Parturition & Lactation Flashcards
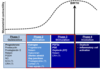
Phase 1 Quiescence
prelude to birth
2nd trimester & 1st part of 3rd trimester
Uterine quiescence
No contractility
Phase 2 activation
R for OT & PGF/PGE up regulated
Ion channels activated
Connexin 43 increase
- gap junctions
- contractility
Phase 3 Stimulation
labor & birth
contractions
cervical dilation
delivery of fetus & placenta
Myometrium responds to uterotropic agents, oxytocin & PGs
Phase 4 Involution
Recovery
Facilitated by OT
delivery of placenta results in rapid hormone withdrawal
Uterine involution & cervical repair
Postpartum
- lactation
- depression
Uterine Activity Regulation
Oxytocin OT
Potent uterotonic agent
OT induced uterine contractions identical to endogenous ones
Uterine contractions can be induced w/ electrical stim of post pit or manual stim of nipple
OT R antagonist- competitive Inhibit labor
Atosiban inhibit preterm labor
Myotmetrial response to OT
Increase sensitivity to OT with increase gestation time
Changes to myometrial OT R
Up reg OT R prior to parturition
PG & parturition
COX inhibitors- inhibit myometrial contractility
Exogenous delivery of PGF2a & PGE2 stimulates uterine contractility in women
PG increase during labor!
COX2 upreg in myometrium & cervix just prior to parturition
FP & OTR
FP
- GPCR
- smooth m. contraction
- vasoconstriction
- vasuclar smooth m. hypertrophy
- stim Ca2+ mobilization
OTR
- smooth m. contraction
- inhibited by progesterone
- mRNA up reg by estradiol
- stim Ca2+ mobilization
EP R
EP1 & EP3
- smooth m. contraction
- vasoconstriction
- EP1 Ca2+ mobilization
- EP3 decrease cAMP
- in upper fundus
EP2 &EP4
- smooth m. relax
- vasodilation
- stim adenylate cyclase
- stim cAMP production
- on the cervicx
Pre term uterus- quiescence

PGE2 & progesterone
- relax tone
- inhibit contractions
- PR
- high EP2 R esp in JZ
- low EP1/EP3
Mem bound PR
- PGRMCs
- high in JZ
Term uterus

Fundus & upper segments
- decrease/loss PR
- decrease/loss mPR
- up reg OTR
Lower seg
- slight increase in OTR
Cervix
- no OTR
Term uterus

Outer myometrium
- up reg FP
fundus
- up reg EP3
- up reg FP
upper seg
- up reg EP3
- up reg FP
Lower seg & cervix
- up reg EP4 & high level EP2
- lower FP level
Amnion & Fetus contribute to contractility

EP1, EP3 & FP are up reg in amnion during labor
Contractile F & R gradient

smooth m. contractile OTR, FP & EP3 R are highest in fundus & upper seg of uterus
Strong contractions
Smooth m. relaxant EP2/EP4 are higest in lower seg & cervix.
Relaxation
Strong contractions initiated in fundus & radiate to cervix.
Parturition requires uterine relaxation

myometrium must relax between contractions
tonic prolonged contraction can cause uterine tetany= life threatening to fetus
As labor progress
- increase OT & PGF
- increase contraction intensity
- decrease relaxation
Net= increased contractile F & decreased time between contractions
Summary
PGF2 augments OT action
PGF binds to FP to cause intense smooth m. contractions throughout entire uterine body
PGF2 stim paracrine OT production
PGE contributes to smooth m. contraction, by binding to EP3 R in uterine fundus & EP1/EP3 R on amnion
PGE2 binds to EP2 R throughout uterus to reg smooth m. relaxation
PGE2 binds to EP2 & EP4 to stim relaxation of lower seg of uterus & cause relax & dilation of cervix!
Increase estrogen may induce parturition
localized E:P ratio shift @ end of gestation in favor of estrogen
stim formation of myometrial gap junctions
stim PGF2a & PGE2 production
stim OT production
stim upreg of myometrial OT R
stim cervical ripening
Intrauterine hormone
OT & PRL stim enz activity in decidual cells
increase hydrolysis of estrone sulfate in fetal mem
Together lead to increase production of locally acting intrauterine estrogens
local effects
- changes due to increase local [] of estrogen
Localized progesterone withdrawal
Progesterone decreases myometrial tone, increased cervical rigidity & blocks OT R
Decrease in progesterone favors myometrial activation
Progesterone withdra permits for myometrial contractions & cervical ripening
Increase PGF2a & PGE2 production
Stim upreg of MMPs - breakdown of cervical plug
MMPs
Ovary, release OCCC & fibrinolysis of follicle wall
Endometrium, breakdwn functionalis & vascular remodeling
Endometerium, invasion & vascular remodel
cervix. dilation & ripening
Labor & Delivery
childbirth period of onset of regular uterine contractions until expulsion of placenta
Stage 1 labor
Latent phase
- reg uterine contractions that bring dilation of cervix (2-4 cm)
- Epidural
Active
- rapid change in dilation to 10 cm
Stage 2 of labor
starts when cervix is fully dilated to delivery of infant
increase in bloody show
desire to push
pressure on rectum
onset of nausea & vomiting



