Myeloma Flashcards
What is the pathophysiology of myeloma?
Myeloma is a plasma cell dyscrasia. Malignant proliferation of a single clone of plasma cells accumulating in the bone marrow, leading to overproduction of Ig or Ig fragments causing organ dysfunction.
How is myeloma classified?
Based in Ig product - it is usually IgG (2/3) or IgA.
Why does myeloma increase susceptibility to infection?
Immunoparesis: levels of Igs other than the one undergoing malignant proliferation (eg IgG) are low; also neutropaenia from cell crowding and treatment.
What are Bence Jones proteins?
In 2/3 of patients with myeloma, urine contains Bence Jones proteins, which are free Ig light chains of kappa (K) or lambda (λ) type, filtered by the kidney.
Describe the epidemiology of myeloma.
Peak age 70 years More common in afro-caribbeans
Give 4 signs of end-organ damage in myeloma.
CRAB HyperCalcaemia Renal impairment - decreased urine output Anaemia, neutropaenia or thrombocytopaenia (marrow infiltration, same as leukaemia) Bone lesions
Why can myeloma cause backache and pepperpot skull?
Myeloma cells signal increased osteoclast activity which causes osteolytic bone lesions which cause backache, pathological fractures and vertebral collapse. This causes pepperpot skull - small holes in the skull.
Why can myeloma cause hypercalcaemia and what are 4 signs of hypercalcaemia?
Myeloma cells signal increased osteoclast activity, causing hypercalcaemia which causes ‘bones (fractures), stones (kidney stones), groans (abdominal pain) and psychic moans (depression)’.
Other than hypercalcaemia what can cause renal impairment in myeloma?
Light chain deposition (20% of myelomas). Damage is mainly caused by precipitation of light chains in the distal loop of Henle. Monoclonal Igs also disrupt glomeruli.
What type of anaemia occurs in myeloma?
Normocytic normochromic anaemia.
What would bloods show for myeloma?
FBC: Marrow infiltration: anaemia, neutropaenia, thrombocytopaenia. ESR: raised Urea and creatinine: raised Hypercalcaemia (40%)
What would bone marrow biopsy show for myeloma?
Many plasma cells with abnormal forms
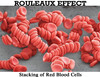
What would blood film show for myeloma?
Rouleaux formation of red cells. This means stacks or aggregations of RBCs because of the discoid shape.
What would be seen on X ray for myeloma?
‘Punched out’ lesions eg pepperpot skull, vertebral collapse, fractures.
What is electrophoresis?
Separation of macromolecules by their charge. Lots of differently charged molecules give a diffuse smear while lots of similarly charged molecules give a band. Therefore it is used to diagnose myeloma, where there is a monoclonal Ig which shows as a band.
What is the first-line screen for bone lesions in myeloma?
Skeletal survey using x ray. (PTS)
What is CT/MRI used for in myeloma?
Looking for lesions which cannot be seen on x ray.
What are the diagnostic criteria for myeloma?
- Monoclonal protein band in serum or urine electrophoresis 2. Many plasma cells on marrow biopsy 3. End-organ damage: CRA 4.Bone lesions
How is hypercalcaemia treated in myeloma?
- Rehydration with IV saline 2. IV bisphosphonates eg zolendronate for acute hypercalcaemia treatment
Spinal cord compression occurs in 5% of myeloma cases. How is this diagnosed and treated?
Diagnosis using MRI -urgent Treatment with dexamethasone corticosteroid and local radiotherapy.
How might myeloma cause visual disturbance? How is this treated?
Hyperviscosity due to increased plasma cells causes reduced cognition, disturbed vision, and bleeding. It is treated with plasmapheresis to remove light chains.
How is acute renal injury treated in myeloma?
Rehydration. Urgent dialysis may be needed.
Describe the supportive management of myeloma.
- Analgesia and bisphosphonates for bone pain
- Blood transfusion +/- EPO for anaemia
- Rehydration for renal failure and keep hydrated to prevent light-chain deposition
- Antibiotics for infections.
Why would you not use NSAIDs for bone pain in myeloma?
There is a risk of renal impairment.
Describe the curative management of myeloma.
- Chemotherapy 2. Autologous stem cell transplantation if fit
What affects prognosis in myeloma?
Worse if:
>2 lytic lesions
beta-2 microglobulin >5.5mg/L
Hb <11g/L
What causes death from myeloma?
Infection, renal failure.
What is MGUS?
Monoclonal gammopathy of undetermined significance. Incidental finding of a monoclonal Ig, increasing incidence with age. Precursor to myeloma. Present in 10% of over-85 year olds.
What is plasmapheresis?
Plasmapheresis is the exchanging of blood plasma or its components to and from the blood, done outside of the body.
(wikipedia)


