Pancreatitis Flashcards
What is pancreatitis?
What are the 2 distinct types of pancreatitis?
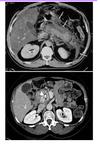
What are the white parts in the 2nd CT scan?

Inflammation of the pancreas
- Acute pancreatitis = rapid onset; the pancreas becomes ‘muddy’ as excess pancreatic juice leaks out
- Chronic pancreatitis = long-standing; recurring (tends to be due to alcohol consumption)
White parts in the 2nd CT scan shows calcium deposits (rok solid depositions) in the head of the pancreas
What are the common risk factors / causes for pancreatitis?
What is the mneumonic to remember it?
What are the 2 most common reasons?
G – gallstones = most common
E – ethanol (alcohol) = most common
T – trauma
S – steroids
M – mumps and other viruses (EBV, CMV)
A – auto-immune (Polyarteritis nodosa, SLE)
S – scorpion/snake bite
H – hypercalceamia, hypertriglyceridaemia, hypothermia
E – 1% risk factor with ERCP (so ERCP should only be conducted if absolutely neccessary)
D – drugs (SAND: steroids and sulphonamides, azothioprine, NSAIDS, diuretics [loop/thiazide])
Gallstones and ethanol cover 80% of the causes
What is the pathophysiology of acute pancreatitis?
Stone in the ampulla causes a back pressure
Bile can back flow into pancreas and cause irritation
What causes the development of acute pancreatitis over time? (pathogenesis)

Most common cause is alcohol, as it increases the permeability of the pancreatic duct epithelium. Digestive enzymes produced by the acinar cells of the pancreas diffuse into the periductal interstitial tissue. Also, pancreatic juice leaks from the pancreatic ducts and into the duodenum continuously. These pancreatic enzymes are activated intracellularly.
Additionally, alcohol causes the precipitation of proteins into the ducts causing a buildup of back pressure
What is the issue with pancreatitis in relation to trypsin activation? How does this affect the panceatitis progression?

Trypsin activates many other pathways, incuding:
Elastase = bleeding occurs because elastase begins eating away and disrupting blood vessels, resulting in ‘haemorrhagic pancreatitis’, hyperglycaemia due to the destruction of islets
Prothrombin = thrombin activation, causes thrombosis and ischaemia (and eventually pancreatic necrosis)
Phospholipase A2 released in the pancreatic juice = gets out into the body and causes fat necrosis, saponification - uses up a lot of calcium and when phospholipase A2 enters the bloodstream, it breaks down the albumin, resulting in hypocalcaemia and hypalbumenia
Kallikrein = many substances released that cause vasodilation
Shock = can result in hypoxia (oxygen deprivation) and anuria (failure of the kidneys to produce urine)

What are the 2 systemic damages caused by pancreatitis?
- Hypoxia
- Anuria
What does a Phospholipase A2 in the presence of free fatty acids (FFAs) from the fat necrosis do?
Interfere with surfactants of your lungs
Results in development of respiratory effects
What are the 3 types of acute pancreatitis?
- Oedematous - ‘changes consistently’ pancreatitis
- Haemorrhagic - arroding of blood vessels and bleeding
- Necrotic = if infected, many corresponding issues (black part on the CT scan shows bacteria producing gas in the infected pancreas)

What are the clinical features of acute pancreatitis, in terms of signs and symptoms?
Symptoms:
Epigastric pain, nausea and vomitting, fevers (due to an inflammatory response, or response to infection)
Signs:
Hypertensive / tackycardiac (in response to losing fluid), peritonism in upper abdomen/generalised (sore stomach), Grey-Turner’s sign (bruising in flanks, usually on one side of the abdomen), Cullen’s sign (bruising around umbilicus)
Bruising tends to occur in haemorrhagic pancreatitis
How is pancreatitis usually diagnosed? What do they look for clinically?
What do some other causes of increased amylase include?
Using a blood test, looking for:
Amylase/lipase
Other causes of ↑ amylase include:
Parotitis
Renal failure
Macroamylasaemia
Bowel perforation
Lung/ovary/pancreas/colonic malignancies can produce ectopic amylase)
Pancreatitis symptoms and signs, and sometimes increased amylase in blood tests, overlap with which other conditions as well?
- Gallstone disease
- Peptic ulcer disease / perforation
- Leaking / ruptured AAA (abdominal aortic aneurysms)
What are the 6 different investigations that can be performed to find / diagnose acute pancreatitis? And why?
- Blood test - look for amylase
- X rays - Erect chest X-ray to make sure there is no perforation, abdominal X-ray to look for gallstones
- USS - ultrasound scan to look for gallstones
- CT abdomen - quite unnecessary, unless after 48hrs suspect there may be more than just pancreatitis going on
- MRCP - type of MRI for suspected gallstone in the common bile duct (CBD)
- ERCP - last resort, only used to remove gallstone from CBD
How can the severity of a pancreatitis be measured? Using what criteria?
What is a mneumonic to help assess severity? How does this scoring system work?
How many points scored equates to severe pancreatitis?
What is a completely different, independent indicator of severity?
Modified Glasgow criteria:
P – PO2 <8KPa
A – age >55yrs
N – WCC >15
C – calcium <2mmol/L
R – renal: urea >16mmol/L
E – enzymes: AST >200iu/L, LDH >600iu/L
A – Albumin <32g/L
S – sugar >10mmol/L
Each sign equates to a point. 3 points or more within 48hrs of the onset of symptoms = severe pancreatitis
CRP - CRP levels >200 suggests severe pancreatitis
What is the management / treatment plan for acute pancreatitis?
What are the 4 main principles of management?
- ABC - airways, breathing, circulation
- Fluid resuscitation (IV fluids, urinary catheter, strict fluid balance monitoring)
- Analgesia
- Pancreatic rest - nutritional support if prolonged recovery, NJ feeding tube (through the nose and into the small bowel so the pancreas is not activated
- Determining underlying cause
What percentage of AP settle with conservative treatment?
95%
Very rarely is surgery needed, usually last resort
What are some systemic complications associated with acute pancreatitis?
Can affect any system as it activates cascade after cascade:
Hypocalcaemia
Hyperglycaemia
SIRS (Systemic Inflammatory Response Syndrome)
ARF (Acute Renal Failure)
ARDS (Adult Respiratory Distress Syndrome)
DIC (Disseminated Intravascular Coagulation)
MOF (Multi Organ Failure) & death
What are some local compliations of acute pancreatitis?
Pancreatic abscess
Pancreatic necrosis - unusual to do an operation to take outthe dead tissue, looks kind of like ‘porridge’ (must be scooped out). Now more commonly used = tube inserted and necrosis flushed out
Pancreatic pseudocyst
Haemorrhage - due to bleeding from arroded vessels:
Small vessels = haemorrhagic pancreatitis (Cullen’s/Grey Turner’s sign), Large vessels (e.g. Splenic artery) = life threatening bleed (unless forms pseudoaneurysm)
Thrombosis - of splenic vein, superior mesenteric vein, portal vein (in order of frequency):
- ascites (abnormal build up of fluid in the abdomen)
- small bowel venous congestion/ischaemia
Chronic pancreatitis
How can an infected necrosis pancreatitis be treated?
Antibiotics and Surgery
What is a pancreatic abscess?
How can the pancreatic abscess be treated?
Complication of infected necrosis - a collection of pus from pancreatic tissue necrosis & infection, becomes lined by granulation tissue, presents 2-4 weeks after attack of pancreatitis
Treatment = antibiotics and surgical drainage
What are pancreatic pseudocysts?
Why is it not a real cysts?
How can pancreatic pseudocysts be treated / managed?
A dmall pancreatic leak - slow pancreatic fluid collection, around which a fibrous capsule forms, presents >6 weeks after pancreatitis
Does not have an epithelial lining
95% spontaneously resolve over 6 months, unless they cause symptoms, in which ase there are 3 ways to drain them:
- Percutaneously under radiological guidance (CT)
- Endoscopically - EUS puncturing posterior wall of stomach & inserting stent
- Surgically via laparoscopic/open
When would you intervene for a pancreatic cyst?
Pseudocyst symptomatic (pain) Pseudocyst causing compression of surrounding structures e.g. CBD (obstructive jaundice), duodenum (high SBO) Pseudocyst infected (abscess) These 3x situations pseudocyst → drained
Explain the surgical intervention below for a pancreatic pseudocyst:
Pseudocyst is ruptures and it’s capsule attached to the lining of the stomach, so the cyst’s contents drain into the stomach
(I think)
What are the biggest issues associated with chronic pancreatitis?
Endocrine issues = insulin dependent diabetes
Exocrine issues = steatorrhoea (excretion of abnormal quantities of fat in the faeces)
What are the 3 main questions asked to someone with pancreatitis?
- What painkillers are you taking?
- What are they taking for their diabetes (if any)
- How much creole are you taking?


