Papers by KL Flashcards
(251 cards)
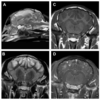
Images of the same dog, 6 months apart. What caused the difference in their appearance? What other significant finding was described in this paper?

Dog with PDH treated with trilostane.
This study also showed a statistically significant increased in size of the adrenals after treatment.
What is the significance of these three patterns of enhancement of the canine adrenal gland?

All three patterns are associated with PDH. Common features include disorderly enhancement throughout the adrenal.
Dogs with PDH also had higher peak intensity than normal dogs.
What is the structure labeled LAG?
How is this image obtainted?
What is the range of thickness of this organ?

Left adrenal gland, obtained transrectally in a horse
Normal: 0.5 - 1.4 cm thick (range)
Mean thickness of caudal pole: 0.66 cm
Mean thickness of cranial pole: 0.9 cm
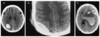
What is a cholesteatoma?
What are characteristic imaging features on CT?
Epidermoid cyst (keratin-filled)
CT: non-contrast enhancing, expansile, tympanic cavity mass, ~ 50-60 HU. Some dogs will have ring enhancement. Bony changes of the bulla (lysis, thickening, expansion), TMJ. Can cause lysis of the petrous temporal bone –> intra-cranial extension

What are the MRI features of a cholesteatoma?
T1w-iso to hypo
T2w- hyper
No CE
No T2* artifact
(Harran, JAAHA 2012)

What is the average range of attenuation for each of the following (in the context of peritoneal effusion)?
- Bile, urine, intestinal contents
- Clotted blood
- Unclotted blood
- Bile, urine, intestinal contents: 0-15 HU
- Clotted blood: 45-70 HU
- Unclotted blood: 30-45 HU
What is the sentinel clot?
The highest attenuating hematoma (sentinel clot) is expected to be close to the site of bleeding. Lower attenuating unclotted blood is located farther from the source.
What were the important factors in optimizing CT protocols for metallic gunshot head trauma in a seal? What factors did not result in improved image quality?
Minimized artifacts with: high frequency image reconstruction algorithm, proprietary extended CT scale raw data reconstruction (ECTS). All with WIDE window setting.
Increasing tube voltage and use of beam-hardening reduction (PFO) filter did not significantly reduce metal artifacts
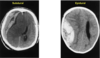
What are the MRI features of acute distemper virus?
- T2W hyperintense, T1W hypointense lesions in the cerebellum and brainstem with loss of gray–white matter distinction (areas of demyelination)
- Large, ill-defined lesions affecting the cerebral gray matter that are T2W and T2-FLAIR hyperin- tense and T1W iso- or hypointense; the may be attributed to the acute, post-ictal brain edema.
What are the MRI features of chronic distemper virus?
- Bilaterally symmetric hyperintense T2W lesions of the white matter just deep to the gray–white matter junction of the parietal and frontal lobes.
- T2W hyperintensity of the arbor vitae of the cerebellum causing loss of cerebellar gray–white matter junction.
- Ill-defined hyperintense T2W lesion of the caudal brainstem.
- Pachymeningeal contrast enhancement.

What are some features of NME that are not commonly reported with GME?
Meningeal enhancement, mass effect, and ventricular dilation were features frequently seen in these cases of NME that are not commonly associated with GME.

In evaluating meningioma and histiocytic sarcoma, how do the following parameters compare?
- Intratumoral ADC and fractional anisotropy (FA)?
- Peritumoral ADC and FA?
- High T2 signal ADC and FA?
- Intratumoral ADC and fractional anisotropy (FA)?
- ADC: HiSA (0.76) < meningioma (1.1)
- Similar FA
- For both peritumoral and high T2 signal ADC and FA?
- ADC: HiSA > meningioma
- FA: HiSA < meningioma
What is the proposed significance of FA and ADC measurements in the peritumoral region?
Lower FA and higher ADC are associated with infiltrative tumor cells
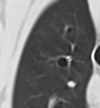
What are the three general causes of bronchial dilation/bronchiectasis?
- Damage to bronchial wall (e.g., chronic bronchitis, chronic pneumonia)
- Obstruction of the bronchial lumen
- Traction from fibrotic tissue (e.g., IPF)
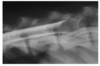
What is the significant feature present in this image that helps you identify the type of bronchiectasis present?

- No bronchial wall thickening to indicate chronic inflammation/damage
- Too diffusely affected to be secondary to obstruction of the lumen
- Diffuse ground glass opacity may indicate pulmonary fibrosis –> therefore this is traction bronchiectasis.
Fitzgerald, et al. VRU 2017

What are the differential diagnoses for contrast medium superimposed with the spinal cord during myelography (6)
- Epidural contrast deposition (focal CM accumulation at the nerve roots may mimic intramedullary contrast – check the VD, should be lateralized)
- Subarachnoid cyst
- Central canalogram (incidental vs. trauma to the cord vs. neoplasia)
- Syringohydromyelia
- Myelomalacia
- Severed spinal cord
Lu, D., Lamb, C.R. & Targett, M.P. (2002) Results of myelography in seven dogs with myelomalacia. Veterinary Radiology and Ultrasound 43, 326–330
Where is the contrast accumulating?
Subdural space
Subdural injection commonly causes contrast to accumulate in the dorsal subdural space of the cranial cervical area. This results in a radiopaque line of contrast with a very sharp dural border, a sharp bevel- or knife tip-like caudal end on lateral radiographs, and a wave-like ventral/axial border on lateral/ventrodorsal radiographs, respectively (also known as the dural drape sign).
Llabres-Diaz, F.J. (2005) Practical contrast radiography 4. Myelography. In Practice 27, 502–510

Where is the contrast accumulating?

Epidural space
The presence of marked undulations in the contrast over the disc spaces, contrast medium around the nerve roots outside the vertebral canal and also in the caudal lumbar area, away from the caudal end of the subarachnoid space, and/or the presence of patchy pooling of contrast in the dependent portions of the vertebral canal can help to identify this artefact.

Where is this lesion located? (Epidural, intradural extramedullary, or intramedullary)

Intramedullary (nephroblastoma)
Intramedullary lesions result in a widening of the spinal cord, together with narrowing and abaxial deviation of the subarachnoid contrast columns on all
projections
Which of the following statements is incorrect regarding normal findings in myelography:
- Focal thinning of the ventral subarachnoid space at the intervertebral disc spaces is common in larger breeds.
- Contrast accumulation in the dural sace can be used to confirm subarachnoid injection of contrast medium.
- There is normal, focal widening of the spinal cord at the level of C5-7 and L3-4.
- The subarachnoid space terminates at the level of C1 and does not cross into the foramen magnum.
Which of the following statements is incorrect regarding normal findings in myelography:
- Focal thinning of the ventral subarachnoid space at the intervertebral disc spaces is common in SMALLER breeds.
- Contrast accumulation in the dural sace can be used to confirm subarachnoid injection of contrast medium.
- There is normal, focal widening of the spinal cord at the level of C5-7 and L3-4.
- The subarachnoid space terminates at the level of C1 and does not cross into the foramen magnum.
Give some examples of diseases that can produce a normal myelogram (4-6 examples)
- Myelitis
- Meningitis
- Degenerative myelopathy
- Ischemic myelopathy
- +/- trauma
- +/- GME
Where is this lesion located?
Intradural extramedullary

What is a typical dose of contrast for equine myelography?
25-50 ml (following removal of 10-40 ml CSF)
What are considered normal results of flexion and extension on the contrast columns in equine myelography?
Flexion:
- dorsal contrast column is unchanged
- ventral contrast column will narrow at the IVDS
Extension:
- dorsal contrast column is unchanged
- ventral contrast column will become wider at C5