MSK Flashcards
Bone Cell Types
- osteoprogenitor cells
- unspecialized that develop into osteblasts
- osteoblasts
- form new bone, role in calcification and protein synthesis
- osteoclasts
- resorbing and breaking down bony matrix
- osteocytes
- mature osteoblasts in the bony matrix
Medical History
- age- problems vary by age (dislocation, overuse, etc)
- gender
- occupation/recreation
- family history (autoimmune, CA, osteoporosis)
- onset and progression of symptoms
- injury vs. “wear and tear”
- joint symptoms (stiffness, movement limitations)
- muscular symptoms
- skeletal symptoms (limb length discrepancy)
- joint pattern (how many affected, symmetrical or not)
- inflammatory vs non-inflammatory
- warmth and swelling
- morining stiffness (“gel phenomenon”)
- non: worsening w/ activity
- extra-articular vs. systemic
- usually autoimmune
- lung, kidney, etc. problems
- how disabling- ADLs
Physical Exam Components
- evaluate symmetrically and systematically
- inspection- deformity, swelling, erythema, asymmetry
- look at skin!
- palpation- tenderness, crepitation, warmth, synovial thickening
- ROM- active and passive, limited d/t muscle/nerve injury
- manual muscle testing- strength/resistance
- special testing
9 Categories of MSK Disorders
- local and regional
- cartilage degeneration
- inflammatory synovitis
- crystalline arthropathies
- enthesopathy
- joint space disease
- osteoarticular disease
- inflammatory myopathy
- general conditions
Local and Regional Conditions
- tendonitis, bursitis
- sprains- injury to ligaments
- I: partial tear, no instability
- II: partial tear, some instability
- III: complete tear
- strains- injury to muscle
- I: few torn fibers, fascia intact
- II: moderate amount of m. fibers torn, fascia intact
- III: tear all m. fibers w/ fascia intact
- loss of articular cartilage
- formation of osteophytes
cartilage degeneration
- primary
- biomechanical abnormalities leading to micro-fisures in the articluar cartilage
- secondary
- infection, autoimmune
- trauma or hypermobility of joint
- pigmented vilonodular synovitis (PVNS)
- thickening vascular swelling and infiltration of synovia
- autoimmune disease
inflammatory synovitis
- monosodium urate
- calcium pyrophosphate
- hydroxyapatite
crystal-induced synovitis
- gout
- pseudogout
- disorder of transition zone where tendons, ligaments and joint capsule attach
enthesopathy
- hallmark: spondyloarthropathies
- enthesis affected
- microorganisms in the joint
- extremely painful
joint space disease
- septic arthritis
- perform joint aspiration and fluid analysis, gram stain, cultures
- hemarthrosis
- blood in joint (can occur w/ ACL tear)
Osteoarticular Disease
- osteopenia
- osteoperosis
- osteonecrosis (typically w/ joint separation)
- periostitis
- painless inflammation and weakness of proximal skeletal muscles
inflammatory myopathy
- increased creatine kinase (CK) levels
- abnormal electromyography (EMG)
- histological abnormalities w/ biopsy
General Conditions
- polymyalgia rheumatic
- fibromyalgia
- complex regional pain syndrome
Initial Imaging Technique
x-ray
- tissue densities:
- air- black or dark gray
- fat- gray (lighter than air and darker than muscle or blood)
- water (blood and soft tissue)- shades of gray
- calcium in bone- white
- metal and contrast agents- bright white
- 2 views at right angles
- compare with old or bilateral views
X-ray Requirements
- Pt identification
- name, age, sex, birth date, medical record number
- location to image
- technical quality
- positioning of body part
- quality
- contrast
- continuous x-ray imaging
- used w/ procedures
- assess joint motion
flouroscopy
- used to evaluate joint soft tissue, muscle pathology, marrow structures, tumors
MRI
- expensive
- difficult to see bone, actually seeing fat in marrow
- T1:
- fat- bright
- water- dark
- T2:
- fat- dark
- water- bright
- blood, edema, CSF- white
MRI with contrast
MRI Arthrogram
- Gadolinium conatrast injected IV or intra-articular
- helps visualize small structure damage- labral tear
- C/I
- cochlear implants, some heart valves, pacemakers, spinal implants, brain aneurysm clips, metalic fragments in eye (some joint prosthesis- some made of non-magnetic materials)
- imaging joints not seen well with x-ray
- SI joint, vertebral bodies
- intra-articular fractures
- bony abnormalities in joint
- high radiation
- 360 degree x-ray 3-D reconstructions
CT scan
- contrast used to determine if mass is solid or cystic
Other Imaging
- test to measure bone mineral density (lumbar spine and proximal femur- T score and Z score)
- measure muscle function w/ needle inserted into muscle
- stimulate sensory/motor nerve w/ electrical impulse to measure conduction
- sometimes used to evaluate disc herniation or spinal cord compression
- increased blood flow w/ radionucleotide to ID tumors, fracures
- DEXA scan
- electromyography test
- nerve conduction study test
- myelogram
- nuclear medicine (Bone/PET scan)
- imaging using sound waves
- typically for prodedures- injections
Ultrasound
- images are grayscale
- high water = darker image (hyperechoic)
Common Ortho Labs
- inflammation markers
- autoantibody test
- antinuclear antibodies (ANA)
- cryoglobulins
- metabolic markers
- inflammation:
- C-reactive protein (CRP)
- Erythrocyte sedimentation rate (ESR)- sed rate
- CBC w/ diff
- autoantibody
- Rheumatoid factor (RF)
- antibodies to anti-cyclic citrulinated proteins (anti-CCP)
- anti-nuclear antibodies (ANA)
- Abx to DNA or pospholipids
- cryoglobulins (normally done by rheumatology)
- metabolic markers
- calcium, phosphorus, Vit D 25-dihydroxy, alkaline phosphatase
Synovial Fluid Analysis
- to ID cause
- septic arthritis, hemarthrosis, crystal arthritis, differentiate inflammatory vs. non-inflammatory arthritis
- r/o infection
- analyze:
- appearance (color)
- normal- clear, straw, wbc <200, PMN <25%
- noninflamm- clear, straw+, wbc 200-1000, PMN <50%
- inflamm- cloudy, yellow/green, wbc 1K-75K, PMN >50%
- septic- opaque, variable, wbc >50K, PMN >90%
- hemorrhagic- red
- volume
- wet prep
- cells, fibrin, collagen, cartilage, synovial fragments, rice bodies, crystals
- polarized light microscopy: ID crystals
- monosodium urate- gout
- calcium pyrophosphate dehydrate (CPPD)- pseudog
- hydroxyapatite- osteoarthritis
- RBCs, WBCs
- gram stain (an/aerobic, fungal)
- gonococcal (most common young adults)
- G+ s. aureus, s. pyogenes, s. pneumonia
- G- enterobacterieae, pseudomonas
- fastidious hemophilus, neisseria meningitides
- crystals
- appearance (color)
Joint Injection for Inflammation Reduction Drugs
Glucocorticoids
- stop production of inflammatory mediators: leukotrienes and prostaglandins
- max 3 injections per year
- increases pts blood sugar
- dexamethoasone sodium phosphate
- 1-2h onset, 12d duration
- hydrocortisone acetate
- 1-2d onset, 1-4w duration
- methylprednisone acetate (Depo-Medrol)
triamcinolone acetonide (Kenalog)
triamcinolone hexacetonide (Aristospan)
- 1-3d onset, 2-4m duration
Steroid Injection Contraindications
- joint infection
- overlying skin infection
- systemic bacteremia
- thrombocytopenia/bleeding disorders
- prosthetic joints
- osteonectrosis or fracture
- uncontrolled DM
- psoriatric plaques
- steroid allergy
Joint Injection for OA Pain
hyaluronate preparation
- hyaluronic acid is in synovial fluid- provides shock absorption
- brand names:
- Synvisc, Orhovisc, Euflexxa
- C/I
- infection
- overlying skin disease
- chicken/egg allergy
Complications of Corticosteroid Injections
- joint
- infection, hemorrhage, flare, steroid arthropathy (joint breakdown w/ too much steroid use)
- systemic
- facial flush
- worstening diabetic control
- supression of HPA axis
- iatrogenic Cushing syndrome
- local
- leakage along steroid tract
- atrophy of subcutaneous fat, depigmentation
- misplaced injections
- tendon rupture, nerve damage, cartilage injury, abscess
- rare
- pancreatitis
- hypersensitivity rxns
- uterine bleeding
- osteonecrosis
MSK Treatment Approaches
- conservative
- RICE- rest, ice, compression, elevation
- rehab
- meds
- Rx: NSAIDs, corticosteroids, pain relievers
- herbal: glucosamine and conjointin
- topical (except over surgical sites!)
- aspiration/injection
- bracing
- activity modification
- surgical
inflammation in subacromial space
(subacromial bursa, suprapsinatus tendon, acromion, coracoacromail ligament, biceps tendon)
- d/t overuse, repetition
- extremely common
- increases w/ age >30
- s/s, tests, dx
shoulder impingement
- s/s
- insidious onset or mild trauma
- deltoid/upper arm aching; dull at rest or sleeping
- rc pain referred to deltoid
- normal/near normal ROM
- full strength or mild weakness d/t inflammation
- tests
- Neer sign
- Hawkins-Kennedy sign
- x-ray (+/- bone spur), MRI (r/o tears, tendinosis)
- diagnosis: clinical
inflammation of long head of biceps
(frequently diagnosed w/ rotator cuff or superior labral patho)

bicipital tendinitis
- role of bicep: supination
- unknown cause
- s/s
- pain in bicep through bicipital groove
- rupture causes “Popeye muscle” deformity
- tests
- Speed’s sign
- Yerganson’s test
- tx
- conservative: PT, ice, subacromial/bicep injection, activity modification, NSAIDs
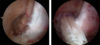
- surgical: arthroscopy w/ 6-8w recovery
impingement signs
- age >40-45
- +/- injury
- s/s, tests, dx

rotator cuff tear
- supraspinatus muscle torn typically- cuff arthropathy: humeral head rides up superiorly
- s/s
- gradually worsening pain, NIGHT PAIN
- +/- weakness
- tests
- drop arm
- empty can
- x-ray (+/- spur, cuff arthropathy)
- MRI
- possible US
- tx
- based on size, acuity, dysfunction, activity level
- no symptoms = no tx
- conservative
- rest, ice, NSAIDs, +/- injection, PT
- NO SLING- will get frozen shoulder
- surgery
- arthroscopic or open repair
shoulder pain, unable to move arm, deformity
- s/s, tests, dx

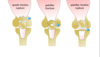
glenohumeral instability/dislocation
- s/s
- dislocation/subluxation vs. generalized- doesn’t affect just the shoulder
- may be trauma or genetic (adolescent)
- may have numbness or tingling
- check axillary n. (CN XI) - feel for deltiod contraction
- ALWAYS do neurovascular check before reduction/procedure
- Bankart Lesion- labrum torn w/ dislocation
- tests
- x-ray pre/post reduction to check for fractures- MUST HAVE AXILLARY VIEW
- for recurrent instability
- apprehension test (anterior/posterior)
- sulcus sign (inferior)
- load and shift test (anterior/posterior)
- tx
- traction/counter traction
- Stimpson hanging arm technique
- 1st- immobilize 2-3w, PT >4w, maybe surgery
- recurrent- arthroscopy vs. open surgery
common injury w/ overhead/throwing athletes, fall on outstreched arm or traction injury, increased tension on bicep tendon
- s/s, tests, dx

SLAP tear (Superior Labrum Anterior to Posterior)
- s/s
- pain anterior and deep
- +/- clicking
- weakness/pain w/ overhead activity
- normal ROM and strength
- tests
- O’Brien test
- Crank test
- GIRD: glenohumeral internal rotation deficit- lose ROM
- MR arthrogram (gold standard)- plain films will be normal
- tx
- grade 1-2: rest, ice, PT w/ scapular stabilizers, throwing protocol, core strengthening
- grade 3+: SLAP repair if <30-35; tenotomy or tenodesis if >35
progressively worsening pain, pain with ACROSS BODY ADDUCTION, rest of exam normal
- s/s, tests, dx

AC joint sprain/dislocation, OA/osteolysis
- sprain
- always lateral shoulder trauma (AC joint +/- CC ligs)
- tx:
- immobilize w/ sling ~2d, rest, ice, NSAIDs, PT
- surgery rare (grade 4+ only)
- OA/osteolysis
- conservative vs. open or arthroscopic excision/resection
pain, freezing and loss of motion of arm (external rotation)
- s/s, tests, dx

adhesive capulitis
- s/s
- freezing -> plateau -> thawing
- trauma, immobilization, thyroid disease, diabetics, women
- adhesions and thickening of joint capsule
- tests
- x-ray to r/o other causes
- NO MRI
- tx
- conservative: rest, ice/heat, PT, GH injection, NSAIDs, pain meds
- surgery:
- manipulation under anesthesia
- arthroscopy for lysis of adhesions
Shoulder Joint Injections
- subacromial space
- seated w/ forearm on lap
- inject ~1cm below posterior border of acromion
- directed medially, anteriorly, slightly superiorly 2-3cm
- glenohumeral joint
- posterior 2 fingers medial and posterior acromion border
- directed anteriomedial toward coracoid process
- bicipital tendon sheath
- sitting or supine
- externally rotate arm and mark point of max tenderness
- insert 30-45 deg into sheath AVOIDING tendon
- AC (acromioclavicular) joint
- seated w/ forearm in lap
- superior approach insert ~.5cm
- SC (sternoclavicular) joint
- sitting or supine
- anterior approach ~0.5cm
compression of brachial plexus +/- subclavian vessels
- s/s, tests, dx
thoracic outlet syndrome
- s/s:
- women 20-50
- trauma or mechanical stress, conginital: cervial rib, long C7 transverse process, fibrous tissue in thoracic outlet
- vague: neck, trapezious, shoulder/arm, supraclavicular pain or aching
- parasthesia (ulnar nerve commonly)
- color changes in arm
- fatigue
- WORSENING w/ ARM OVERHEAD
- bruits
- tests
- Adson’s maneuver
- elevated arm stress
- tx
- conservative
- rest, meds: NSAIDs, muscle relaxers, PT w/ postural awareness
- surgery- rare
- conservative
Elbow Physical Exam
- inspection
- edema, deformity, ecchymosis, atrophy
- palpation
- bony landmarks
- ROM at elbow
- flexion, extension, supination, pronation
- strength testing
- special tests
pain w/ use and TTP over tendon origin, pain with grip strength
- s/s, tests, dx
medial/lateral epicondylitis
- s/s
- overuse injury
- +/- weakness
- lateral pain- tennis elbow (common extensor)
- medial pain- golfer’s elbow (common flexor)
- tx
- conservative
- rest, ice, NSAIDs, +/- cortisone, injection bracing
- surgery (not common)
- drill holes in bone to advance healing
- conservative
pain in medial joint line
- types, s/s, tests, dx
collateral ligament injury
- radial collateral ligament (LCL)
- rare, usually associated w/ fracture or dislocation
- ulnar collateral ligament (MCL)
- repeated valgus stress (pitching), injuries rare
- s/s
- acute- pop then medial elbow pain
- chronic- no specific injury, just progressing pain
- ulnar paresthesia (ring/little finger)
- pain w/ ecchymosis
- tests
- valgus stress test
- MR arthrogram
- tx
- conservative: rest, NSAIDs, PT, throwing mechanics
- surgery- “Tommy John” UCL repair
tender mass at tip of elbow
- s/s, tests, dx

olecranon bursitis
- s/s
- acute or gradual
- direct blow, gout or crystalline deposits (gritty on palpation), infection (septic) bursitis requires surgery
- swollen, painful, sometimes red posterior elbow
- warm to touch
- remainder of exam benign
- tests
- aspirate and analyze WBC, crystals, gram stain/culture
- tx
- I&D and Abx
- NSAIDs, elbow pad, cortisone injection if no infection
- surgical excision (not common)
aching over medial elbow, numbness/tingling, claw hand
- s/s, tests, dx
cubital tunnel syndrome (ulnar neuritis)
- s/s
- medial elbow aching
- atrophy of hand
- direct blow vs. leaning on elbows or holding flex position
- check for deformity/carrying angle
- tests
- elbow flex test
- positive Tinel’s sign
- vibration and light touch perception- 2pt discrimination
- manual muscle testing
- finger abduction and adduction
- x-rays
- EMG/NCS
- tx
- conservative
- rest, avoid flexion, night extension splint
- surgery
- ulnar nerve decompression
- transposition- move nerve out of cubital tunnel
- conservative
pain and ecchymosis in antecubital fossa, “pop”,
“reverse Popeye” deformity
- s/s, tests, dx

distal bicep tendon rupture
- s/s
- pain and palpable defect in antecubutal fossa
- musce belly retracts w/ elbow flexion
- weakness w/ supination
- tests
- x-ray
- MRI
- tx
- surgery w/in 2 weeks of injury
- consider conservative if elderly, nondominant, partial
extreme swelling, pain, and inability to move elbow
- s/s, tests, dx

elbow dislocation
- s/s
- FOOSH
- terrible triad- dislocation w/ fracture of coronoid and radial head
- 80% posterior
- LCL always disrupted
- brachial a., median and ulnar nn. injured
- tests
- neurovascular check
- x-ray
- +/- CT scan
- tx
- reduction and splint under conscious sedation
- ROM start in 5-7d
Elbow Injections
- olecranon bursa
- elbow flexed, poserior 1cm distal to olecranon bursa
- 18g needle w/ 10ml syringe
- grasp bursa w/ other hand
- elbow joint
- seated w/ 45 degree elbow flex
- palpate center of lateral epicondyle, radial head, tip of olecranon triangle
- lateral epicondylitis
- seated w/ elbow flexed 90 degrees
- 1cm distal to epicondyle, point of max tenderness
- 22g needle
- medial epicondylitis
- seated w/ elbow extended 20 degrees
Wrist and Hand Exam
- inspection
- scars, atrophy, edema, erythema, deformity
- palpate
- bony and soft tissue
- ROM- active and passive
- especially if suspect tendon injury
- strength
- special testing
compression of median nerve
- s/s, tests, dx
carpal tunnel syndrome
- s/s
- female, repetition, DM, thyroid, RA, pregnancy
- 1st, 2nd, 3rd finger numbness and tingling
- worse at night
- muscle weakness- loss of grip and motor dexterity
- tests
- Tinel’s sign
- Phalen’s sign (*most useful)
- 2pt discrimination loss
- muscle atrophy
- EMG and nerve conduction studies
- tx
- conservative
- NSAIDs, activity modification, bracing, injection
- surgery
- open vs endoscopic
- conservative
swelling/stenosis in tendon sheath of snuff box
(abductor pollicis longis/extensor pollicis brevis)
-s/s, tests, dx
DeQuervain’s Tenosynovitis
- s/s
- pain +/- mild edema
- tests
- Finkelstein test
- tx
- injection, +/- bracing, PT
- rarely surgical release
“bump” on dorsum of wrist, volar radial wrist, base of finger
- s/s, tests, dx

ganglion cyst
- s/s
- fluid leaks from joint capsule/tendon synovial sheath
- vary in size +/- pain
- transilluminate
- can compress medial nerve and radial artery
- tx
- conservative
- NSAIDs, rest, wrist splint
- aspiration- WATCH radial artery
- surgical
- if recurrent painful cyst or N/V compromise
- conservative
finger/thumb deformity with pain, swelling, ecchymosis after injury
- s/s, tests, dx

thumb/finger dislocations
- s/s
- tearing of collateral ligament/volar capsular ligament
- check for joint stability 1-2w later
- tests
- x-ray to r/o fracture
- tx
- conservative- taping
forced abduction of thumb
- s/s, tests, dx
gamekeeper’s (skier’s) thumb
- s/s
- tear of ulnar collateral ligament (UCL) of MC joint
- pain, swelling, ecchymosis
- tests
- valgus stress test
- x-ray to r/o fracture
- +/- MRI if suspect rupture
- tx
- conservative vs. surgical if UCL ruptured
finger “feels locked” and palpable nodule with flex/extension
- s/s, tests, dx

trigger finger
- s/s
- pain and catching
- thickening of flexor tendon sheath- a1 pulley
- mostly long and ring finger
- female, RA/DM
- worse after inactivity
- tx
- conservative vs. surgical
finger flexion weakness following injury
- s/s, tests, dx

flexor tendon injuries
flexor digitorum profundus (FDP) & digitorum sublimis (FDS)
- s/s
- “Jersey finger”- ring finger most common
- swelling, ecchymosis
- TTP at distal phalanx
- associated w/ RA/OA
- tests
- test flexion at PIP and DIP
- tx
- surgical repair
- *** DOCUMENT evaluation with every finger/hand cut ***
flexed PIP and hyperextended DIP
- s/s, tests, dx

boutonniere deformity
- s/s
- rupture extensor central slip
- tests
- x-ray to r/o fracture
- tx
- extension splint to PIP
- 6w if youger, 3w if older
blunt trauma to finger tip w/ swelling, ecchymosis, deformity
- s/s, tests, dx

mallet finger
- s/s
- rupture to extensor tendon at DIP
- tests
- x-ray to r/o fracture
- tx
- RICE
- extensor splint all times for healing
- surgery for large avulsion
hyperextension of PID/flexion of DIP
- s/s, tests, dx
swan neck deformity
- s/s
- weakening of volar plate
- RA/nerve disorders
- pain and swelling
- tests
- x-ray
- tx
- conservative vs. surgical

infection of soft tissue around fingernail
- s/s, tests, dx

paronychia
- s/s
- pain and swelling around nail
- tx
- digital block and drainage
- oral abx
- cephalexin (Keflex) 500mg po q6h 10d
- tmp/smx (Bactrim DS) 1 po q12h 10d
- clindamycin (Cleocin) 300mg 1 po q8h 10d
finger pulp infection
- s/s, tests, dx

felon
- s/s
- puncture wound (usually thumb or index)
- sever pain and swelling
- tense, red, swollen, very tender
- tests
- S. aureus pathogen
- tx
- digital block w/ surgical drainage
- abx: Keflex or Bactrim
fight bite in index, middle, ring finger
- s/s, tests, dx
septic flexor tenosynovitis
- s/s
- puncture wound
-
Kanavel’s 4 cardinal signs
- intense pain w/ extension
- flexion posture
- fusiform swelling
- tenderness along flexor tendon sheath
- tests
- CBC, ESR, sed rate
- x-ray
- tx
- call hand service
- SURGICAL EMERGENCY **DO NOT MISS
- Abx
- poor prognosis- usually residual stiffness, loss of ROM
clear fluid filled vesicles on finger
- s/s, tests, dx

herpetic whitlow
- s/s
- pain, swelling
- tests
- herpes simples 1 or 2
- tx
- conservative- DO NOT DRAIN these
- +/- antivirals
Lower Extremity Physical Exam
- inspection
- LL length/alignment, deformity, muscle atrophy, pelvic obliquity, Q-angle
- Q-angle:
- female 17 deg, male 14 deg
- angle of ASIS to middle patella to mid tibia
- stresses medial side of knee + foot pronation
- Q-angle:
- gait analysis
- LL length/alignment, deformity, muscle atrophy, pelvic obliquity, Q-angle
- palpation
- bony prominences, soft tissue, joint line
- ROM
- manual muscle testing (MMT)
- special tests
Hip Anatomy Terminology
- ischial tuberosity
- anterior tilt- downward tilt w/ hip extension
- posterior tilt- hip flexion
- lateral tilt
- pelvic rotation w/ walking
- diarthroidal- movement in 3 planes
- hip pain- anterior to seam line of pants
- back pain- posterior to seam line of pants
- femoral neck angle
- anteversion- smaller angle than normal (foot in)
- retroversion- larger angle than normal (foot out)
- coxa vara- inclination <125 degrees
- coxa valga- inclination >125 degrees
Hip Exam Special Tests
- Trendelenburg Test/Sign
- hip drop opposite affected gluteus medius/minimus
- Thomas test
- hip flexor contracture/psoas tightness (knee to chest)
- log roll test
- pain w/ internal leg rotation- acetabular/femoral neckpathology
- FABER (Patrick) test
- flexion-abduction-external rotation (cross leg while lying)
- SI joint or hip problem
- Hamstring flexibility
- passive SLR 80 degrees
- knee extension should be 5-15 degrees of straight
pain and swelling of thigh, +/- ecchymosis, +/- palpable defect
- s/s, tests, dx
hip strain
- s/s
- TTP
- pain with stretching or resistance to MMT
- tx
- RICE, NSAIDs, pain relievers, PT
- surgery- avulsion injuries
lateral hip/thigh pain
- s/s, tests, dx
hip bursitis - trochanteric bursitis
- s/s
- most common hip bursitis
- lumbar spine OA/scoliosis, length discrepancy, trauma
- runner, female, middle age to elderly
- pain at rest and activity
- difficulty ambulating
- TTP greater trochanter
- pain w/ abduction
- tx
- RICE
- cortisone injection
- NSAIDs, pain reliever
- weight loss
- rehab: stretch/strengthen gluteus medius and IT band
buttock, labial/scrotal pain
- s/s, tests, dx
piriformis syndrome
- s/s
- pain w/ sitting or getting out of bed
- pain w/ hip adduction
- difficulty sitting
- absent neurological signs
- TTP SI joint, gluteal muscles, greater sciatic notch
- tests
- piriformis test
- Lasegue sign- leg lifted and straight, flex knee and cross
- x-ray, MRI, CT to r/o other causes
- EMG to differentiate btw piriformis and herniated disk
- tx
- NSAIDs, PT, +/- injection
- surgery?
clicking, popping, locking hip with lateral pain
“C sign”
- s/s, tests, dx
femoral acetabular impingement
- s/s
- osseous deformity of acetabular rim, femoral head/neck junction
- causes labral tear and articular cartilage microtrauma
- from overuse
- tests
- decreased flex and IR
- +FIDDIR
- x-ray (AP and lateral)
- MR arthrogram
- tx
- conservative vs. surgical
high trama impact to leg in seated position
- s/s, tests, dx
hip dislocation
- s/s
- obvious deformity
- tests
- check distal pulses and nerve status, knee
- x-rays (AP and lateral)
- CT if fracture suspected
- tx
- reduction ASAP
- if no fracture w/ PWB and advance as tolerated
pain in groin, lateral hip or buttock; worse w/ weight bearing; catching/popping sensation
- s/s, tests, dx
osteonecrosis
- s/s
- bone death- collapse of femoral head
- risks: corticosteroid use, alcohol abuse, trauma, sickle cell, RA, lupus
- Trendelenburg gait
- decreased/painful ROM
- tests
- pain w/ straight leg raise
- +log roll
- x-ray, MRI or CT
- tx
- w/out collapse
- core decompression
- vascularized fibular grafting
- w/ collapse
- arthroplasty (replacement)
- w/out collapse
loss of articular cartilage in hip
- s/s, tests, dx
hip osteoarthritis
- s/s
- childhood disease, trauma, osteonecrosis, infection
- anterior groin/thigh pain (worse at night)
- pain w/ activity and progresses to constant pain
- popping, catching grinding
- fixed external rotation and flexion contracture
- tests
- x-rays
- tx
- conservative
- pain control, activity modification, assistive devices
- surgery
- osteotomy
- total hip arthroplasty
- conservative
ASIS compression
- s/s, tests, dx
lateral femoral cutaneous nerve entrapment
- s/s
- pain and dysethesia of lateral thigh
- decreased sensation but pressure or tapping over nerve increases symptoms
- no muscle or abnormal reflexes
- tests
- plain films- r/o abnormalities
- CT/MRI- r/o pelvic or abdominal masses
- tx
- weight loss, loosening tigh clothing
- meds
- cortisone injection
- surgical release of nerve rarely done
Knee Physical Exam Technique
- inspection
- gait, alignment, feet, discoloration, effusion, atrophy
- palpation
- quad/patellar tendon, joint line, MCL/LCL, bursa, popliteal fossa
- ROM
- knee flexion 0-130 degrees (up to 10 percent of hyperextension)
- manual muscle testing
- grading scale
- special test
Knee Special Tests
- apprehension test
- move patella laterally: +if pain, apprehension, quad contraction
- J sign
- excessive lateral patellar shift in terminal extension (up and out)
- McMurray’s test- meniscus
- leg lifted w/ knee at 90 degree angle then…knee out/foot in to knee in/foot out
- try to catch popping or catching
- anterior drawer/Lachman’s test- ACL
- ACL prevents anterior translation of tibia and posterior translation of femur
- posterior drawer/posterior sag sign- PCL
- valgus stress test- tests MCL
- knee pressed in, ankle pressed out
- varus stress test- tests LCL
- knee pressed out, ankle pressed in
swelling, redness, pain decreased ROM, +/- atrophy in knee
- s/s, tests, dx
bursitis
- s/s
- pre-patellar- inflamed (trauma related) or septic
- pes anserine- early medial compartment OA
- overuse, injury, break in skin
- tx
- aspirate to r/o infection
- NSAIDs, activity modification, compression
- surgery rarely to resect (normally resolves on own)

anterior knee pain w/ running, jumping, kicking
tendinitis
- quadriceps tendon- above patella
- patellar tendon- “jumper’s knee”, inferior patella
- s/s
- TTP on bony prominences/tendon
- pain w/ resisted knee extension
- full ROM
- +/- swelling
- tests
- plain films
- tx
- RICE, NSAIDs, activity modification, PT (hamstring stretches), knee strap/sleeve

knee effusion (giving off liquid), palpable defect, can’t extend leg against gravity when seated or straight leg raise when lying
- s/s, tests, dx
tendon ruptures (quad, patella fracture, patellar)
- s/s
- fall on partially flexed knee
- pain, swelling, inability to ambulate
- discoloration
- tests
- plain films to r/o fracture
- MRI
- tx
- surgery
diffuse anterior knee pain, worse after long sitting, stairs, jump/squat, catching or grinding behind patella
- s/s, tests, dx
patellofemoral syndrome
- s/s
- overuse of overloading of joint
- worse w/ activities the load front of joint
- chondromalacia- pathologic changes of articular cartilage (softening of cartilage)
- observe alignment while weight bearing- foot pronation, femoral anteversion, genu valgum, vastus medialis oblique atrophy
- tests
- Q-angle, J sign, patellar apprehension sign
- assess hamstring tightness and quad strength- weak quads put more sheer force across patellofemoral joint
- plain films
- tx
- activity modification, NSAIDs, bracing
- PT- flexibility and strengthening
severe knee pain, inability to ambulate, patella lateral
- s/s, tests, dx
lateral patellofemoral instability
- s/s
- direct contact or sudden change in position
- usually spontaneously relocates
- deformity, swelling
- tests
- apprehension sign
- TTP medial patella
- plain films
- MRI to r/o soft tissue damage
- tx
- conservative
- RICE
- +/- aspiration
- braced in extension
- NSAIDs, pain meds
- PT- quad strengthening, flexibility
- surgery
- if recurrent dislocation or conservative failure
- MPFL repair
- conservative

intermittent pain in knee w/ catching, locking, popping, giving out that can come and go
- s/s, tests, dx
meniscus tears
- s/s
- acute w/ twisting, squatting, change in position
- swelling
- joint effusion and joint line tenderness
- decreased ROM- EMERGENCY IF CANNOT EXTEND
- +/- quad atrophy (quad shuts down w/ knee injury)
- +/- locked knee
- tests
- McMurray test
- plain films- weight bearing
- MRI
- tx
- conservative
- RICE, pain control, PT
- surgery
- meniscectomy vs. meniscal repair
- inner cut out (no circulation) while outer stitched
- conservative

excessive joint fluid tracts to popliteal bursa
- s/s, tests, dx
baker’s cyst
- s/s
- most common cyst in knee
- associated w/ degenerative meniscal tears
- popliteal swelling/fullness and pain
- calf pain and swelling if ruptures (may think DVT)
- tests
- plain films
- MRI other pathlology suspected
- tx
- conservative
- rarely surgery for fear of transecting popliteal nerve

knee pain, immediate joint effusion, instability, decreased ROM, hemearthrosis - deceleration, hyperextension
- s/s, tests, dx
ACL tear
- s/s
- effusion
- decreased muscle strength
- antalgic gait
- +/- “pop”
- tests
- +Lachman’s exam
- pivot shift test
- anterior drawer
- plain films, MRI
- tx
- RICE, ROM
- surgical reconstruction if younger, active (need full ROM before surgery)
force to anterior tibia w/ flexed knee
- s/s, tests, dx
PCL tear
- s/s
- pain, joint effusion, +/- instability
- decreased ROM
- tests
- posterior drawer test
- posterior sag
- x-ray/MRI
- tx
- depends upon degree of instability
valgus or varus grade I / II / III
evaluated and 0 and 30 degrees extension (more play at 30 deg)
- s/s, tests, dx
collateral ligament sprain
- s/s
- pain, swelling, stiffness, +/- instability or mechanical symptoms
- TTP over ligament/attachment
- tests
- plain films, MRI
- tx
- MCL- conservative if isolated or grade 1-3
- LCL- conservative grade 1-2, surgical grade 3

pain, mechanical symptoms, creptius in knee, +/- effusion
- s/s, tests, dx
chondral/osteochondral defect (OCD)
- s/s
- direct trauma, articular cartilage injuries
- tests
- plain films to check for loose bodies, MRI
- tx
- conservative
- surgical
- microfracture- punch holes in bone
- OATS- punches of outer articular cartilage place on points of greater weigth bearing
- autologous chondrocyte implantation
Foot and Ankle Exam
- inspection
- gait analysis, hindfoot analysis
- palpation
- anterior joint line, malleoli, sinus tarsi, achilles tendon, metatarsals, peroneal tendons, posterior tibial tendon
- ROM
- manual muscle testing
- special tests
- anterior drawer test
- draw foot anteriorly
- Thompson test
- feet hanging off bed, calf squeezed, foot should move if achilles intact, torn if no movement
- inversion stress test
- foot inverted while holding ankle
- eversion stress test
- foot everted while holding ankle
- interdigitation neuroma test
- foot squeeze test
- web space compression tenderness test
- anterior drawer test
pain, swelling, ecchymosis in ankle w/ inversion or eversion
- s/s, tests, dx
ankel sprain
- s/s
- inversion: anterior/posterior talofibular lig, calcaneofibular lig, tibiofubular lig, subtalar lig
- eversion: deltoid lig
- TTP
- palpate/assess 5th MT ALWAYS- don’t miss Jones fx
- palpate/assess achilles tendon ALWAYS
- tests
- anterior drawer
- squeeze test
- external rotation test
- x-ray, MRI, MR arthrogram (looking for uniformity around talus)
- tx
- goal: prevent chronic instability and pain
- conservative- rehab
- surgical- rare
sudden/severe pain near heel, “someone kicked me in the ankle”
- s/s, tests, dx
achilles tendon rupture
- s/s
- swelling, ecchymosis, difficulty ambulating
- palpable tendon defect
- tests
- Thompson’s test (most reliable w/in 48 hrs)
- plain films, ?MRI
- tx
- non-surgical: serial casting
- surgical
- tendon retraction- based on activity level, age, risk

vague paresthesis of plantar foot, compression of tibial nerve
- s/s, tests, dx
tarsal tunnel syndrome
- s/s
- worse after walking/exercise
- relieved w/ rest
- night pain
- TTP over tarsal tunnel (posterior to medial malleolus)
- decreased sensation
- tests
- Tinel sign
- plain films
- MRI to r/o other patho/space occupying lesions
- EMG/NCS not accurate at ankle and below
- tx
- conservative
- injection, orthotics
- surgical- poor outcomes
- conservative
insideous onset heel/foot pain w/ worse “start up pain”
- s/s, tests, dx
plantar fasciitis
- s/s
- increased pain w/ standing and walking
- TTP medial calcaneal tuberosity
- toe dorsiflexion increases pain
- tests
- plain films
- entheseophyte- heel spur (but not source of pain)
- tx
- conservative
- orthotics, night splint, PT, NSAIDs, injections, acupuncture
- rarely surgical
- conservative
posterior tibial tendon dysfunction
- s/s, tests, dx
pes planus - flat foot
- s/s
- classic presentation- mid 50, female, overweight
- RF: corticosteroid injections, DM, HTN, prev foot injuries
- insidious onset pain and swelling in media ankle
- ankle rolls and lost arch
- sinus tarsi pain
- hindfoot valgus- “too many toes”
- unable to toe raise
- tests
- plain films, ?MRI - thickening of tendon
- tx
- conservative
- casting, orthotics, PT
- surgical
- tendon transfer / osteotomy
- conservative

forefoot pain
- s/s, tests, dx
metatarsalgia
- s/s
- abnormal metatarsal lengths, toe deformities: claw/hammer
- pain w/ activity
- callus formation- intractable plantar keratosis
- pain, swelling, MTP joint stability
- digital nerve function
- ddx
- plantar wart: anywhere on sole, punctate hemorrhage, fibrillated texture
- tests
- plain films
- tx
- conservative
- metatarsal pad, removal of callus, orthotics, PT, shoe wear
- surgical
- realign toes and/or metatarsal heads
- conservative

perineural fibrosis of common digital nerve
- s/s, tests, dx
interdigital (Morton) neuroma
- s/s
- 3rd-4th toe webspace
- plantar forefoot pain
- dysesthesias of 2 affected toes
- rarely at night
- “feels like walking on marble”
- tests
- squeeze test
- assess MTs
- sensory exam (ANYTIME a nerve is involved)
- plain films, MRI/US to r/o other causes
- tx
- conservative
- metatarsal pad, shoe change, corticosteroid injection
- surgical
- excision
- conservative

lateral deviation of great toe at MTP joint
- s/s, tests, dx
hallux valgus (“bunion”)
- s/s
- pain, swelling, numbness or tingling
- tests
- plain films
- tx
- conservative
- shoe wear, orthotics, PT- biomechanical evaluation
- surgery
- conservative

1st MTP joint sprain
- s/s, tests, dx
turf toe
- s/s
- pain, swelling, ecchymosis
- +/- ligamentous
- common in athletes
- hyperextension of MTP
- tests
- plain films
- MRI to r/o other causes
- tx
- conservative
- orthotic devices, stiff soled shoes
- surgical (rare)
- only if displaced intra-articular or avulsion fracture
- conservative
Toe Deformities
- hammer toe
- PIP flexion deformity (no DIP or MTP deformities)
- claw toe
- MTP extension w/ PIP flexion
- mallet toe
- DIP flextion
- s/s
- swelling, pain, deformity, shoe calluses
- tests
- evaluate sensory and motor of lower extremity
- tx
- conservative
- shoe wear, splints
- surgical
- fix deformities
- conservative

brachial plexus innervations

lumbar plexus innervations

cervical spine test
spurling test
- narrows neural foramen
- increases/reproduces redicular symptoms
- pain
- base of skull to thoracic region
- SCM / trapezious muscles
- < ROM
- headache
- sleep disturbances
- fatigue
- difficulty concentrating
- +/- radicular symptoms
- pain, numbness, tingling
cervical sprain / strain
- PE
- +/- swelling, tenderness, limited ROM
- neurologic exam usually normal
- tests
- x-rays
- Tx
- meds: NSAIDs, pain meds, muscle relaxers, steroids
- +/- cervical collar or neck roll
- massage, stretching, PT
- DISCUSS tx options (time off, rest, ice/heat, chiro)
- self limited (4-6w)
- whiplash (6-12m)

lumbar spine tests
- straight-leg raise
- check for herniated disk
- pain w/ lifting asymtomatic leg
- seated straight leg raise
- creates sciatic tension
- patient will lean back to reduce pain (+)
- __FABER test
- flexion-abduction-external rotation (figure 4 postion)
- hip and SI joint pathology
tests for “non-organic” pain
Waddell signs
- non-organic tenderness
- axial simulation/torso rotation
- seated straight-leg raise
- sensory examination
neural foramen narrowing, disc herniation, bone spur
- limited mobility
- chronic neck pain - worse w/ upright activity
- paraspinous muscle spasm
- headaches
- radicular symptoms
- interference w/ ADLs
- myelopathy symptoms
PE, tests, Tx
cervical spondylosis
- PE
- tenderness, decreased ROM w/ pain, gait/sensory analysis
- tests
- Spurling, Babinski, Brudzinski-Kernig, ankle clonus
- x-ray, MRI, CT myelogram
- Tx
- degeneration will continue w/ time
- conservative vs. surgical
- decompression and fusion

- LBP
- radicular pain to buttocks/posterior thigh
- difficulty ambulating, sleeping, finding comfortable position
- bowel or bladder dysfunction (S2-S4)
- saddle anesthesia
- weakness in lower exremeties
PE, tests, Tx
cauda equina syndrome
(compression of n. roots distal to conus medullaris)
- PE
- unable to heel toe walk
- anal sphincter tone
- tests
- MRI, CT myelogram
- Tx
- IMMEDIATE decompression surgery

neurogenic pain in nerve roots
- +/- associated numbness, weakness, loss of reflexes
- neck and radiating pain w/ numbness and tingling
- muscle spasms
- muscle weakness
- headaches
- relief when hand raised over head
cervical rediculopathy
- can be caused by disc herniation or degenerative changes
- abrupt vs. insidious
- LBP w/ unilateral radicular leg pain
- exacerbated w/ walking, sitting, standing, coughing
- radiates from buttocks to foot or follows dermatome to anterior aspect of thigh not past knee
PE, tests, Tx
lumbar herniated disk
- PE
- list/trunk shift
- sciatica
- seated asymptomatic leg raise (specific to herniated disk)
- tests
- plain films - degenerative changes
- MRI if neurologic changes/intolerable pain
- Tx
- conservative
- NSAIDs, rest, PT
- epidural steroid injections
- manipulative therapy, traction, acupuncture
- surgical
- microdiscectomy, laminectomy
- conservative

neurological deficit d/t compression of spinal cord
- gradual onset
- long-tract signs
- palmar parathesia
- decreased finger dexterity
- subtle gait disturbances
- abnormal urinary function
- lack of pain
- loss of vibration/position sense
tests, PE, Tx
myelopathy
- tests
- Babinski sign
- Brudzinski-Kernig test (head lift - leg lift/abduct)
- ankle clonus (foot dorsiflex)
- x-ray, MRI, CT myelogram, EMG/NCS (neuropathy vs compression)
- PE
- TTP, decreased ROM, decreased lordosis, +/- Spurling
- shoulder pain does not radiate past elbow (cervical)
- Tx
- delayed leads to paralysis, weakness, chronic pain
- conservative
- spontaneous resolution in 2-8w
- NSAIDs
- cervical traction
- NO SPINAL MANIPULATION (no chiropractor)
general low back or SI joint tenderness
- doesn’t radiate past the knee
PE, tests, Tx
lumbar sprain/strain
- PE
- decreased ROM, motor/sensory exam (L4-S1), special tests to r/o other structures
- tests
- +/- plain films
- MRI not indicated
- Tx
- conservative
- pain control, PT/HEP, pt education
- provide options for shared decision
- get them back to work
- conservative
LBP > 90 days (3m)
- LBP radiating to 1 or both buttocks
- worse w/ bending, lifting, stooping, twisting
- stiffness
- intermittent pain down leg
- relief w/ lying
PE, tests, Tx
chronic low back pain
- PE
- TTP lumbar and/or SI joint, decreased ROM, normal motor/sensory exam, positive SLR
- tests
- plain films (look for degenerative changes)
- MRI (evaluate structural changes)
- Tx
- pt education
- pain management (watch narco abuse)
- psychological testing
- injections
- biofeedback
- cognitive/behavior conditioning
- psychotherapy
- detoxification programs
4 cervical vetabrae fractures
PE, tests, Tx
- Jefferson fracture / C1 burst fracture
- Hangman’s fracture (C2 pedicles)
- Clay-shoveler’s fracture
- C7 > C6 > T1
- Avulsion fracture
- PE
- MOI specific: severe neck/back pain, paraspinous muscle spasm, bony tenderness, +/- neurologic
- tests
- plain images: AP, lateral, odontoid
- Tx
- immobilization
- Methylprednisone 30mg/kg bolus, then 5.4mg/kg/h drip 23h
- conservative vs. surgical intervention

neurogenic claudication
- fatigue and weakness from proximal to distal
- sitting or lying relieves pain
- narrowing of lumbar spine w/ nerve root compression
- order of commonality: L3/4 -> L4/5 -> L2/3
PE, tests, Tx
spinal stenosis
- PE
- +/- proprioception, reflexes, urine/bowel (spincter tone rarely affected)
- tests
- Romberg test (balance lost w/ eyes closed)
- x-rays to T10
- MRI
- EMG/NCS
- Tx
- conservative
- pain control, PT, water therapy, body mechanics
- surgical
- quality of life
- decompression and spinal fusion
- conservative
lumbar fracture

- stabbing, knife-like pain in buttocks/posterior leg(s)
- worse w/ prolonged sitting, twisting, rotating
- trauma, leg-length inequality, tight iliopsoas, scoliosis, hip OA, pregnancy
PE, tests, Tx
SI joint dysfunction
- PE
- TTP
- normal motor/sensory findings
- tests
- FABER test
- compression test (push on ASIS and rock patient)
- plain films
- CT scan
- Tx
- conservative
tailbone pain
- pain w/ sitting, BM, sexual intercourse
PE, tests, Tx
coccydynia
- PE
- TTP rectally
- GI/gynocological exams
- tests
- plain films
- MRI to r/o other
- Tx
- conservative
- PT, change activity, nerve block, 6m-1y recovery
- surgical
- coccygectomy
- conservative
pars interarticularis defect / forward translation of vertebrae
- repetetive hyperextension
- back pain w/ movement
- radiculopathy
PE, tests, Tx
spondylolysis / spondylolisthesis
- PE
- loss or lordosis
- decreased strength after walking
- SLR
- tests
- x-ray
- Tx
- conservative
- weight loss
- surgical
- stabilize defect if skeletally immature
- conservative
lateral curvature in spine
- +/- pain
- radiculopathy (L4/5 common)
- extensor hallicis longus weakening
- getting shorter/developing hump
- cardiopulmonary decompensation rarely
PE, tests, Tx
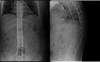
scoliosis
- PE
- neuro exam for reflexes, motor, sensory function
- gain analysis
- tests
- full-length PA and lateral films
- EMG (radiculopathy vs. neuropathy)
- Tx
- skeletally immature
- observation, bracing (25-45 deg), fusion (>45 deg)
- Milwaukee or Boston brace
- mature
- conservative tx, surgical if curve >50-60 deg
- skeletally immature
- back pain w/ weight bearing activities relieved by rest
- pain a night
- +/- constitutional symptoms (weight loss, fever, decreased appetite, night sweats, fatigue)
PE, tests, Tx
metastatic disease
- PE
- inspect for deformity
- TTP
- neuro exam
- tests
- AP/lateral plain films
- bone scan to ID other areas of mets
- Tx
- dependent on tumor
- decompression and stabilization w/ postop radiation
these spinal fracture uccur mostly d/t osteoporosis/weakening
thoracic vertebral fractures
vertebral fracture goal, type, tx
- goal - prevent neurologic injury, restore stability/normal fx
- types
- avulsion
- compression
- fracture/dislocation
- tx
- spinal fusion
- cervical
- soft collar, Philadelphia collar, rigid orthosis, halo
- thoracic
- corset, 3-point orthosis, clamshell
- lumbar
- elastic belt, corset, rigid orthosis
crystal deposition disease characteristics & 2 types
- sudden onset of severe joint pain and swelling
- usually 1 joint
- crystals found in synovium, cartilage, surrounding tissue
- types
- gout - monosodium urate crystals (MSU)
- calcium pyrophosphate dehydrate crystals (CPPD)
- pseudogout - synovitis
- chondrocalcinosis - deposits in soft tissue
disease / 4 phases / causes
- urate saturation in blood/body fluids
- hypertension, metabolic syndrome, obesity
- thiazide diuretics / low dose ASA
- diet:
- high purine: organ meat, select seafood
- high-fructose corn syrup
- excessive alcohol: beer/distilled liquors
- protective:
- Vit C, coffee, cherries
hyperuricemia
- phases
- asymptomatic (>7mg/dL)
- acute gouty flare
- intercritical gout (intervals between attacks)
- chronic tophaceous gout
- causes
- underexcretion (90%)
- kidney, HTN, obesity, lead, drugs
- overproduction
- diet, obesity, psoriasis, nicotinic acid (B3)
- underexcretion (90%)
gout
s/s, test, tx
- s/s
- sudden onset, cardinal signs inflammation, +/- constitutional
- 1st metatarsophalangeal joint (Podagra), ankle, midfoot, knee
- subcutaneous tophus: fingers, wrists, ears, olecranon bursa, achilles tendon
- tests
- synovial fluid analysis: crystal negative birefringement
- rod-shaped crystals
- +/- serum urate level
- x-ray (r/o fracture), US to look for crystals
- Tx
- lifestyle modifications
- acute: RICE, NSAIDs, Colchicine, corticosteroids
- meds
- xanthine oxidase inhibitor (overproduce/underexcr)
- Allopurinol 100mg PO daily
- Febuxostat 40mg po daily
- increase renal excretion (underexcr)
- Probenecid 250mg po daily
- Pegloticase 8mg IV q2w (warn: anaphylaxis, $$$)
- xanthine oxidase inhibitor (overproduce/underexcr)
calcium phyrophosphate dihydrate crystal deposition disease
(CPPD crystal deposition disease)
3 types, s/s, tests, Tx
- types (more common in women, gout in men)
- pseudogout - acute synovitis
- knee most common
- chondrocalcinosis - calcification in hyaline cartilage
- asymptomatic, incidental finding
- pyrophosphate arthropathy - OA w/ CPPD
- pseudogout - acute synovitis
- tests
- x-ray
- synovial fluid analysis
- postitive bifringement (square crystals)
- Tx (if symptomatic)
- RICE, NSAIDs, corticosteroids, +/- Colchicine
3 Hydroxyapatite Arthropathy Diseases
- crystals in joints, tendons, ligaments, bursa
- identified w/ electron microscopy
- species of basic calcium phosphate
- pts tend to be younger
- calicific tendinitis
- sudden shoulder pain w/out MOI
- pain->plateaus->pain when resolving->no pain
- tx conservative or surgical (usually resolves on own)
- Milwaukee shoulder
- crystals destroy RC and shoulder joint
- DISH (diffuse idiopathic skeletal hyperostosis)
- bridging in cervical spine
MSK infection
- superficial > deep
- olecranon, prepatellar, infrapatellar, 1st MTP
- redness, warmth, swelling
- typically no ROM restriction (if joint infection, pt will not move)
PE, tests, Tx
septic bursitis
- PE
- aspirate to r/o infection
- acute: S. aureus, B hemolytic strep, psuedomonas
- chronic (think systemic): B abortus, M. tuberculosis
- aspirate to r/o infection
- tests
- x-ray to r/o other, look for foreign body
- Tx
- outpatient
- PCN or 1st gen cephalosporin
- tri/sulfa (Bactrim) if MRSA
- Clindamycin or Linezolid if PCN allergy
- inpatient
- Nafcillin, oxacillin, cefazolin IV
- Vanco, daptomycin, linezolid if MRSA
- outpatient
MSK infection
- very painful, red, swollen, hot joint (knee typical)
- decreased ROM
- +/- fever
- IV drug use (SC or SI joint), diabetes, alcohol, immuno
- UTIs / indwelling catheters
- injury
PE, tests, Tx
septic arthiritis (infection to joint)
- PE
- tests
- x-rays: ususally normal, soft tissue swelling
- radiolucent lines if prosthetic infection
- MRIs
- identify osteomyelitis
- bone scan for associated osteomyelitis
- labs
- synovial fluid analysis
- WBC > 50,000, low glucose, high protein
- ESR & CRP
- synovial fluid analysis
- cervical/urethral cultures if +gonococcal
- x-rays: ususally normal, soft tissue swelling
- Tx
- surgery
- IV antibiotics (4-6w)
infection of the bone
PE, tests, Tx
osteomyelitis
- PE
- trauma, surgery, immuno, systemic disease
- localized bone pain
- +/- sinus tract, swelling, abscess, constitutional
- tests
- biopsy/culture of affected area (GOLD standard)
- CBC - leukocytosis
- elevated CRP/Sed rate
- plain films
- MRI - marrow changes
- CT - early cortical erosions
- bone scan (highly sensitive, low specificity)
- Tx
- debridement and excision of infected bone
- abx spacer
- IV abx
- Abx impregnated methylmethacrylate beads
- debridement and excision of infected bone

- loss of articular cartilage (trauma, obesity)
- extra-articular organs not affected
- pain affecting sleeping
- stiffness lasting <30 min (worse w/ inactivity)
- swelling
- joint instability
- locking and grinding
PE, tests, Tx
osteoarthritis
- PE
- joint effusion, crepitus, antalgic gait, decreased ROM, muscle atrophy
- +/- deformity
- knees: genu varum (bow) vs. valgum (knock)
- hands:
- Bourchard nodes (PIP)
- Heberden nodes (DIP)
- tests
- x-ray: joint space narrowing, osteophytes, sclerosis
- MRI: r/o other sources of pain (not routinely used in OA)
- no US
- no specific labs
- Tx
- conservative as long as possible
- RICE, bracing, corticosteroid injections
- meds
- NSAIDs, tramadol, glucosamine/chondroitin
- NO opiates
- PT
- patient education- activity, occupation, weight loss
- CAM: accupuncture, Tai Chi, supplements
- surgical
- NO arthroscopy
- joint replacement
- conservative as long as possible
autoimmune attack of synovial tissue/joints
- genetics (+ family history)
- female
- age, smoking, coffee 3+/day
PE, tests, Tx
rheumatoid arthritis
- PE
- symmetric polyarthritis, deformities
- morning stiffness
- isidious onset w/ distal joints first - MCP, PIP (spares DIPs, toe IPs)
- swelling, tenderness, fever, malaise, weakness
- nodules anywhere
- improves with pregnancy then flares after
- C1-C2 articulation can affect surgery
- swan-neck; boutonniere deformity; hammer toes
- Felty’s syndrome: RA, splenomegaly, neutropenia
- tests
- Rheumatoid factor
- anti-CCP (anti-cyclic citrulinated peptide antibody)
- Tx
- lifelong - no cure, just management/remission
- NSAIDs, low-dose prednisone, steroid injections
- disease modifying antirheumatic drugs (target inflammation/antibodies)
- Sulfasalazine, hydryoxychloroquine
- Methotrexate/Leflunamide
- Cyclophosphamide
- anti-TNF drugs
- inflixamab, entanercept
- adalimumab, golimamab
- surgery - joint replacement

RA scoring system

4 phases of fracture healing
- cellular callus
- mesenchymoid cell proliferation
- mineralized callus
- collagen to cartilage
- bony callus
- lamellar bone replaces mineralized callus
- remodeling

fracture complications
- acute respiratory distress syndrome (ARDS)
- fat embolism to lungs
- atelectasis (partial or complete collapse of lung)
- DVT, PE
- compartment syndrome (5 P’s)
- nerve/blood vessel injury
- failure of normal healing
5 P’s of compartment syndrome
- pain out of proportion
- paresthesia
- pallor
- paralysis
- pulselessness
fracture description

- bone side and name, position
- proximal, mid, distal
- line: transverse, spiral, oblique
- type of fracture
- open (no skin break) / closed (bone protruding)
- complete / incomplete
- greenstick, buckle (Torus) - “squished can”
- simple / comminuted (w/ or w/out butterfly fragment)
- angulation (bent- change in anatomical position)
- direction apex is pointing, location of distal fragment
- ex.: angulated 45 deg apex dorsal
- displacement (distance apart)
- anterior, posterior, lateral, medial
- 100% = no contact at fracture site
- other:
- distraction- amount of separation
- shortening- overriding, impacted
- # of pieces
- fragments
- joint disruption- intra-articular
- % subluxation- dislocation laterally, medially…
Mechanism, Presentation, Dx, Tx

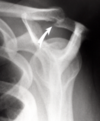
clavical fracture
- mechanism
- direct blow, fall on outstretched arm
- presentation
- pain, deformity, grinding at fx site, sagging shoulder
- CHECK SKIN for necrosis
- tx
- based on displacement
- conservative
- immobilize: sling, brace 4-6w
- surgery
- ORIF: open reduction w/ internal fixation
- IM nail (intermedulary)
Mechanism, Presentation, Dx, Tx
*what nerve affected

proximal humerus fracture
(axillary nerve)
- high energy injury: fall, MVA
- Neer classification: 2, 3, 4-part (head, shaft, greater/lesser tuberosity)
- tx
- conservative: sling 6w, passive ROM after 3w
- surgery
- ORIF
- hemiarthroplasty
- ORIF
Mechanism, Presentation, Dx, Tx
*what nerve affected

humeral shaft fracture
(radial nerve)
- mechanism: trauma, fall
- tx
- varies by severity
- malunion common
Mechanism, Presentation, Dx, Tx
*artery injury to watch

supracondylar fracture
(brachial artery)
- mechanism: fall w/ elbow extended
- tx
- surgery
Mechanism, Presentation, Dx, Tx

epicondyle/condylar fractures
(medial/lateral condyle)
- mechanism
- fall on outstreatched arm (valgus/varus force)
- tx
- conservative
- rest, splint, delayed, ROM
- surgical
- percutaneous pinning
- ORIF
- conservative
Mechanism, Presentation, Dx, Tx

radial head/neck fracture
- mechanism
- fall w/ elbow extended
- most common elbow fx in adults
- tx
- long arm splint 2-3w (must go beyond wrist)
- rarely surgery
- DO NOT immobilize too long
- PT
Mechanism, Presentation, Dx, Tx

olecranon fracture
- mechanism
- fall onto posterior elbow
- active tricep avulsion
- tx
- displacement & triceps guide treatment
Mechanism, Presentation, Dx, Tx

MUGR “gruesome murder”
- Galeazzi
- radial fracture w/ distal radioulnar joint dislocation
- fall on outstreatched arm w/ elbow flexed
- surgical fixation
- Monteggia
- ulnar fracture w/ radial head dislocation
- fall on outstretched arm
- surgery
Mechanism, Presentation, Dx, Tx

radial shaft fracture
- mechanism
- high energy injury, MVA
- usually w/ ulnar fracture/dislocation
- tx
- surgery
Mechanism, Presentation, Dx, Tx

ulnar shaft fracture
- mechanism
- usually direct blow
- tx
- spint
- rarely surgery
Mechanism, Presentation, Dx, Tx

distal radius fracture
- mechanism
- Colles: low energy FOOSH
- Smith: fall on flexed wristh (reverse Colles)
- most common fx of upper extremity
- presentation
- deformity, swelling, ecchymosis
- tenderness over fracture site
- tx
- buckle/minimal displacement - immobilize
- colles/smith/angulation/displacement - reduction or surgery (6w: 2 splint, 4 cast)
Mechanism, Presentation, Dx, Tx

chauffeur fracture (radial styloid fracture)
- mechanism
- direct blow to back of wrist
- forced ulnar deviation and supination
- tx
- surgery
Mechanism, Presentation, Dx, Tx

scaphoid fracture
- mechanism
- FOOSH
- often misdiagnosed as sprain
- “snuff box pain”
- most common carpal fx
- tx
- when in doubt- tx as fx: thumb SPICA splint
- splint 12w
- surgery rarely
Mechanism, Presentation, Dx, Tx

metacarpal fracture - boxer’s fracture
- mechanism
- hitting object with closed fist
- neck, shaft, or base fx
- 5th metacarpal neck most common
- presentation
- pain, swelling, rotational deformity, depressed knuckle
- CHECK for open wounds
- tx
- acceptable angulation: 10-20-30-40 rule from 1st digit
- rotational deformity NOT acceptable
- conservative
- ulnar gutter splint/cast
- 4-6w immobilization
- referral
- unstable fractures/rotational deformity
- closed reduction vs. surgeryd
1st metacarpal fractures

fracture at base of 1st metacarpal
- types:
-
Bennett fracture: intra-articular avulsion fx - CMC joint
- sublux/dislocation
-
Rolando fracture: “Y” or “T” shaped comminuted, intra-articular fx
- same mechanism, less commom
-
Bennett fracture: intra-articular avulsion fx - CMC joint
failures of healing
- malunion
- incomplete or faulty healing that affects function
- delayed union
- slower than normal healing
- non-union
- lack of bony reconstituion - bone remains at callus stage
Mechanism, Presentation, Dx, Tx

phalange fractures
- mechanism
- most common MSK injury
- presentation
- pain, swelling, deformity
- CHECK open wounds, nail bed injury - ortho referral
- tx
- budding taping
- surgery: angulation, displacement, open fracture
- complications:
- loss of motion, malunion, nonunion
Mechanism, Presentation, Dx, Tx

pelvic fracture
- mechanism
- high energy, MVAs
- presentation
- check for GU injuries: bladder, prostate
- fall - unable to bear weight
- leg shortened and externally rotated
- tx
- stabilize
- most need surgery
3 hip fracture types

- femoral neck
- types:
- subcapital, transcervical, basicervical
- intracapsular
- blood flow to femoral head disrupted
- tx
- femoral neck w/ no/minimal displacement - pinning
- w/ displacement - arthroplasty (replacement)
- types:
- intertrochanteric
- tx
- intramedullary nail/gamma nail
- dynamic hip screw (DHS)
- tx
- subtrochanteric
- tx: screws
Mechanism, Presentation, Dx, Tx

femur shaft fracture
- mechanism
- high energy, MVA
- tx
- nonsurgical
- non-displaced or multiple comorbidities
- surgical
- displaced/unstable
- nonsurgical
Mechanism, Presentation, Dx, Tx

supracondylar fracture
- mechanism
- load to flexed knee
- presentation
- assess popliteal artery, ACL
- pain, swelling, inability to flex/extend knee, +/- deformity
- tx
- conservative vs. surgical
Mechanism, Presentation, Dx, Tx

tibial plateau fracture
- mechanism
- extreme load or fall
- 60% lateral
- tx
- non-operative
- nwb w/ close follow-up
- surgery
- cannulated screw fixation or plate/screw, NWB
- non-operative
Mechanism, Presentation, Dx, Tx

patella fracture
- mechanism
- direct trauma
- forceful quadriceps contraction
- presentation
- deformity, swelling, can’t SLR
- tx
- non-operative:
- nwb 6w, gradually increase PROM
- surgery if displacement >3mm
- non-operative:
Mechanism, Presentation, Dx, Tx

tibial shaft fracture
- mechanism
- high energy, often open, twisting mechanism
- most common long bone fracture
- presentation
- pain, deformity, wounds, fracture blisters
- compartment syndrome - 5 P’s, fasciotomy
- assess n/v status
- tx
- conservative - LLC w/ progressive weight bearing
- surgical
- unstable, open fracture
- presentation after reduction
- IM nail
Mechanism, Presentation, Dx, Tx

Maisonneuve fracture
- mechanism
- eversion injury - Mortise widening
- proximal 1/3 fibula fracture
- w/ fibular neck - think peroneal nerve palsy
- tx
- surgery
- ORIF
- surgery
Mechanism, Presentation, Dx, Tx

ankle fracture
- mechanism
- twisting (inversion/eversion), MVA
- most common bone + joint injury
- smoking and habitus
- presentation
- pain, swelling, deformity, inability to ambulate
- tx
- conservative
- avulsion: treat like ankle sprain
- posterior splint vs. walking cast vs. walking boot
- surgical
- if any mortise widening/suspicion
- conservative

Mechanism, Presentation, Dx, Tx

medial malleolus fracture
- mechanism
- usually high impact: MVA, fall, tackled
- considerations:
- displacement (<2mm in joint acceptable)
- joint involvement (<25% joint surface acceptable)
- tenderness elsewhere
- tx
- referral
- non-operative
- nwb short leg splint vs. wbat short leg cast
Dx, Tx

bi/tri-malleolar frature
- unstable, refer for surgery
3 types 5th metatarsal fractures
Stress, Jones, Avulsion
- mechanism
- IMPORTANT: sudden vs. aching over time
- inversion - Jones
- eversion - other fracture
- tx
- stress - nwb cast 6-8w
- Jones - surgery vs. short-leg walking cast vs nwb cast 6-8
- avulsion - most common, short-leg walking cast/boot 4-6

Mechanism, Presentation, Dx, Tx

stress fractures
- mechanism
- overuse
- presentation
- insidious pain that progressively gets worse
- MRI for inflammatory stress
- tx
- eliminate the stress - REST
- nwb 6-12w, immobilize, PT, pain control
Physeal Fractures Typing
(pediatric/growth plate)
SALTER
- Type I: S- straight across
- Type II: A- above
- Type III: L- lower
- Type IV: T- through/transverse
- Type V: R- ruined (cRushed)

metacarpal fracture complications
- loss of grip strength
- residual dorsal deformity
- loss of knuckle prominence
Mechanism, Presentation, Dx, Tx
(fibula fracture - no pic)
fibula fracture
- mechanism
- direct blow, inversion/eversion injury
- presentation
- limping or uable to bear weight due to pain, edema, ecchymosis
- tx
- non-weightbearing
- dependent on location, ankle stability
4 Spondyloarthopathies
share predisposing factors and clinical features
- ankylosing spondylitis
- reactive athritis
- psoriatric arthritis
- enteropathic arthritis
Spondylarthropathies Common Features and Tx
- spine/joint pain
- chronic inflammation -> new bone formation (joint ankyloses)
- asymetrical peripheral arthritis
- ocular inflammation (acute anterior uveitis
- HLA-B27 gene
- sacroiliitis in imaging
- Tx
- pt education
- exercise
- NSAIDs, corticosteroids, sulfasalazine, methotrexate, anti-TNF therapy

- most common axial skeleton inflammatory disease
- white males 15-40
- LBP >3m: SI joint +/- buttocks
- early morning stiffness, fatigue
- asymmetrical polyarthritis
- entesitis: achilles tendinitis and/or heel pain
- ocular involvement
PE, tests, Tx

Ankylosing Spondylitis
- PE
- stooped posture (advanced)
- chest expansion
- tests
- Schober test - measure points on back (lumbar mobility)
- +/- FABER test (for SI joint)
- RF/ANA negative
- HLA-B27
- x-rays: “bamboo spine”
- MRI: inflammatory changes
- develops 1-3w after systemic infection (but aseptic)
- GI (salmonella, ersinia, shigella), GU (chlamydia)
- LE asymmetrical polyarthritis
- malaise, fever, fatigue
- enthesitis: achilles tendon or plantar fasciitis
- dactylitis: suasage fingers
-
Reiter’s syndrome
- conjuntivitis, urethritis/cervicitis, arthiritis (“can’t see, can’t pee, can’t climb a tree”)
PE, tests, Tx

Reactive Arthritis
- PE
- mucocutaneous lesions
- papulosquamous eruptions on palms and soles
- diarrhea
- tests
- x-rays, MRI
- HLA-B27
- synovial fluid analysis to dx septic vs. aseptic
- Tx
- NO CURE - self limited
- NSAIDs
- +/- intra-articular injection
- papulosquamous disease w/ kertinocyte proliferation
- asymmetric polyarthritis in large and small joints w/ dactylitis
- DIP joints w/ nail dystrophy (pitting, oil drop stains)
PE, tests, Tx
Psoriatric Arthritis
- PE
- spondylitis - inflammation of vertabrae
- mimics RA but no nodules or RF
- tests
- x-rays
- Tx
- pain control
- anti-TNF
- nonerosive, assymtrical polyarthritis - large joints
- pt has Crohn’s or ulcerative colitis
- inflammation of joints follow GI inflammation
PE, tests, Tx
Enteropathic Arthritis
- PE
- lower extremeties- peripheral arthritis not assoc. w/ HLA-B27
- spondylitis/sacroiliitis- assoc. w/ HLA-B27
- tests
- HLA-B27
- Tx
- control GI -> controlled joint inflammation
autoimmune connective disease - thickening of skin/connetive tissue
3 cardinal processes
Scleroderma (systemic sclerosis)
- autoimmunity and inflammation
- vascular injury and obliteration
- capillary loss
- fibrosis and matrix deposition
- deposition of connective tissue matrix
3 Classifications of Scleroderma
- Systemic
- Diffuse
- all over, rapid progression
- swelling, erythema, pruritis, fatigue, stiffnesss, malaise, Raynaud later
- early pulmonary fibrosis and acute renal failure
- Limited
- peripheral (spares trunk)
- CREST
- Calcinosis cutis
- Raynaud’s:
- primary cause: cold/stress = episodic vasoconstriction
- secondary: disease, B-blockers, chemotherapy
- Esophageal dysmotility (thickening)
- Sclerdactyly
- Telangiectasia
- Diffuse
- Mixed Connective Tissue Disorder
- overlap of SLE, scleroderma, myositis
- Raynaud w/ hand edema, renal crisis later
- autoantibody against U1-RNP
- Localized
- more common in children
- Morphea - reddish/purple lesion of skin
- skin induration (hardening) spares digits, common on LE
- NO Raynaud, NO systemic involvement
Scleroderma Organ Involvement
- skin
- thickening, symmetrical/bilateral, starts @ fingers and works proximal, masklike facies, hyperpigmentation/vitiligo in dark skinned, calcium deposits
- GI tract
- periodontal disease; GERD; stomach-gastroparesis; small intestine-impaired mobility, malabsorption; colon-constipation, rectal prolapse
- lungs
- honeycomb x-ray; RF: AA, male, difuse skin, severe GERD, topoisomerase-I antibodies
- pulmonary HTN; RF: limited cutaneous, late disease onset, many telangiectasias, anticentromere autoantibodies
- kidneys
- life threatening; CKD; RF: AA, tendon rubs, RNA plymerase I & II autoantibodies
- cardiac
- diffuse disease; tachychardia; conduction abnormalities; regurgitation; diastolic HF; pericardial effusion
- MSK
- CTS; decreased joint mobility; tendon friction rubs (rupture)
- other
- dry eyes/mouth; hypothyroid; CNS spared
Scleroderma Tests, Dx, Tx
- tests
- labs
- CBC /w diff - anemia
- Sed rate/CRP/RA normal
- Vit deficiencies: folate, B12, D
- nailfold capillaroscopy
- labs
- Dx
- skin induration, Raynaud’s, organ manifestations
- Tx
- No known regime to alter course
- immunosuppressants
- corticosteroids (sparingly in low doses)
- cyclophosphamide (slow lung disease)
- methotrexate (for skin manifestations)
- antifibrotic therapy
- D-penicillamine (prev. new organ involvement, improved survival)
- ACE inhibitors (for renal crisis)
- treat specific organ complications
Cells of Bone Remodeling
- osteoblasts - build
- osteoclasts - break down
- ostecytes - mature cells
- secrete and calcifies bone matrix material
- regulate bone reabsorption and formation
- release cytokines
- osteoprotogerin (OPG)
- receptor activator of nuclear factor kB ligand (RNAKL)
- regulate osteoclast production and rate of bone reabsorption
amount of bone acquired by modeling and remodeling / peak times
bone mineral density (BMD)
- peak bone mass
- 18-20 - proximal femur
- 25-30 - spine
- more loss than formation after this
bone physiology vs. pathology

primary / secondary causes of osteoporosis
- primary (idiopathic)
- juvenile (8-14 y/o)
- Stage I
- post-menopausal women (51-75)
- trabecular bone loss
- common fx: vertebral body, distal forearm
- Stage II (senile)
- men and women 70+
- trabecular and cortical bone loss
- common fx: wrist, vertebra, hip
- secondary
- men > women
- environmental factors
- nutrition, Ca/Vit D deficiency, inactivity, meds (PPI, chemo), tobacco, alcohol, caffeine, trauma
- disease
- RA, cushings, DM, hyperthyroid
Who to DEXA Scan
DEXA - bone density scan
- 70+ y/o
- 50-70 postmenopausal
- 50-59 w/ wrist fracture
- 70’s w/ vertebral fracture
- 50+ w/ hip fracture
Osteoporosis S/s, PE, tests, workup
- S/s
- NO s/s - must screen at risk
- PE
- measure height loss: >4cm since young adult max suggests vertebral fx
- BMI
- kyphosis: Dowager hump (wedge shaped compression fx)
- +/- spinal TTP and percussion
- tests
- FRAX - fracture risk assessment tool: demographics, prev fx, parent fx, smoking, glucocorticoids, RA, alcohol, DEXA BMD #
- workup
- labs to assess secondary causes
- x-rays to check for fractures
-
duel energy x-ray absorptiometry (DEXA) for bone mineral density
- T-score: value of control peak BMD
- within 1 SD = normal
- -1.0 to -2.5 SD = osteopenia
- -2.5 SD and below = osteoporosis
- -2.5 and below + fragility fx = severe/established osteoporosis
- Z-score: value of age/sex match
- -2.0 and above = normal
- -2.0 and below = below expected
- Repeat testing
- normal - mild osteopenia: 10-15y
- moderate osteopenia: 3-5y
- advanced osteopenia: annually
- undergoing tx: annual to monitor response
- Not recommended
- premenopausal, men < 70, women < 65 w/out risk factors
- T-score: value of control peak BMD
Other Osteoporosis Screening Tests
- QCT-quantitiative CT (spine)
- pQCT (wrist and tibia)
- Finger DXA
- US of calcaneous or wrist
- 3D CT of bone biopsy microarchitecture
- softening of bone - decreased mineralization between calcified bone and osteoid
- rickets - defective mineralization of cartilage in epiphyseal growth plate
PE, tests, Tx

osteomalacia
- PE
- asymtomatic
- deformity over time
- muscle weakness
- fracture
- antalgic gait/difficulty ambulating
- tests
- Chvostek’s sign: tap on facial nerve elicits twitch
- labs for underlying disorders: CMP, LFT, calcium, Vit D
- x-rays
- bone biopsy
- Tx
- Vit D replacement (>18 6,000 IU qd or 50,000 qw x 8w, 1500-2000 qd maint.)
- patient education: dietary changes, fall risk
-
localized bone remodeling disorder:
- lytic phase: excessive reabsorption (osteoclasts)
- mixed phase: then increased bone formation of weaker, disorganized bony structure (osteoclast and osteoblast)
- sclerotic phase: disorganized bone becomes vascular, fibrous connective tissue
PE, tests, Tx

Paget Disease
- PE
- asymptomatic or specific bone pain
- increased hat size, hearing loss, tinitis (if skull)
- deformities: bowing, kyphosis, abnormal gait
- tests
- x-rays, +/- bone scan, No MRI/CT
- labs
- alkaline phosphatase (bone specific) - high sensitivity for diagnosis
- NOT a calcium/Vit D issue (osteoclast problem)
- urine: hydroxyproline, dexypyridinoline, C-telopeptide
- Tx
- goal: control activity, treat complications
- Bisphosphonates
- Zoledronate acid (Reclast) 5mg IV
- Alendronate (Fosamax) 40mg x 6m
- Risedronate (Actonel) 30mg qd x 2m
- neoplasm - refer for amputation, chemo
- joint disease (OA or fracture) - replacement/ORIF
Osteoporosis Treatment
- supplemental calcium (1000/1200 W>50 & M>70) and vitamin D (600/800 W/M>70)
- Bisphosphonates
- inhibit osteoclasts to decrease turnover and bone loss
- oral
- Alendronate (Fosamax)
- Alendronate/cholecalciferol (Fosamax + D)
- Risedronate (Actonel)
- Iandronate (Boniva)
- Parenteral
- Zoledronic acid (Reclast)
- Ibandronate (Boniva)
- Expensive:
- Selective Estrogen REceptor Modulators (SERMs)
- decrease cytokines that activate osteopblasts - vertebral fx only
- Raloxifene (Evista) 60mg po qd
- Recombinant human parathyroid hormone
- Teriparatide (Forteo) 20mcg SQ qd (thigh or abdominal wall)
- high risk vertebral fractures, stimulates bone formation, no more than 2y, black box: osteosarcoma
- Human monoclonal antibody
- Denosumab (Prolia) 60mg SQ q6m
- Abx to RANKLE - inhibits osteoclast formation/activity
- Selective Estrogen REceptor Modulators (SERMs)
- Calcitrol
- nasal spray, inhibits osteoclasts
- Estrogen/progestin
- decreases bone turnover/loss
- Fracture treatment (total hip, hemiarthroplasty, vertebroplasty, kyphoplasty)
Bone Lesion Abbreviations
ABC, CMF, EG, GCT, FD, NOF, SBC
- ABC - aneurysmal bone cyst
- CMF - chondromyxoid fibroma
- EG - eosinophilic granuloma
- GCT - giant cell tumor
- FD - fibrous dysplasia
- NOF - non ossifying fibroma
- SBC - simple bone cyst
Benign vs. Malignant Lesions
benign types
benign typically have well defined borders
- bone forming (osteo-)
- osteoid osteoma, osteoblastoma, osteoma
- cartilage forming (chondro-)
- chondroma, osteochondroma, chondroblastoma
- fibrous bone lesions (fibro-)
- fibrous dysplasia, nonossifying fibroma
- radiolucent bone lesions
- giant cell tumor, unicameral bone cyst, aneurysmal bone cyst

- most common benign osteoid tumor
- most common in long bones - proximal femur
- most common in 2nd decade of life (10-30 y/o)
- night pain
- pain relieved w/ NSAIDs
tests, Tx
osteoid osteoma
- tests
- <1cm lytic nidus w/ surrounding sclerosis
- HOT on bone scan, use CT to localize
- “cherry red” nidus histology
- Tx
- NSAIDs for pain
- curettage/burring
- radiofrequency ablation
- dnew bone depositied on skull, tibia, femur
- 2nd to 4th decade
- associated w/ Gardner’s syndrome
- colonic polyps, desmoid tumors
PE, tests, Tx

osteoma
- PE
- firm mass w/ little to no pain
- tests
- xray: dense cortical bone, not contiguous w/ intramedullary canal
- Tx
- observation vs. marginal resection
- larger osteoid tumor (>2cm and more aggressive)
- 1st to 3rd decades
- posterior spine, long bones (femur, tibia)
- night pain
- pain w/ activity NOT responsive to NSAIDs
tests, Tx
osteoblastoma
- tests
- x-ray: no sclerotic rim, NO nidus
- Tx
- biopsy
- surgical
- curettage and bone grafting
- tumor excision w/ bone reconstruction vs internal fixation
- exostosis - bony projection on surface of bone covered with cartilage
- most common benign bone tumor
- solitary or multiple (Multiple Hereditary Exostoses)
- femur (at knee), tibia, humerus
PE, tests, Tx

osteochondroma
- PE
- often asymptomatic
- pain or painful mass
- away from growth plate
- tests
- xrays
- Tx
- asymptomatic
- monitor
- symptomatic
- surgical excision
- asymptomatic
- tumor of hyaline cartilage within medullary canal
- <5cm
- associated w/
- Ollier’s disease
- Maffucci’s syndrome
PE, tests, Tx
enchondroma
- PE
- asymptomatic - usually incidental finding
- pain w/ pathologic fracture
- tests
- plain films: stippled calcification
- Tx
- no tx if asymptomatic
- symptoms
- biopsy
- currettage w/ bone grafting
- tumor of hyaline cartilage on surface of bone
- usually metaphyseal (near tendon/ligament attachment)
PE, tests, Tx
periosteal chondroma
- PE
- painful, sometimes palpable mass
- tests
- xray: saucerization w/ sclerosis
- Tx
- excision
- need to r/o chondrosarcoma
- abnormal tissue formation in place of lamellar bone
- more common in femur
PE, tests, Tx

fibrous dysplasia
- PE
- pain
- tests
- xray: ground glass appearance
- Tx
- Bisphosphonates
- surgical management
- rigid fixation
- fluid filled cystic tumor w/ fibrous lining
- near physis and grows distally
- age 5-15 y/o
PE, tests, Tx

unicameral bone cyst
- PE
- incidental finding -or-
- mild pain, swelling, stiffness in joint
- sudding pain d/t pathologic fracture
- tests
- xray
- Tx
- r/o sarcoma!
- intralesional aspiration and corticosteroid injection
- surgery
- curettage w/ bone grafting
- aggressive vascular lesion w/ cystic blood filled cavities
- less frequent than GCT
- locally destructive
- d/t secondary lesion
tests, Tx
aneurysmal bone cyst
- tests
- MRI (instead of CT) to image fluid levels
- Tx
- surgery
- curettage and bone grafting
- surgery

- most common malignant bone tumor
- common w/ other carcinomas:
- breast/prostate, lung, kidney, GI tract, thyroid

metastatic disease
- proliferation of interosseus plasma cells
- found in bone marrow
- more common in AA, men, 50+
PE, tests, Tx

multiple myeloma
- PE
- bone pain, pathologic fractures, weakness/malaise
- neuro complaints - spinal cord compression
- tests
- plain films
- Tx
- surgical fixation of pathologic fractures
- chemotherapy
- radiation
- most common malignant bone tumor
- primitive mesenchymal bone forming cells produce malignant osteoid
- femur, tibia, humerus
- more common in 12-25 y/o
PE, tests, Tx

osteosarcoma
- PE
- variable: pain, swelling, night pain, no hx trauma
- palpable mass
- decreased ROM
- lymphandenopathy
- +/- respiratory mets
- primary (surface) vs. secondary (intramedulary) - variants
- tests
- labs: LDH, ALP, CBC w/ diff, CMP, urinalysis
- open biopsy
- plain xrays
- CXR to check for mets to lungs
- bone scan (evaluate metastatic disease)
- CT (location and staging)
- MRI (eval soft tissue involvement)
- Tx
- wide resection - limb sparing
- rotationplasty
- amputation
- chemo
- cartilage malignancy
- low grade/low mets - high grade/aggressive
PE, tests, Tx

chondrosarcoma
- PE
- pain over time
- night pain
- +/- mass
- symptoms near location of tumor
- arises from benign cartilage lesion (enchondroma, osteochondroma)
- pelvis, femur, humerus, ribs
tests

secondary chondrosarcoma
- tests
- plain films: scattered, irregular calcification
- endothelioma (internal surface) of bone
- associated w/ chromosomal translocation
- birth - 20’s
PE, tests, Tx

Ewing sarcoma
(boards question - know osteo vs. ewing sarcomas)
- PE
- progressively worse pain
- night pain
- localized swelling/mass
- increased warmth over area, fever, incr sed rate/WBCs, anemia, malaise (mimics infection)
- tests
- plain films: destructive lesion w/ poor border, periosteal bone formation
- MRI for soft tissue involvement
- CT scan for staging
- Tx
- dependent on location and size
- chemo/radiation
- surgery
- limb sparing vs. amputation (rare)
- dependent on location and size
- cartilage forming in epiphysis (d/t immature cartilage cell proliferation)
- ususally 2nd decade when growth plates open
PE, tests, Tx
chondroblasoma
- PE
- pain, tenderness, swelling, limp (if in LE)
- tests
- xray: well circumscribed/defined lytic lesion w/ surrounding sclerosis; +/- stippled calcification
- histology: “chickenwire calcification”
- Tx
- curettage (scrapping) and bone graft
- increased risk of osteoarthritis when joint involved
- proliferation of fibrous tissue
- fibrous cortical defect <1 cm affecting cortex only
- children/adolescents
- Jaffe-Campanacci syndrome - multiple NOFs and cafe au lait spots
PE, tests, Tx
nonossifying fibroma
- PE
- asymptomatic to painful
- test
- xray: geographic, thick sclerotic rim, well circumscribed
- Tx
- usually heals spontaneously by 20’s
- oberservation vs. surgical
- curettage and bone graft
- aggressive proliferation of benign multinucleated cells
- ages 20-50
- femur, tibia, radius
PE, tests, Tx
giant cell tumor
- PE
- pain, swelling, deformity w/ increasing size
- pathologic fractures
- can metastasize to lung
- tests
- xray: lucent, sometimes see bony destruction, can enter soft tissue
- Tx
- surgery
- curettage, ablation, bone grafting, fixation
- surgery
- chronic multisymptom inflammatory autoimmune disease - autoantibodies
- frequent relapses, permanent organ damage, women of childbearing age
epidemiology, hx, systems, tests, Tx
systemic lupus erythematosus (SLE)
- epidemiology
- unknown: genetics, environment (UV, drugs: procainamide, hydralazine, quinidine, isoniazid), viruses, diet (a.a.), hormonal
- Hx
- sunlight, hair loss, Raynaud’s, FH
- systems
- fever, malaise, wt loss; skin; MSK: pain, stiffness out of proportion, non-erosive; kidneys; CNS: seizures, psychosis; cardio; GI; hematologic: anemia, thrombocytopenia; ocular
- tests
- CBC w/ diff, CMP, ESR, CRP, PT, PTT, ANA, urinalysis
- anti-dsDNA
- anti-Smith
- anithistone (drug induced SLE)
- plain films to r/o other
- CXR, ECG, echocardiogram to eval other systems
- Tx
- conservative vs. medicinal based on severity
- counseling/lifestyle - smoking cessation, sun, fatigue, sleep
- PT/OT
- meds
- antimalarials: hydroxycholoroquine (Plaquenil)
- NSAIDs
- corticosteroids: Prednisone (not w/ NSAIDs)
- supplement CA+Vit D if long-term
- DMARDs (immunosuppressants)
- Methotrexate (Trexall)
- Azathioprine (Imuran)
- Cyclophosphamide
- Mycophenolate
- autoimmune disorder affecting exocrine glands
- salivary and lacrimal glands
- bilateral parotid gland swelling
- women 40-60
- primary
- SICCA symptoms
- keratoconjunctivitis
-
xerostomia
- mouth infections: dental carries, difficulty swallowing, pain, hoarseness, parotitis
- SICCA symptoms
- secondary
- associated w/ SLE, RA, scleroderma
etiology, systems, tests, Tx
Sjorgren’s Syndrome
- etiology
- unknown: genetics, environment: viruses, hormones
- systems
- fatigue, fever; skin; pulmonary; MSK; renal; neuro: neuropathy, myelopathy; neoplasia: lymphandenopathy
- tests
- ocular/oral exams
- Schirmer test (strip from eye)
- Rose Bengal staining
- labs: CBC w/ diff, CMP, +RF, +ANA, +ESR
- anti-Ro/SSA
- anti-La/SSB
- Tx
- no cure - treat symptoms/systems
- fluid replacement, skin lotion, humidifiers, eye & dental exams
- rheumatology referral
- non-erosive inflammatory affecting shoulders and pelvic girdle
- typically 50+
- sudden onset muscle pain and stiffness
- morning stiffness >45min
-
associated w/ giant cell arteritis (temporal arteritis)*
- extracranial blood vessels, can cause blindness
tests, Tx
Polymyalgia Rheumatica
- tests
- HLA-DR4
- ESR >40, CRP, CBC w/ dif, -RF, -antiCCP, CPK
- GCA (temporal artery biopsy) - gold standard
-
Tx
- Prednisone 12.5-25mg/d
- PPI to protect GI
- Ca+/Vit d
- giant cell arteritis
- Prednisone 40-60mg 4w then decrease 10mg q2w until at 20mg, then reduce by 2.5mg q2-4w to 10mg then decrease 1mg q1-2m as long as no relapse
- systemic vascular syndrome that obliterates small/medium vessels
- necrotizing inflammation occuring at bifurcations that weakens vessels (aneurysms, thrombi, hemorrhage, ischemia, infarction)
- men ages 40-60
etiology, systems, tests, Tx
Polyarteritis Nodosa
- etiology
- unknown: HBV/HCV, CECR1 gene mutation
- systems
- fever, fatigue, anorexia/weight loss, myalgia
- nervous system, cutaneous: Raynaud’s, rash, purpura, livido reticularis; GI, renal failure, testicular tenderness
- tests
- CBC w/ diff, CRP, ESR, liver function, HBV/HCV, -RF, -ANA
- biopsy skin
- abdominal CT for ischemic/affected organs
- Tx
- refer to rheumatologist
- meds:
- Prednisone 1-2mg/kg/d
- antivirals for HBV
- tx HTN
- humoral attack to muscle capillaries and small arterioles - capillary infarctions/destruction
- abnormal T-cell activity, genetic HLA types DR3/5/7, infections, drugs (statins, interferon, quinidine)
S/s, tests, Tx

Dermatomyositis
- S/s
- Gottron’s papules: raised scaly lesions on MCP, PIP, elbows, eyelids
- rash in V neck distribution
- arthralgias in knees, wrists, hands; fatigue, weight loss, fever; Raynaud’s; GI; pulmonary; cardiac
- proximal muscle weakness - standing climbing, walking, lifting
- tests
- CBC, ESR, CK, AST/LDH
- +ANA (non specific)
- anti-Mi2 & anti-MDA5 (specific)
- MRI, EMG
- muscle biopsy - definitive
- Tx
- non-med: high protein, exercise, consult system specialists
- skin: avoid UV, topical corticosteroids, hydroxychloroquine
- oral meds:
- corticosteroids - Prednisone 1mg/kg/d 4-8w; d/c when CK level normal
- Methotrexate 7.5mg po weekly, increase as needed; take w/ folic acid
- T-cell mediated cytotoxic process against muscle antigens
S/s, tests, Tx
Polymyositis
- S/s
- arthralgias in knees, wrists, hands; fatigue, weight loss, fever; Raynaud’s; GI; pulmonary; cardiac
- proximal muscle weakness - standing climbing, walking, lifting
- tests
- CBC, ESR, elevated CK, AST/LDH
- +ANA (non specific)
- anti-Jo-1 (specific)
- MRI, EMG
- muscle biopsy - definitive
- Tx
- non-med: high protein, exercise, consult system specialists
- skin: avoid UV, topical corticosteroids, hydroxychloroquine
- oral meds:
- corticosteroids - Prednisone 1mg/kg/d 4-8w; d/c when CK level normal
- Methotrexate 7.5mg po weekly, increase as needed; take w/ folic acid
- central sensitization - chronic widespread pain and tenderness
S/s, tests, Tx
Fibromyalgia
- S/s
- widespread pain and stiffness (neck, shoulder, low back, hips)
- fatigue, disordered sleep, cognitive function, depression, HA, IBS, TMJ, overactive bladder
- tests
- labs to r/o other diseases: CBC w/ diff, BMP, TSH, ESR, CRP, ANA, RF, CPK
- imaging for underlying pathology
- Tx
- focus on non-pharm: education, counseling, eliminate stressors, PT/OT
- meds (low dose, short term)
- acetaminophen, Tramadol 50mg q6-8h PRN
- muscle relaxers: Cyclobenzaprine (Flexeril) 5mg po q8h
- NO OPIOIDS
- anxiety and insomnia
- Alprazolam (Xanax)
- Zolpidem (Ambien)
- antidepressants
- Amitriptyline, Duloxetine (Cymbalta), Venlafaxine (Effexor)
- anticonvulsants for neuropathic pain
- Gabapentin (Neurontin), Pregabalin (Lyrica)
- pain, swelling, vasomotor dysfunction in extremeties following trauma or surgery
- soft tissue disorder, immobilization when pt should be getting better
S/s, tests, Tx

Complex Regional Pain Syndrome
- S/s
- pain out of proportion to event
- color changes
- skin dry, shiny, wrinkles w/ temp changes
- joint fibrosis: flexion contractures, frozen shoulder
- muscle weakness/tremors
- 3 stages: acute (3m), subacute (9m), chronic (1+y)
- tests
- no specific labs
- plain films for bone demineralization (DEXA scan)
- triple phase bone scan - increased uptake in articular structures
- Tx
- conservative
- education - screen for depression and suicide
- NSAIDs, corticosteroids
- sympathetic nerve block
- PT/OT
- surgical
- upper thoracic/lumbar sympathectomy
- chemical sympathectomy
- spinal cord stimulator implant
- conservative
- cognitive difficulties and skeletal muscle fatigue
- myalgic encephalomyelitis
S/s, tests, Tx
Chronic Fatigue Syndrome
- S/s
- sudden onset of abrupt, debilitating fatigue - impacts ADLs
- +/- flulike prodrome
- similar to fibromyalgia
- test
- r/o heart disease, thyroid, anemia, liver and renal disease, psych
- Tx
- supportive and symptomatic
- autosomal dominant connective tissue disorder
- multi-system: eye, skeleton, heart, aorta, lung, integument
S/s, tests, Tx
Marfan Syndrome
- S/s
- eye: lens displacement, retinal detachment; msk: ligament laxity, increased limb and finger length; mouth: arched palate, crowded detention; spontaneous pneumothorax; striae atrophy; cystic organs
- tests
- genetic testing
- opthalmic exam
- skeletal testing
- Tx
- education, tx of pathology
- heterogeneous disorder of connective tissue - affects structure, production or processing of collagen
- fragile tissues, joint hypermobility, skin hyperextensibility
S/s, tests, Tx

Ehlers-Danlos Syndrome
- S/s
- velvety skin/atrophy
- medium and large vessel rupture
- easily bruises
- organ rupture, premature rupture of fetal membranes
- Tx
- treat manifestations
- care w/ suturing
- B-blocker to protect vessels
- defects in bony matrix causes hereditary osteopenia
- blue sclera
S/s, tests, Tx

Osteogenesis Imperfecta
- S/s
- recurrent fx w/ bony deformity, impaired mobility
- short stature
- restrictive lung disease, compression of brain stem
- abnormal teeth
- blue sclera
- Tx
- fracture management
- Risedronate - increase bone mineral density


