humerus fractures?
[JAAOS 2015;23:77-86]
- LHB tendon
- Capsule
- Periosteum
What is the closed reduction maneuver for proximal humerus fractures?
[Orthobullets]
- Longitudinal traction
- Abduction to 90°
- ER
What are the surgical options for proximal humerus fractures?
[JAAOS 2015;23:77-86]
CRPP – 2-3 lateral pins
What is the most common associated fracture with a supracondylar humerus fracture?
[JAAOS 2012;20:69-77]
Ipsilateral distal radius
What is the most common nerve injury associated with an extension type supracondylar fracture?
[JAAOS 2012;20:69-77] [JAAOS 2015;23:e72-e80]
- Extension type
- Anterior interosseous nerve
- Followed by median, radial and ulnar
- Flexion type
* Ulnar nerve - Posterolateral displacement
* Median and anterior interosseous nerve - Posteromedial displacement
* Radial nerve
In the absence of a distal radial pulse, what are clinical indicators of sufficient perfusion?
[JAAOS 2012;20:69-77]
- Normal capillary refill
- Temperature
- Color (typically described as pink)
What is Baumann’s angle?
[Orthobullets]
- Angle formed between a line parallel to the longitudinal axis of the humeral shaft and a line along the lateral condylar physis as viewed on the AP image
- Normal = 70-75 (compare to contralateral side)
- Deviation >5-10 should not be accepted
What are blocks to closed reduction of supracondylar fractures?
[JAAOS 2015;23:e72-e80]
- Brachialis muscle interposition
- Button-holing of metaphyseal spike through brachialis
- Brachial artery
- Nerve
- Periosteum
- Joint capsule
What is the technique for closed reduction of an extension type supracondylar fracture?
[CORR course]
- Elbow extension, longitudinal traction, correct varus/valgus and medial/lateral translation and rotation, flex elbow with thumb pressure over olecranon to correct sagittal alignment
- Consider milking brachialis if distal humerus buttonholed through
What is the technique for closed reduction of a flexion type supracondylar humerus fracture?
- “push-pull technique” [Journal of Pediatric Orthopaedics B 2016, 25:412–416]
* With elbow at 45 correct coronal plane deformity (varus/valgus/translation), flex elbow to 90 with towel under apex of deformity apply a posterior directed force along the axis of the forearm, slight over correction can be corrected with a pull along the axis of the forearm - Traditionally done in extension
What are the complications associated with operative treatment of supracondylar fracture?
[JAAOS 2012;20:69-77]
- Pin migration
- Pin tract infection
- Osteomyelitis/septic arthritis
- Malunion
- Compartment syndrome
- Ulnar nerve injury
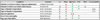
What is the recommended pin placement in management of supracondylar fractures?
[JAAOS 2012;20:69-77]
- Adequate number of lateral pins
* In general, Type II – 2 pins, Type III – 3 pins - As far apart as possible
- Pins should be divergent
- Pins should not converge or cross at fracture site
- Pins should engage both the medial and lateral columns
- Consider a medial pin if fracture remains unstable or in presence of comminution
What is the technique for medial pin placement in SCHF?
[JAAOS 2012;20:69-77]
- Small incision over medial epicondyle
- Elbow in extension (prevents ulnar nerve from subluxing anterior)
- Identify and protect ulnar nerve
What are the indications for a medial pin in SCHF?
[CORR course]
- Reverse obliquity
- Very distal fractures
- Very young
What is the management of the pulseless hand in the setting of a supracondylar humerus fractures?
[JAAOS 2012;20:69-77]
- In the presence of adequate perfusion (pink)
- Reduce fracture and pin
- If adequate perfusion remains – admit for observation with elbow in approx. 45° flexion
- In the presence of pulseless extremity and inadequate perfusion (white)
- Reduce the fracture and pin
- If remains dysvascular – explore artery and monitor for compartment syndrome (consider fasciotomy)
- If adequate perfusion - admit for observation with elbow in approx. 45° flexion
What neurological injury is associated with injury to the brachial artery in SCHF?
[JBJS 2015;97:937-43]
Median nerve
In a SCHF, if an open exploration is performed and there is still inadequate distal perfusion despite the brachial artery being in continuity and decompressed, what can be attempted relieve vasospasm?
[JBJS 2015;97:937-43]
- Increase ambient temperature
- Apply topical lidocaine or papaverine
- Stellate ganglion block
What approaches are used for management of open reduction of supracondylar fractures?
[JAAOS 2015;23:e72-e80]
“go to the metaphyseal spike”- [CORR course]
- Anterior approach = extension type
- Transverse or ‘lazy S’ over flexion crease of antecubital fossa
- If releasing blocks to reduction – stay lateral to biceps tendon to avoid neurovascular structures
- If exploring neurovascular bundle – identify proximal to fracture site
- Lateral approach = posteromedial displacement
* Plane between BR and triceps - Medial approach = posterolateral displacement and flexion type
What are the complications associated with supracondylar humerus fractures?
[JAAOS 2012;20:69-77]
- Cubitus varus
- Can lead to cosmetic concerns and tardy posterolateral rotatory instability b
- No effect on elbow ROM
- Correctional osteotomy should be considered if significant varus present
- Performed at >1 year
- Lateral closing wedge osteotomy with pin fixation
- What is the Skaggs osteotomy? [J Child Orthop. 2011 Aug; 5(4): 305–312]
- Interlocking lateral wedge osteotomy with lateral pin fixation
- Corrects cubitus varus and extension
- Enhanced stability and less lateral prominence than closing wedge
- Compartment syndrome
What radiographic view best demonstrates a lateral condyle fracture?
[J Am Acad Orthop Surg 2011;19:350-358]
Internal oblique view (fragment often lies posterolateral)
How is an arthrogram administered in the context of distal humerus lateral condyle fracture?
[J Am Acad Orthop Surg 2011;19:350-358]
Traditionally performed via the lateral soft spot, which is a triangle formed by the radial head, olecranon, and lateral column of the humerus.
- This area may be distorted in patients with lateral condylar fracture
- Alternatively, the needle may be placed directly into the posterior surface of the olecranon fossa.
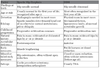
What are the indications for nonop vs. operative management in lateral condyle humerus fractures?
[J Am Acad Orthop Surg 2011;19:350-358]
- Nonoperative indications
- Type I, nondisplaced
- Fractures with an intact cartilage hinge that has been confirmed on MRI
- ≤2 mm displacement on all radiographic views
- Operative indications
- >2mm displacement
- 2-4mm = CRPP
- >4mm = ORIF
- Nonunion