MRCS Part B Applied surgical sciences and critical care Flashcards
What affects the accumulation of fluid in the interstitium? How does this fluid differ from plasma? What happens to excess fluid? How does oedema develop?
The formation of fluid in the interstitium is governed primarily by Starlings Forces (not the same as Starlings Law!). These consist of forces from the within the capillary; the capillary pressure itself and the plasma colloid oncotic pressure. This is counterbalanced by forces within the interstitium which comprise the interstitial fluid pressure and the interstitial fluid osmotic pressure. There is normally a balance between these forces so that most of the fluid that passes out of the capillary is subsequently re-absorbed. It has a similar electrolyte profile to plasma. However, protein is not usually present as their high molecular weight precludes their filtration. Excess fluid is usually returned to the vascular system via the lymphatic route. Oedema is characterised by an excessive quantity of fluid in the extracellular space. Factors which favour its development include: Increased hydrostatic pressure Hypoproteinaemia (lower plasma oncotic pressure) Venous/ lymphatic obstruction Endothelial changes in the capillary bed (for example in acute inflammation) Starlings forces: About one sixth of the body consists of spaces between cells. The fluid within these spaces is termed interstitial fluid. This fluid is formed by filtration and diffusion from capillaries. It contains almost the same constituents as plasma with the exception of proteins as these are not filtered due to their high relative molecular mass. The pressure in the capillaries tends to force fluid and its dissolved substances through capillary pores and into this space. In contrast the osmotic pressure exerted by plasma proteins (colloid osmostic pressure) tends to favor movement from the interstitial spaces back into the vascular compartments (capillaries) themselves. The lymphatic system returns back to the circulation the small amounts of protein that do leak into the interstitium. There are four primary forces that determine fluid movement through a capillary membrane (Starlings forces): Capillary pressure - forces fluid out of the capillary Interstitial fluid pressure- which tends to force fluid inwards through the capillary membrane (when it is positive) Plasma colloid osmotic pressure- favors influx into the capillary Interstitial fluid osmotic pressure- favors efflux from the capillary into the interstitum
How is the respiratory rhythm generated? What is the Hering-Breur reflex? What is the most important factor in controlling respiration? In what situations is this altered?
There are 2 groups of medullary neurones, the dorsal and ventral respiratory groups, that discharge action potentials with an intrinsic rhythm that corresponds to the respiratory cycle. These upper motor neurones have efferents to the diaphragm by way of the contralateral phrenic nerve.
These neurones receive inputs from higher centres in the CNS including the cerebral cortex and the pons. They also receive inputs from the aortic and carotid bodies. They also have a vagal input which is the sensory afferent from the lung itself. Inspiration is initiated from the dorsal respiratory group.
Hering-Breur reflex: When the lung is inflated, receptors send impulses to the dorsal respiratory neurones via the vagus. With high tidal volumes this serves to regulate inspiration. In humans, it is not generally activated until volumes exceed 800ml. It is therefore generally only active during exercise.
The most important factor controlling respiration is the partial pressure of carbon dioxide in the plasma. Within the CNS, carbon dioxide results in generation of hydrogen ions that stimulate central chemoreceptors. In the periphery, the receptors are located in the aortic and carotid bodies.
Patients with chronic lung disease may become less sensitive to changes in carbon dioxide levels and their respiratory drive is hypoxia driven. In this small group of people, administration of excessive oxygen may dampen the respiratory stimulus.
Control of ventilation:
- Coordinated by the respiratory centres, chemoreceptors, lung receptors and muscles.
- Automatic, involuntary control of respiration occurs from the medulla.
- The respiratory centres control the respiratory rate and the depth of respiration.
Respiratory centres
- Medullary respiratory centre: Inspiratory and expiratory neurones. Has ventral group which controls forced voluntary expiration and the dorsal group controls inspiration. Depressed by opiates.
- Apneustic centre: Lower pons. Stimulates inspiration - activates and prolongs inhalation. Overridden by pneumotaxic control to end inspiration.
- Pneumotaxic centre: Upper pons, inhibits inspiration at a certain point. Fine tunes the respiratory rate.
Ventillatory variables
- Levels of pCO2 most important in ventilation control
- Levels of O2 are less important.
- Peripheral chemoreceptors: located in the bifurcation of carotid arteries and arch of the aorta. They respond to changes in reduced pO2, increased H+ and increased pCO2 in ARTERIAL BLOOD.
- Central chemoreceptors: located in the medulla. Respond to increased H+ in BRAIN INTERSTITIAL FLUID to increase ventilation. NB the central receptors are NOT influenced by O2 levels.
Lung receptors include:
- Stretch receptors: respond to lung stretching causing a reduced respiratory rate
- Irritant receptors: respond to smoke etc causing bronchospasm
- J (juxtacapillary) receptors
What is meant by the term inotrope? How do they work? What is the difference between inotropes and vasoconstrictors? What haemodyanamic parameters need to be monitored to allow the use of inotropes? How are inotropes administered and why? What is the main functional difference between adrenaline and nor adrenaline when used therapeutically?
Inotropes are agents which affect the contractility of the myocardium. Both positive and negative inotropes are recognised. However, the former group are more clinically useful.
Many inotropes work by increasing intracellular calcium levels and thus contractility. Many, such as adrenaline, act via beta receptors and increase cellular cAMP levels with subsequent mobilisation of calcium. Some, such as dopexamine, act indirectly by increasing the level of endogenous noradrenaline by inhibition of its neuronal re-uptake.
Inotropes principally act centrally and predominantly on the myocardium. The commonly used catecholamine type agents achieve this through agonism of the beta 1 receptor. Vasoconstrictors such as nor adrenaline exert most of their effects peripherally via alpha receptor agonism. Intropes are predominantly used where there is depression of myocardial function, they increase cardiac output and often blood pressure and this in turn can improve myocardial perfusion. This dual action is important since chronotropic effects alone may worsen rather than improve myocardial ischaemia. Vasoconstrictors are mainly used where there is a peripheral problem such as leaky capillary beds and vasodilation such as may occur in sepsis. In clinical practice it is sometimes necessary to use a combination of drugs.
Generally, mean arterial pressure and the central venous pressure need to be known and monitored.
Inotropes are administered centrally this ensures that they enter a high flow system directly and allows for the most reliable dosing.
Adrenaline mainly works as a beta 1 receptor agonist and therefore most of its effects are cardiac. Noradrenaline is a predominantly an alpha receptor agonist and works peripherally.
Inotropes are a class of drugs which work primarily by increasing cardiac output. They should be distinguished from vasoconstrictor drugs which are used specifically when the primary problem is peripheral vasodilatation.
Catecholamine type agents are commonly used and work by increasing cAMP levels by adenylate cyclase stimulation. This in turn intracellular calcium ion mobilisation and thus the force of contraction. Adrenaline works as a beta adrenergic receptor agonist at lower doses and an alpha receptor agonist at higher doses. Dopamine causes dopamine receptor mediated renal and mesenteric vascular dilatation and beta 1 receptor agonism at higher doses. This results in increased cardiac output. Since both heart rate and blood pressure are raised, there is less overall myocardial ischaemia. Dobutamine is a predominantly beta 1 receptor agonist with weak beta 2 and alpha receptor agonist properties. Noradrenaline is a catecholamine type agent and predominantly acts as an alpha receptor agonist and serves as a peripheral vasoconstrictor.
Phosphodiesterase inhibitors such as milrinone act specifically on the cardiac phosphodiesterase and increase cardiac output.
- Adrenaline: α-1, α-2, β-1, β-2
- Noradrenaline: α-1,( α-2), (β-1), (β-2)
- Dobutamine: β-1, (β 2)
- Dopamine: (α-1), (α-2), (β-1), D-1,D-2
Minor receptor effects in brackets
Effects of receptor binding
α-1, α-2: vasoconstriction
β-1: increased cardiac contractility and HR
β-2: vasodilatation
D-1: renal and spleen vasodilatation
D-2: inhibits release of noradrenaline
What is meant by the term transplant? What type of transplant is a renal transplant from an unrelated donor? How do xenografts and autografts differ from an allograft? Can you name any examples of xenografts and autografts?
The transposition of tissue from one anatomical region to another.
It is an allograft. This refers to the transplant of an organ or tissue from one individual to another unrelated individual of the same species. If the donor was an identical twin then this would be termed an isograft. Xenografts are transplants from one species to another. Autografts are transplants from one site to another on the same individual.
A porcine heart valve is an example of a xenograft. The use of long saphenous vein as a conduit in coronary artery bypass grafting could be termed an autograft.
Transplantation of solid organs: A number of different organ and tissue transplants are now available. In many cases an allograft is performed, where an organ is transplanted from one individual to another. Allografts will elicit an immune response and this is one of the main reasons for organ rejection.
Graft rejection occurs because allografts have allelic differences at genes that code immunohistocompatability complex genes. The main antigens that give rise to rejection are:
ABO blood group
Human leucocyte antigens (HLA)
Minor histocompatability antigens
ABO Matching
ABO incompatibility will result in early organ rejection (hyperacute) because of pre existing antibodies to other groups. Group O donors can give organs to any type of ABO recipient whereas group AB donor can only donate to AB recipient.
HLA System: The four most important HLA alleles are:
HLA A
HLA B
HLA C
HLA DR
An ideal organ match would be one in which all 8 alleles are matched (remember 2 from each parent, four each = 8 alleles). Modern immunosuppressive regimes help to manage the potential rejection due to HLA mismatching. However, the greater the number of mismatches the worse the long term outcome will be. T lymphocytes will recognise antigens bound to HLA molecules and will then become activated. Clonal expansion then occurs with a response directed against that antigen.
The extent to which an organ needs to be accurately cross matched depends on the organ type. For example, the liver is less immunogenic than the kidney and thus HLA matching is not commonly undertaken.
Allograft: Transplant of tissue from genetically non identical donor from the same species - Solid organ transplant from non related donor
Isograft: Graft of tissue between two individuals who are genetically identical - Solid organ transplant in identical twins
Autograft: Transplantation of organs or tissues from one part of the body to another in the same individual - Skin graft
Xenograft: Tissue transplanted from another species - Porcine heart valve
What is meant by the term HLA and how is it relevant in renal transplantation?
The term HLA stands for human leucocyte antigen. It is encoded by a loci of genes the proteins of which are exposed on the cell surface and form the basis of the immune system. The proteins encoded by HLAs are those on the outer part of body cells that are (in effect) unique to that person. There are three major HLA (MHC class I) genes these are A, B and C. The three major MHC class II genes are HLA DP, DQ and DR. The immune system uses the HLAs to differentiate self cells and non-self cells. Any cell displaying that person’s HLA type belongs to that person and, therefore, is not an invader. Cells displaying non self HLA antigens are identified as foreign and thus become targets for the immune system. This is of major importance in renal transplantation as the rejection of the graft is directly linked to the number of HLA mismatches between donor and recipient.
Transplantation of solid organs: A number of different organ and tissue transplants are now available. In many cases an allograft is performed, where an organ is transplanted from one individual to another. Allografts will elicit an immune response and this is one of the main reasons for organ rejection.
Graft rejection occurs because allografts have allelic differences at genes that code immunohistocompatability complex genes. The main antigens that give rise to rejection are:
- ABO blood group
- Human leucocyte antigens (HLA)
- Minor histocompatability antigens
ABO Matching
ABO incompatibility will result in early organ rejection (hyperacute) because of pre existing antibodies to other groups. Group O donors can give organs to any type of ABO recipient whereas group AB donor can only donate to AB recipient.
HLA System: The four most important HLA alleles are:
- HLA A
- HLA B
- HLA C
- HLA DR
An ideal organ match would be one in which all 8 alleles are matched (remember 2 from each parent, four each = 8 alleles). Modern immunosuppressive regimes help to manage the potential rejection due to HLA mismatching. However, the greater the number of mismatches the worse the long term outcome will be. T lymphocytes will recognise antigens bound to HLA molecules and will then become activated. Clonal expansion then occurs with a response directed against that antigen.
The extent to which an organ needs to be accurately cross matched depends on the organ type. For example, the liver is less immunogenic than the kidney and thus HLA matching is not commonly undertaken.
- Allograft: Transplant of tissue from genetically non identical donor from the same species - Solid organ transplant from non related donor
- Isograft: Graft of tissue between two individuals who are genetically identical - Solid organ transplant in identical twins
- Autograft: Transplantation of organs or tissues from one part of the body to another in the same individual - Skin graft
- Xenograft: Tissue transplanted from another species - Porcine heart valve
Describe the key features demonstrated in the x-ray. Outline the processes by which a fracture usually heals. What features determine the rate of fracture union?

This image demonstrates a displaced, comminuted fracture of the humerus with callus formation.
Fracture healing typically follows four key stages. In the first stage, there is the formation of haematoma at the fracture site. Microvessels proliferate and enter the haematoma and granulation tissue forms. In the second stage, new woven bone is formed from the periosteum and forms a collar around the end of each bony fragment. Eventually, bridging callus is formed. As this processes proceeds, the fracture site becomes progressively more stable. In the third stage, the fracture site is reasonably inflexible and the cortical bone unites. In the final stage, the fracture site remodels along the lines of stress and Haversian systems are laid down.
Factors affecting Union:
- Site of fracture, cancellous bone unites faster than cortical bone
- The presence of contamination
- Degree of soft tissue loss or destruction
- Poor blood supply
- Loss of periosteum
- Degree of displacement
- Degree of comminution
- Persistent mobility of the fracture site due to inadequate immobilisation
- Co-morbidities, including age
The healing of uncomplicated fractures typically follows the processes outlined in the table below. The timing of these events, even in uncomplicated cases, is affected by the type of bone, degree of displacement and co-morbidities. Fractures involving cancellous bone typically unite rapidly and by six weeks, union is often sufficiently advanced to resist normal stresses. In contrast, fractures involving cortical bone, such as the tibia, are slower to unite and it is not uncommon for tibial fractures to take up to 16 weeks to unite, some femoral fractures may take up to 6 months.
- Stage I: Formation of fracture site haematoma. Angiogenesis. Formation of granulation type tissue. Deposition of mineral salts
- Stage II: Formation of sub periosteal bone. Bone formation in medullary cavity of the fracture. Eventual formation of bridging callus
- Stage III: Endosteal bone formation
- Ingrowth of callus from medually cavity into fibrous tissue at fracture site
- Stage IV: Occurs following union of cortical bone at fracture site. Remodelling occurs. Haversian systems are laid down along lines of stress. Osteoclasts remove bridging callus
Complications:
- Stage I: Poor blood supply or excessive mobility favors cartilage formation instead of callus
- Stage II: Displaced fractures inhibit bridging callus formation
- Stage III: These stages are slow even in the normal setting, if internal fixation is used, bridging callus is less likely to form and this can delay the onset of mechanical stability
- Stage IV: Remodelling is less effective at correcting rotational deformity and the overall process is less effective in the elderly and when factors are present that inhibit healing
What is the commonest malignant bone tumour?
The commonest malignant bone tumour is metastatic cancer from another primary site.
A common pitfall is to answer this question stating that osteosarcoma is the commonest malignant bone tumour
Clearly if the question is : “What is the commonest primary malignant bone tumour?”. Then the answer is osteosarcoma. Ensure you listen carefully to the examiner.
Giant cell tumour of bone
These lesions sit between benign and malignant. Most are benign. They are relatively rare. They consist of multinucleated giant cells (osteoclast like). Malignancy in these lesions is rare and is of the order of 2%. They account for 20% of benign bone tumours. The lesions may present as an enlarging mass, with pain or pathological fracture. On imaging, these lesions have an epiphyseal location and have a characteristic “soap bubble” appearance. They do not normally demonstrate sclerosis and have a sharply defined border. Histologically, they demonstrate multinucleated giant cells. Treatment is challenging since these lesions are locally aggressive and have a high rate of local recurrence following excision.
Malignant bone tumours
The commonest malignant bone tumour is bone metastasis from another solid organ malignancy. Metastatic lesions to bone are significantly more common than primary bone tumours which are extremely rare.
Osteosarcoma
This is the most common form of primary bone tumour. It typically affects males in their second decade. They typically present as a painful expanding mass affecting a long bone such as the femur, in close proximity to a joint. Imaging demonstrates a lesion with mixed sclerotic and lucent zones in the metaphysis bone formation within the tumour is often visible. All patients will be fully staged at presentation with CT, MRI and often PET scanning. There is a high rate of metastasis to the lungs and most patients will receive chemotherapy. Surgical excision is the main treatment.
Ewings sarcoma
Ewings sarcomas typically affect long bones and typically occurs during the first two decades of life. They are complex tumours and have overlap with primitive neuroectodermal tumours. They have a predilection for the lower extremity. They typically present as a painful swelling affecting a long bone. Inflammatory markers such as the ESR are sometimes raised and this is associated with a poorer prognosis. On plain films, the tumour shows evidence of bone destruction with a periosteal reaction (onion skin) appearance. As the condition progresses the periosteal findings can change as the tumour invades the periosteum. Treatment is with excisional surgery and chemotherapy.
Secondary malignant tumours of bone
Metastatic bone tumours may be described as blastic, lytic or mixed. Osteoblastic metastatic disease has the lowest risk of spontaneous fracture when compared to osteolytic lesions of a similar size.
Lesions affecting the peritrochanteric region are most prone to spontaneous fracture (because of loading forces at that site).
The factors are incorporated into the Mirel Scoring system to stratify the risk of spontaneous fracture for bone metastasis of varying types.
Which tumours classically metastasise to bone?
Breast
Lung
Thyroid
Renal
Prostate
Giant cell tumour of bone
These lesions sit between benign and malignant. Most are benign. They are relatively rare. They consist of multinucleated giant cells (osteoclast like). Malignancy in these lesions is rare and is of the order of 2%. They account for 20% of benign bone tumours. The lesions may present as an enlarging mass, with pain or pathological fracture. On imaging, these lesions have an epiphyseal location and have a characteristic “soap bubble” appearance. They do not normally demonstrate sclerosis and have a sharply defined border. Histologically, they demonstrate multinucleated giant cells. Treatment is challenging since these lesions are locally aggressive and have a high rate of local recurrence following excision.
Malignant bone tumours
The commonest malignant bone tumour is bone metastasis from another solid organ malignancy. Metastatic lesions to bone are significantly more common than primary bone tumours which are extremely rare.
Osteosarcoma
This is the most common form of primary bone tumour. It typically affects males in their second decade. They typically present as a painful expanding mass affecting a long bone such as the femur, in close proximity to a joint. Imaging demonstrates a lesion with mixed sclerotic and lucent zones in the metaphysis bone formation within the tumour is often visible. All patients will be fully staged at presentation with CT, MRI and often PET scanning. There is a high rate of metastasis to the lungs and most patients will receive chemotherapy. Surgical excision is the main treatment.
Ewings sarcoma
Ewings sarcomas typically affect long bones and typically occurs during the first two decades of life. They are complex tumours and have overlap with primitive neuroectodermal tumours. They have a predilection for the lower extremity. They typically present as a painful swelling affecting a long bone. Inflammatory markers such as the ESR are sometimes raised and this is associated with a poorer prognosis. On plain films, the tumour shows evidence of bone destruction with a periosteal reaction (onion skin) appearance. As the condition progresses the periosteal findings can change as the tumour invades the periosteum. Treatment is with excisional surgery and chemotherapy.
Secondary malignant tumours of bone
Metastatic bone tumours may be described as blastic, lytic or mixed. Osteoblastic metastatic disease has the lowest risk of spontaneous fracture when compared to osteolytic lesions of a similar size.
Lesions affecting the peritrochanteric region are most prone to spontaneous fracture (because of loading forces at that site).
The factors are incorporated into the Mirel Scoring system to stratify the risk of spontaneous fracture for bone metastasis of varying types.
Radiologically, how to the bony metastatic lesions of breast and prostate cancer differ? What is the functional relevance of this?
Most breast cancer metastasis are radiolucent, those of prostate cancer are sclerotic. Radiolucent lesions have a higher intrinsic risk of pathological fracture.
Giant cell tumour of bone
These lesions sit between benign and malignant. Most are benign. They are relatively rare. They consist of multinucleated giant cells (osteoclast like). Malignancy in these lesions is rare and is of the order of 2%. They account for 20% of benign bone tumours. The lesions may present as an enlarging mass, with pain or pathological fracture. On imaging, these lesions have an epiphyseal location and have a characteristic “soap bubble” appearance. They do not normally demonstrate sclerosis and have a sharply defined border. Histologically, they demonstrate multinucleated giant cells. Treatment is challenging since these lesions are locally aggressive and have a high rate of local recurrence following excision.
Malignant bone tumours
The commonest malignant bone tumour is bone metastasis from another solid organ malignancy. Metastatic lesions to bone are significantly more common than primary bone tumours which are extremely rare.
Osteosarcoma
This is the most common form of primary bone tumour. It typically affects males in their second decade. They typically present as a painful expanding mass affecting a long bone such as the femur, in close proximity to a joint. Imaging demonstrates a lesion with mixed sclerotic and lucent zones in the metaphysis bone formation within the tumour is often visible. All patients will be fully staged at presentation with CT, MRI and often PET scanning. There is a high rate of metastasis to the lungs and most patients will receive chemotherapy. Surgical excision is the main treatment.
Ewings sarcoma
Ewings sarcomas typically affect long bones and typically occurs during the first two decades of life. They are complex tumours and have overlap with primitive neuroectodermal tumours. They have a predilection for the lower extremity. They typically present as a painful swelling affecting a long bone. Inflammatory markers such as the ESR are sometimes raised and this is associated with a poorer prognosis. On plain films, the tumour shows evidence of bone destruction with a periosteal reaction (onion skin) appearance. As the condition progresses the periosteal findings can change as the tumour invades the periosteum. Treatment is with excisional surgery and chemotherapy.
Secondary malignant tumours of bone
Metastatic bone tumours may be described as blastic, lytic or mixed. Osteoblastic metastatic disease has the lowest risk of spontaneous fracture when compared to osteolytic lesions of a similar size.
Lesions affecting the peritrochanteric region are most prone to spontaneous fracture (because of loading forces at that site).
The factors are incorporated into the Mirel Scoring system to stratify the risk of spontaneous fracture for bone metastasis of varying types.
What is the commonest primary malignant tumour of bone? How are they diagnosed, staged and treated? What is the commonest benign bone tumour?
Osteosarcoma - commonest malignant bone primary
Diagnosis is made by a combination of imaging and biopsy. Imaging with plain films and CT scanning will usually characterise the lesion. Biopsy is carefully planned such that the biopsy tract can be subsequently resected. Staging is performed with PET/CT scanning of the chest. The lungs are a common site of disease extension and most patients are treated with a combination of chemotherapy and resectional surgery.
Osteochondroma are one of the commonest benign bone tumours. Osteochonroma is a common non familial developmental aberration with the majority of cases presenting in the first two decades of life. The lesion is thought to arise as a result of herniation of cartilage through the growth plate and this followed by endochondral ossification typically results in a cartilage capped bony protuberance. They are typically located on long bones, usually the distal end of the femur.
Giant cell tumour of bone
These lesions sit between benign and malignant. Most are benign. They are relatively rare. They consist of multinucleated giant cells (osteoclast like). Malignancy in these lesions is rare and is of the order of 2%. They account for 20% of benign bone tumours. The lesions may present as an enlarging mass, with pain or pathological fracture. On imaging, these lesions have an epiphyseal location and have a characteristic “soap bubble” appearance. They do not normally demonstrate sclerosis and have a sharply defined border. Histologically, they demonstrate multinucleated giant cells. Treatment is challenging since these lesions are locally aggressive and have a high rate of local recurrence following excision.
Malignant bone tumours
The commonest malignant bone tumour is bone metastasis from another solid organ malignancy. Metastatic lesions to bone are significantly more common than primary bone tumours which are extremely rare.
Osteosarcoma
This is the most common form of primary bone tumour. It typically affects males in their second decade. They typically present as a painful expanding mass affecting a long bone such as the femur, in close proximity to a joint. Imaging demonstrates a lesion with mixed sclerotic and lucent zones in the metaphysis bone formation within the tumour is often visible. All patients will be fully staged at presentation with CT, MRI and often PET scanning. There is a high rate of metastasis to the lungs and most patients will receive chemotherapy. Surgical excision is the main treatment.
Ewings sarcoma
Ewings sarcomas typically affect long bones and typically occurs during the first two decades of life. They are complex tumours and have overlap with primitive neuroectodermal tumours. They have a predilection for the lower extremity. They typically present as a painful swelling affecting a long bone. Inflammatory markers such as the ESR are sometimes raised and this is associated with a poorer prognosis. On plain films, the tumour shows evidence of bone destruction with a periosteal reaction (onion skin) appearance. As the condition progresses the periosteal findings can change as the tumour invades the periosteum. Treatment is with excisional surgery and chemotherapy.
Secondary malignant tumours of bone
Metastatic bone tumours may be described as blastic, lytic or mixed. Osteoblastic metastatic disease has the lowest risk of spontaneous fracture when compared to osteolytic lesions of a similar size.
Lesions affecting the peritrochanteric region are most prone to spontaneous fracture (because of loading forces at that site).
The factors are incorporated into the Mirel Scoring system to stratify the risk of spontaneous fracture for bone metastasis of varying types.

Is a pathological fracture purely a sign of a malignant bone tumour?
No, pathological fractures can complicate a number of bone disease including benign bone tumours and intrinsic disorders of the bone such as osteoporosis.
Giant cell tumour of bone
These lesions sit between benign and malignant. Most are benign. They are relatively rare. They consist of multinucleated giant cells (osteoclast like). Malignancy in these lesions is rare and is of the order of 2%. They account for 20% of benign bone tumours. The lesions may present as an enlarging mass, with pain or pathological fracture. On imaging, these lesions have an epiphyseal location and have a characteristic “soap bubble” appearance. They do not normally demonstrate sclerosis and have a sharply defined border. Histologically, they demonstrate multinucleated giant cells. Treatment is challenging since these lesions are locally aggressive and have a high rate of local recurrence following excision.
Malignant bone tumours
The commonest malignant bone tumour is bone metastasis from another solid organ malignancy. Metastatic lesions to bone are significantly more common than primary bone tumours which are extremely rare.
Osteosarcoma
This is the most common form of primary bone tumour. It typically affects males in their second decade. They typically present as a painful expanding mass affecting a long bone such as the femur, in close proximity to a joint. Imaging demonstrates a lesion with mixed sclerotic and lucent zones in the metaphysis bone formation within the tumour is often visible. All patients will be fully staged at presentation with CT, MRI and often PET scanning. There is a high rate of metastasis to the lungs and most patients will receive chemotherapy. Surgical excision is the main treatment.
Ewings sarcoma
Ewings sarcomas typically affect long bones and typically occurs during the first two decades of life. They are complex tumours and have overlap with primitive neuroectodermal tumours. They have a predilection for the lower extremity. They typically present as a painful swelling affecting a long bone. Inflammatory markers such as the ESR are sometimes raised and this is associated with a poorer prognosis. On plain films, the tumour shows evidence of bone destruction with a periosteal reaction (onion skin) appearance. As the condition progresses the periosteal findings can change as the tumour invades the periosteum. Treatment is with excisional surgery and chemotherapy.
Secondary malignant tumours of bone
Metastatic bone tumours may be described as blastic, lytic or mixed. Osteoblastic metastatic disease has the lowest risk of spontaneous fracture when compared to osteolytic lesions of a similar size.
Lesions affecting the peritrochanteric region are most prone to spontaneous fracture (because of loading forces at that site).
The factors are incorporated into the Mirel Scoring system to stratify the risk of spontaneous fracture for bone metastasis of varying types.

What is an osteoclastoma? What is a chondroma and what features would favor a benign over a malignant lesion?
Osteoclastoma: These are multinucleated giant cell tumours affecting the bone. They are locally aggressive lesions with a low metastatic potential. They have a classical soap bubble appearance on x-ray.
Chondromas a benign cartilaginous lesions and are also very common. These are most typically located in the hands and upper limbs and are rarely found within the axial skeleton, a fact that helps to distinguish these from their sarcomatous counterparts. They are located either within the medulla (endochondroma) or on the periosteal surface (juxtacortical chondroma).
Central location, rapid change in size and irregular borders are all clinical features that would raise the suspicion of sarcoma.
Benign bone tumours
These are relatively common and typically occur in the young. Most will cease growth once skeletal maturity is attained. A key aspect to managing benign bone tumours lies in the exclusion of a malignant bone tumour. Plain films, CT, MRI and sometimes a bone biopsy may be required.
- Osteoid osteoma: M>F
- Commonest between 10 and 25 years
- Severe pain that responds to NSAIDS
- Femur and tibia usually affected
- Lesion affects cortex and radiologically consists of a lucent centre surrounded by reactive sclerosis
- Usually smaller than 1cm
- Chondroma: Common benign tumour
- Endochondroma are central lesions that may cause cortical thinning
- Ecchondroma project beyond the cortex
- May cause pathological fracture
- Rarely found in large bones
- Osteochondroma: One of the commonest benign bone tumours
- Usually occurs on the surface of a metaphysis (usually femur, proximal humerus or tibia)
- Pedunculated lesion arising from metaphysis
- Long standing lesions
- Do not grow once skeletal maturity reached
- Bone cyst: Commonest in adolescent boys
- Occur in proximal femur and humerus
- May result in pathological fracture
- Does not affect growth plate
- On imaging appears as ovoid radiolucent area with surrounding cortical thinning
Giant cell tumour of bone
These lesions sit between benign and malignant. Most are benign. They are relatively rare. They consist of multinucleated giant cells (osteoclast like). Malignancy in these lesions is rare and is of the order of 2%. They account for 20% of benign bone tumours. The lesions may present as an enlarging mass, with pain or pathological fracture. On imaging, these lesions have an epiphyseal location and have a characteristic “soap bubble” appearance. They do not normally demonstrate sclerosis and have a sharply defined border. Histologically, they demonstrate multinucleated giant cells. Treatment is challenging since these lesions are locally aggressive and have a high rate of local recurrence following excision.
Malignant bone tumours
The commonest malignant bone tumour is bone metastasis from another solid organ malignancy. Metastatic lesions to bone are significantly more common than primary bone tumours which are extremely rare.
Osteosarcoma
This is the most common form of primary bone tumour. It typically affects males in their second decade. They typically present as a painful expanding mass affecting a long bone such as the femur, in close proximity to a joint. Imaging demonstrates a lesion with mixed sclerotic and lucent zones in the metaphysis bone formation within the tumour is often visible. All patients will be fully staged at presentation with CT, MRI and often PET scanning. There is a high rate of metastasis to the lungs and most patients will receive chemotherapy. Surgical excision is the main treatment.
Ewings sarcoma
Ewings sarcomas typically affect long bones and typically occurs during the first two decades of life. They are complex tumours and have overlap with primitive neuroectodermal tumours. They have a predilection for the lower extremity. They typically present as a painful swelling affecting a long bone. Inflammatory markers such as the ESR are sometimes raised and this is associated with a poorer prognosis. On plain films, the tumour shows evidence of bone destruction with a periosteal reaction (onion skin) appearance. As the condition progresses the periosteal findings can change as the tumour invades the periosteum. Treatment is with excisional surgery and chemotherapy.
Secondary malignant tumours of bone
Metastatic bone tumours may be described as blastic, lytic or mixed. Osteoblastic metastatic disease has the lowest risk of spontaneous fracture when compared to osteolytic lesions of a similar size.
Lesions affecting the peritrochanteric region are most prone to spontaneous fracture (because of loading forces at that site).
The factors are incorporated into the Mirel Scoring system to stratify the risk of spontaneous fracture for bone metastasis of varying types.
What is the commonest malignant colonic lesion? What is the commonest anatomical site for colonic cancers to develop? What are the commonest presenting symptoms of colorectal cancer? What diagnostic modalities are available to investigate the colon? Once colonic cancer is diagnosed, how is the patient staged?
Adenocarcinoma. Other rare lesions include melanomas, carcinoid tumours and in the distal anal canal squamous cell cancers. Up to 70% of colonic cancers occur in the sigmoid colon and upper rectum.
The commonest symptoms include change in bowel habit and rectal bleeding. Other symptoms include abdominal pain, weight loss and those related to anaemia resulting from chronic occult blood loss.
Investigations: Colonoscopy, CT colonoscopy, Barium enema, CT scanning with faecal tagging
Colonoscopy is the most sensitive and specific test.
All colonic cancers are staged with CT scanning of the chest, abdomen and pelvis. MRI scanning of the rectum is performed if the cancer lies below the peritoneal reflection.
Patients diagnosed as having colorectal cancer should be completely staged using CT of the chest/ abdomen and pelvis. Their entire colon should have been evaluated with colonoscopy or CT colonography. Patients whose tumours lie below the peritoneal reflection should have their mesorectum evaluated with MRI.
Once their staging is complete patients should be discussed within a dedicated colorectal MDT meeting and a treatment plan formulated.
Treatment of colonic cancer
Cancer of the colon is nearly always treated with surgery. Stents, surgical bypass and diversion stomas may all be used as palliative adjuncts. Resectional surgery is the only option for cure in patients with colon cancer. The procedure is tailored to the patient and the tumour location. The lymphatic drainage of the colon follows the arterial supply and therefore most resections are tailored around the resection of particular lymphatic chains (e.g. ileo-colic pedicle for right sided tumours). Some patients may have confounding factors that will govern the choice of procedure, for example a tumour in a patient from a HNPCC family may be better served with a panproctocolectomy rather than segmental resection. Following resection the decision has to be made regarding restoration of continuity. For an anastomosis to heal the key technical factors include; adequate blood supply, mucosal apposition and no tissue tension. Surrounding sepsis, unstable patients and inexperienced surgeons may compromise these key principles and in such circumstances it may be safer to construct an end stoma rather than attempting an anastomosis.
When a colonic cancer presents with an obstructing lesion; the options are to either stent it or resect. In modern practice it is unusual to simply defunction a colonic tumour with a proximal loop stoma. This differs from the situation in the rectum (see below).
Following resection patients with risk factors for disease recurrence are usually offered chemotherapy, a combination of 5FU and oxaliplatin is common.
Rectal cancer
The management of rectal cancer is slightly different to that of colonic cancer. This reflects the rectum’s anatomical location and the challenges posed as a result. Tumours located in the rectum can be surgically resected with either an anterior resection or an abdomino - perineal resection. The technical aspects governing the choice between these two procedures can be complex to appreciate and the main point to appreciate for the MRCS is that involvement of the sphincter complex or very low tumours require APER. In the rectum a 2cm distal clearance margin is required and this may also impact on the procedure chosen. In addition to excision of the rectal tube an integral part of the procedure is a meticulous dissection of the mesorectal fat and lymph nodes (total mesorectal excision/ TME). In rectal cancer surgery invovlement of the cirumferential resection margin carries a high risk of disease recurrence. Because the rectum is an extraperitoneal structure (until you remove it that is!) it is possible to irradiate it, something which cannot be offered for colonic tumours. This has a major impact in rectal cancer treatment and many patients will be offered neoadjuvent radiotherapy (both long and short course) prior to resectional surgery. Patients with T1, 2 and 3 /N0 disease on imaging do not require irradiation and should proceed straight to surgery. Patients with T4 disease will typically have long course chemo radiotherapy. Patients presenting with large bowel obstruction from rectal cancer should not undergo resectional surgery without staging as primary treatment (very different from colonic cancer). This is because rectal surgery is more technically demanding, the anastomotic leak rate is higher and the danger of a positive resection margin in an unstaged patient is high. Therefore patients with obstructing rectal cancer should have a defunctioning loop colostomy.
In the emergency setting, where the bowel has perforated, the risk of an anastomosis is much greater, particularly when the anastomosis is colon-colon. In this situation, an end colostomy is often safer and can be reversed later. When resection of the sigmoid colon is performed and an end colostomy is fashioned the operation is referred to as a Hartmans procedure. Whilst left sided resections are more risky, ileo-colic anastomoses are relatively safe even in the emergency setting and do not need to be defunctioned.

What is this investigation, what does it show and what is the treatment?

This is a double contrast barium enema. It demonstrates an “apple core” lesion of the ascending colon. This is most likely to represent a right sided colonic adenocarcinoma. Ideally, it should be biopsied using a colonoscope and staged with CT scanning of the chest abdomen and pelvis. It should be treated with a right hemicolectomy.
Patients diagnosed as having colorectal cancer should be completely staged using CT of the chest/ abdomen and pelvis. Their entire colon should have been evaluated with colonoscopy or CT colonography. Patients whose tumours lie below the peritoneal reflection should have their mesorectum evaluated with MRI.
Once their staging is complete patients should be discussed within a dedicated colorectal MDT meeting and a treatment plan formulated.
Treatment of colonic cancer
Cancer of the colon is nearly always treated with surgery. Stents, surgical bypass and diversion stomas may all be used as palliative adjuncts. Resectional surgery is the only option for cure in patients with colon cancer. The procedure is tailored to the patient and the tumour location. The lymphatic drainage of the colon follows the arterial supply and therefore most resections are tailored around the resection of particular lymphatic chains (e.g. ileo-colic pedicle for right sided tumours). Some patients may have confounding factors that will govern the choice of procedure, for example a tumour in a patient from a HNPCC family may be better served with a panproctocolectomy rather than segmental resection. Following resection the decision has to be made regarding restoration of continuity. For an anastomosis to heal the key technical factors include; adequate blood supply, mucosal apposition and no tissue tension. Surrounding sepsis, unstable patients and inexperienced surgeons may compromise these key principles and in such circumstances it may be safer to construct an end stoma rather than attempting an anastomosis.
When a colonic cancer presents with an obstructing lesion; the options are to either stent it or resect. In modern practice it is unusual to simply defunction a colonic tumour with a proximal loop stoma. This differs from the situation in the rectum (see below).
Following resection patients with risk factors for disease recurrence are usually offered chemotherapy, a combination of 5FU and oxaliplatin is common.
Rectal cancer
The management of rectal cancer is slightly different to that of colonic cancer. This reflects the rectum’s anatomical location and the challenges posed as a result. Tumours located in the rectum can be surgically resected with either an anterior resection or an abdomino - perineal resection. The technical aspects governing the choice between these two procedures can be complex to appreciate and the main point to appreciate for the MRCS is that involvement of the sphincter complex or very low tumours require APER. In the rectum a 2cm distal clearance margin is required and this may also impact on the procedure chosen. In addition to excision of the rectal tube an integral part of the procedure is a meticulous dissection of the mesorectal fat and lymph nodes (total mesorectal excision/ TME). In rectal cancer surgery invovlement of the cirumferential resection margin carries a high risk of disease recurrence. Because the rectum is an extraperitoneal structure (until you remove it that is!) it is possible to irradiate it, something which cannot be offered for colonic tumours. This has a major impact in rectal cancer treatment and many patients will be offered neoadjuvent radiotherapy (both long and short course) prior to resectional surgery. Patients with T1, 2 and 3 /N0 disease on imaging do not require irradiation and should proceed straight to surgery. Patients with T4 disease will typically have long course chemo radiotherapy. Patients presenting with large bowel obstruction from rectal cancer should not undergo resectional surgery without staging as primary treatment (very different from colonic cancer). This is because rectal surgery is more technically demanding, the anastomotic leak rate is higher and the danger of a positive resection margin in an unstaged patient is high. Therefore patients with obstructing rectal cancer should have a defunctioning loop colostomy.
In the emergency setting, where the bowel has perforated, the risk of an anastomosis is much greater, particularly when the anastomosis is colon-colon. In this situation, an end colostomy is often safer and can be reversed later. When resection of the sigmoid colon is performed and an end colostomy is fashioned the operation is referred to as a Hartmans procedure. Whilst left sided resections are more risky, ileo-colic anastomoses are relatively safe even in the emergency setting and do not need to be defunctioned.

What are phaeochromocytomas? What hormones do they secrete? What symptoms do they cause? How is the diagnosis made? How would you image a suspected phaeochromocytoma? What is the operation of choice for a phaeochromocytoma?
These are hormonally active tumours of the adrenal medulla. They are derived from chromaffin cells. They secrete catecholamines. The classical symptoms include headache, palpitations and sweating. Some are discovered incidentally or during the diagnostic work up of hypertension.
A 24 hour urine collection of catecholamine hormones and their metabolites is undertaken and in patients with phaeochromocytoma the levels vastly exceed the normal range.
Investigating: I would use a combination of CT, MRI and I-MIBG scanning. The previous concerns about contrast agents precipitating crises is no longer valid, should there be concerns, blockade can be used.
Surgical Mx: Laparoscopic adrenalectomy
These are tumours of the adrenal medulla and are derived from chromaffin cells. They are able to secrete catecholamines. Some present with hypertension although only 0.6% of patients with hypertension will be found to have a phaeochromocytoma. Others may be found incidentally during imaging performed for another reason. Approximately 5% of incidental tumours are found to be phaeochromocytomas. Some phaeochromocytomas are linked to genetic syndromes these include; MEN II, von Hippel Lindau and neurofibromatosis type I.
The classical presenting symptoms that are associated with phaeochromocytomas include headache, palpitations and sweating.
Diagnosis of phaeochromocytoma includes 24 hour urine collection for adrenaline, nor adrenaline, metanephrine and nor metanephrine levels. Imaging is with MRI and CT, the latter investigation was previously associated with concerns about the relationship of crises related to the use of contrast media. This risk is now acknowledged to be rare. However, where concerns are raised, adrenergic blockade may be used. Radionucleotide imaging with I-MIBH (meta iodobenzylguanidine) scanning will localise many pheochromocytomas and detected extra adrenal lesions.
Treatment is with surgical excision, laparoscopic adrenalectomy is the favoured approach. The preoperative preparation of these patients is important. It is crucial that the patient is given alpha blockers prior to surgery (phenoxybenzamine). Some patients require additional beta blockade but these are not commenced until alpha blockade has been achieved.
What is the normal arterial pH? How is it maintained within such a narrow range?How is arterial pH usually measured? What is the difference between bicarbonate and standard bicarbonate? What is meant by the term anion gap and why is it used?

It is between 7.35 and 7.40
A number of physiological processes are involved in maintaining pH. Within the blood itself, bicarbonate is present and will tend to combine readily with hydrogen ions to form carbonic acid. This dissociates to form carbon dioxide and water. The lungs and the kidneys provide the main sites of acid base excretion and conservation. Via the lungs, changes in respiratory rate allow for the retention or excretion of carbon dioxide with associated implications for pH. In the kidneys, bicarbonate is retained and over the longer term, hydrogen ion excretion can be increased to address increases hydrogen ions.
Arterial pH is usually measured by a method of arterial blood gas sampling and analysis. ABG machines also directly measure oxygen, carbon dioxide, sodium, potassium and chloride - the bicarb is calculated from the other known parameters.
The bicarbonate value is that which is actually present at the time. However, this can be affected by various respiratory processes. These can be corrected for by adjusting the carbon dioxide level to 5.3kPa. This can change the value of the bicarbonate, which is known as the standard bicarbonate.
Anion Gap: Within the plasma, the balance of cations and anions usually ensures electrochemical neutrality. However, only a proportion of anions are measured, these include bicarbonate and chloride. Other anions are not measured (but are present) and these account for the anion gap. In patients with metabolic acidosis, knowledge of the anion gap is helpful since it can help to distinguish between acidosis resulting from bicarbonate loss (where the anion gap is normal) or acid gain (when it increases).
The normal arterial pH is between 7.35 and 7.40, this corresponds to a hydrogen ion concentration of 40nmol/L. The pH of the body is controlled by a number of physiological mechanisms. Blood and tissue buffering is one of the most ubiquitous systems. Hydrogen ions combine with bicarbonate to form carbonic acid which dissociates under the influence of carbonic anhydrase to form carbon dioxide and water. The control of bicarbonate ion concentration is renal and that of carbon dioxide by the lungs.
In response to acid accumulation, increases in respiratory rate facilitate the excretion of carbon dioxide. Over the longer term, the kidney is able to increase hydrogen ion excretion.
Within the kidney, the proximal convoluted tubule re-absorbs 85% of filtered bicarbonate. In the distal nephron, hydrogen ions are secreted into the collecting duct by an H+ ATPase pump. The excreted acid is generated in the tubular cells from the formation of carbonic acid. When it dissociates, the hydrogen ion is excreted and the bicarbonate ion is retained. Urinary buffers such as ammonium ions serve to address this hydrogen ion load. However, in the normal situation, urine is slightly acidic with a pH of between 5 and 6.
Interpretation of acid base changes
Clinically, the most useful method of assessing acid base balance is through the measurement of arterial blood gases. These are collected from a main artery (usually radial) into a syringe that contains an anticoagulant. The pO2, pH and pCO2 are directly measured and the bicarbonate is calculated using the Henderson Hasselbach equation The Henderson Hasselbach equation is pH=pK+log [HCO3]/[H2CO3]. The pK for the bicarbonate/ carbonic acid system is 6.1 and the carbonic acid is usually viewed as being synonymous with carbon dioxide. The key message about the equation is that it illustrates that the pH depends upon the ratio of bicarbonate to carbon dioxide. One value that is provided by arterial blood gas measurements is the standard bicarbonate. The standard bicarbonate is the value that is obtained when the pCO2 is corrected to 5.3kPa, it has the effect of removing any respiratory component. Usually, the standard bicarbonate is between 22 and 26 mmol/L increases are consistent with metabolic alkalosis and values below this range suggest metabolic acidosis.
Anion gap
Other ions measured with arterial blood gas machines are sodium, potassium and chloride. Chloride and bicarbonate carry a negative charge and are thus anions. Extracellular fluid is normally electrochemically neutral. However, the cations and anions that are measured do not usually balance precisely, the difference arises because there are other anions in the plasma that are not usually measured. This difference is termed the anion gap. Metabolic acidosis can arise through two main mechanisms, bicarbonate loss or acid gain. In the former, there is an increase in plasma chloride levels so that the anion gap remains constant. However, in the latter, where there is an increased production of acid, there is an increase in the anion gap.
It is not uncommon for patients to have more than one disturbance of acid base metabolism. For example they may have a respiratory acidosis due to a narcotic overdose and a metabolic alkalosis due to vomiting. In these situations, the pH will represent the sum total of all processes combined. Careful interpretation of the arterial blood gases will allow the underlying causes to be elucidated.

What are the key macroscopic differences between ulcerative colitis and Crohn’s disease? What key histological feature helps distinguish ulcerative colitis from Crohns disease?
Macroscopic: Ulcerative colitis is confined to the colon and spreads in a progressive fashion from the rectum proximally. Crohn’s disease is patchy in its distribution with the terminal ileum being the commonest site of disease. Indeed, Crohn’s can affect any segment of the GI tract from mouth to anus. At the disease site, ulcerative colitis is a condition that predominantly affects the mucosa, Crohn’s disease is transmural.
Histological: Epitheliod granulomas which are more likely to be found in associated with Crohns disease.
Ulcerative colitis is a form of inflammatory bowel disease. Inflammation always starts at rectum, does not spread beyond ileocaecal valve (although backwash ileitis may occur) and is continuous. The peak incidence of ulcerative colitis is in people aged 15-25 years and in those aged 55-65 years. It is less common in smokers.
The initial presentation is usually following insidious and intermittent symptoms. Features include:
- bloody diarrhoea
- urgency
- tenesmus
- abdominal pain, particularly in the left lower quadrant
- extra-intestinal features: include sclerosing cholangitis, iritis and ankylosing spondylitis. Arthritis is the most common extra-intestinal feature in both CD and UC
Common to both Crohn’s disease (CD) and Ulcerative colitis (UC):
- Related to disease activity: Arthritis (pauciarticular, asymmetric), Erythema nodosum, Osteoporosis, Episcleritis (more common in Crohns disease)
- Unrelated to disease activity: Arthritis (polyarticular, symmetric), Pyoderma gangrenosum, Clubbing, Primary sclerosing cholangitis (much more common in UC), Uveitis (more common in UC)
Pathology
- Red, raw mucosa, bleeds easily
- No inflammation beyond submucosa (unless fulminant disease)
- Widespread superficial ulceration with preservation of adjacent mucosa which has the appearance of polyps (‘pseudopolyps’)
- Inflammatory cell infiltrate in lamina propria
- Neutrophils migrate through the walls of glands to form crypt abscesses
- Depletion of goblet cells and mucin from gland epithelium
- Granulomas are infrequent
Barium enema
- Loss of haustrations
- Superficial ulceration, ‘pseudopolyps’
- Long standing disease: colon is narrow and short -‘drainpipe colon’
Endoscopy
- Superficial inflammation of the colonic and rectal mucosa
- Continuous disease from rectum proximally
- Superficial ulceration, mucosal islands, loss of vascular definition and continuous ulceration pattern.
Management
- Patients with long term disease are at increased risk of development of malignancy
- Acute exacerbations are generally managed with steroids, in chronic patients agents such as azathioprine and infliximab may be used
- Individuals with medically unresponsive disease usually require surgery- in the acute phase a sub total colectomy and end ileostomy. In the longer term a proctectomy will be required. An ileoanal pouch is an option for selected patients
What colonic complications may occur in association with ulcerative colitis? What is the treatment of choice for a patient with ulcerative colitis who is acutely unwell and whose condition has failed to respond to steroids? How and why does this surgical strategy differ from the elective treatment of choice for definitive disease management?
These include the development of colorectal cancer (six fold increased risk)
Bleeding
Toxic megacolon
Colonic perforation
Medically resistant disease
Failure to respond to steroids (UC) : Acutely - sub total colectomy and end ileostomy
The definitive surgical strategy for the management of ulcerative colitis is a pan proctocolectomy. This differs from a sub total colectomy in that the rectum is removed. Resection of the rectum is not undertaken in the emergency setting because this carries considerable increased risk that is not justified in the emergency setting. It should be noted that a sub total colectomy is not the definitive management and that even where a sub total colecotmy is performed, a resection of the rectum will be required subsequently.
Ulcerative colitis is a form of inflammatory bowel disease. Inflammation always starts at rectum, does not spread beyond ileocaecal valve (although backwash ileitis may occur) and is continuous. The peak incidence of ulcerative colitis is in people aged 15-25 years and in those aged 55-65 years. It is less common in smokers.
The initial presentation is usually following insidious and intermittent symptoms. Features include:
- bloody diarrhoea
- urgency
- tenesmus
- abdominal pain, particularly in the left lower quadrant
- extra-intestinal features: include sclerosing cholangitis, iritis and ankylosing spondylitis. Arthritis is the most common extra-intestinal feature in both CD and UC
Common to both Crohn’s disease (CD) and Ulcerative colitis (UC):
- Related to disease activity: Arthritis (pauciarticular, asymmetric), Erythema nodosum, Osteoporosis, Episcleritis (more common in Crohns disease)
- Unrelated to disease activity: Arthritis (polyarticular, symmetric), Pyoderma gangrenosum, Clubbing, Primary sclerosing cholangitis (much more common in UC), Uveitis (more common in UC)
Pathology
- Red, raw mucosa, bleeds easily
- No inflammation beyond submucosa (unless fulminant disease)
- Widespread superficial ulceration with preservation of adjacent mucosa which has the appearance of polyps (‘pseudopolyps’)
- Inflammatory cell infiltrate in lamina propria
- Neutrophils migrate through the walls of glands to form crypt abscesses
- Depletion of goblet cells and mucin from gland epithelium
- Granulomas are infrequent
Barium enema
- Loss of haustrations
- Superficial ulceration, ‘pseudopolyps’
- Long standing disease: colon is narrow and short -‘drainpipe colon’
Endoscopy
- Superficial inflammation of the colonic and rectal mucosa
- Continuous disease from rectum proximally
- Superficial ulceration, mucosal islands, loss of vascular definition and continuous ulceration pattern.
Management
- Patients with long term disease are at increased risk of development of malignancy
- Acute exacerbations are generally managed with steroids, in chronic patients agents such as azathioprine and infliximab may be used
- Individuals with medically unresponsive disease usually require surgery- in the acute phase a sub total colectomy and end ileostomy. In the longer term a proctectomy will be required. An ileoanal pouch is an option for selected patients
What restorative strategies are available following a sub total colectomy for ulcerative colitis?
The only restorative option is completion proctectomy and formation of an ileoanal pouch. This is usually anastomosed to the anal verge. Very rarely, some surgeons will offer a continent Koch pouch ileostomy. Ileo-rectal anastomosis is not an accepted treatment for ulcerative colitis. Many patients choose not to undergo pouch surgery with its associated lifestyle restrictions. These will be left with a permanent end ileostomy.
Ulcerative colitis is a form of inflammatory bowel disease. Inflammation always starts at rectum, does not spread beyond ileocaecal valve (although backwash ileitis may occur) and is continuous. The peak incidence of ulcerative colitis is in people aged 15-25 years and in those aged 55-65 years. It is less common in smokers.
The initial presentation is usually following insidious and intermittent symptoms. Features include:
- bloody diarrhoea
- urgency
- tenesmus
- abdominal pain, particularly in the left lower quadrant
- extra-intestinal features: include sclerosing cholangitis, iritis and ankylosing spondylitis. Arthritis is the most common extra-intestinal feature in both CD and UC
Common to both Crohn’s disease (CD) and Ulcerative colitis (UC):
Related to disease activity: Arthritis (pauciarticular, asymmetric), Erythema nodosum, Osteoporosis, Episcleritis (more common in Crohns disease)
Unrelated to disease activity: Arthritis (polyarticular, symmetric), Pyoderma gangrenosum, Clubbing, Primary sclerosing cholangitis (much more common in UC), Uveitis (more common in UC)
Pathology
- Red, raw mucosa, bleeds easily
- No inflammation beyond submucosa (unless fulminant disease)
- Widespread superficial ulceration with preservation of adjacent mucosa which has the appearance of polyps (‘pseudopolyps’)
- Inflammatory cell infiltrate in lamina propria
- Neutrophils migrate through the walls of glands to form crypt abscesses
- Depletion of goblet cells and mucin from gland epithelium
- Granulomas are infrequent
Barium enema
- Loss of haustrations
- Superficial ulceration, ‘pseudopolyps’
- Long standing disease: colon is narrow and short -‘drainpipe colon’
Endoscopy
- Superficial inflammation of the colonic and rectal mucosa
- Continuous disease from rectum proximally
- Superficial ulceration, mucosal islands, loss of vascular definition and continuous ulceration pattern.
Management
- Patients with long term disease are at increased risk of development of malignancy
- Acute exacerbations are generally managed with steroids, in chronic patients agents such as azathioprine and infliximab may be used
- Individuals with medically unresponsive disease usually require surgery- in the acute phase a sub total colectomy and end ileostomy. In the longer term a proctectomy will be required. An ileoanal pouch is an option for selected patients
What is a malignant melanoma? What are the risk factors for the development of melanoma? What types of melanoma are recognised? When a melanoma is resected, what single pathological variable correlates most closely with prognosis?
It is a malignant tumour arising from the epidermal melanocyte.
Risk Factors: Both environmental and phenotypical features are recognised. The former include; Intermittent sun exposure associated with sun burn and use of sun beds at young age. The strongest phenotypical risk factor is increased numbers of melanocytic naevi and dysplastic naevus syndrome.
The commonest variant is the superficial spreading melanoma, typically the female leg or male back are usually affected, these account for 65% of lesions. About 28% of lesions are nodular melanoma This term should be strictly applied to those lesions that have no horizontal growth phase. Approximately 7% of lesions are lentigo maligna melanoma, these lesions have a long and relatively latent horizontal growth phase. Acral and subungual melanomas may be encountered. The former comprise 10% of all melanomas on white skin, but up to 50% on darker skinned persons and are thus not uncommon. In contrast, subungual melanomas are rare, they are most frequently found in the thumb or toe, they arise from the nail plate and thus produce nail discolouration.
The Breslow thickness, this is a pathological measurement of the vertical growth phase of a melanoma and correlates with survival. Lesions <0.78 mm have a 10 year survival of 95%. In contrast, a depth of >3.6mm has a 10 year survival rate of 30%.
Malignant melanoma: The main diagnostic features (major criteria):
- Change in size
- Change in shape
- Change in colour
Secondary features (minor criteria)
- Diameter >6mm
- Inflammation
- Oozing or bleeding
- Altered sensation
Treatment
- Suspicious lesions should undergo excision biopsy. The lesion should be removed in completely as incision biopsy can make subsequent histopathological assessment difficult.
- Once the diagnosis is confirmed the pathology report should be reviewed to determine whether further re-excision of margins is required (see below):
Margins of excision-Related to Breslow thickness
- Lesions 0-1mm thick: 1cm
- Lesions 1-2mm thick: 1- 2cm (Depending upon site and pathological features)
- Lesions 2-4mm thick: 2-3 cm (Depending upon site and pathological features)
- Lesions >4 mm thick: 3cm
Further treatments such as sentinel lymph node mapping, isolated limb perfusion and block dissection of regional lymph node groups should be selectively applie
What staging is performed for patients with melanoma? How are patients with nodal disease in the groin typically managed? If you were clinically suspicious of a subungual melanoma, what site would you biopsy?
Rather interestingly, little or no staging is performed either before or following resection of primary melanomas. In those patients with worrisome lesions, there is a role for sentinel lymph node biopsy. Patients with nodal disease or relapse at any site, are then fully staged with CT scanning of the head, chest, abdomen and pelvis. PET scanning is also used.
Nodal disease groin: This depends upon the overall disease stage. However, isolated groin nodal disease is usually managed by a block dissection of the groin.
Subungual melanomas are rare and originate in the nail bed. Therefore, suspicious lesions are managed by removal of the nail and biopsy of the nail bed. If the diagnosis is confirmed then specialist surgical resection is required. Rarely, this may involve amputation of the affected digit.
Malignant melanoma: The main diagnostic features (major criteria):
- Change in size
- Change in shape
- Change in colour
Secondary features (minor criteria)
- Diameter >6mm
- Inflammation
- Oozing or bleeding
- Altered sensation
Treatment
- Suspicious lesions should undergo excision biopsy. The lesion should be removed in completely as incision biopsy can make subsequent histopathological assessment difficult.
- Once the diagnosis is confirmed the pathology report should be reviewed to determine whether further re-excision of margins is required (see below):
Margins of excision-Related to Breslow thickness
Lesions 0-1mm thick: 1cm
Lesions 1-2mm thick: 1- 2cm (Depending upon site and pathological features)
Lesions 2-4mm thick: 2-3 cm (Depending upon site and pathological features)
Lesions >4 mm thick: 3cm
How are the adrenal glands organised? From which amino acid are adrenaline and nor adrenaline derived? What provides the stimulus for the release of adrenaline and nor-adrenaline?
The paired adrenal glands consist of a cortex and medulla. The former region is divided into three distinct histological zones; the glomerulosa, fasciculata and reticularis. These secrete (in order); mineralocorticoids, glucocorticoids and androgens. The medulla contains chromaffin cells and secretes adrenaline and nor adrenaline - made from tyrosine - release stimulated by the sympathetic nervous system via pre gangionic fibres from the thoracic spinal cord.
Adrenal medulla
The chromaffin cells of the adrenal medulla secrete the catecholamines noradrenaline and adrenaline. The medulla is innervated by the splanchnic nerves; the preganglionic sympathetic fibres secrete acetylcholine causing the chromaffin cells to secrete their contents by exocytosis.
Phaeochromocytomas are derived from these cells and will secrete both adrenaline and nor adrenaline.
The glucocorticoids and aldosterone are mostly bound to plasma proteins in the circulation. Glucocorticoids are inactivated and excreted by the liver.
What is cryoprecipitate? What are the main constituents of cryoprecipitate? When is it typically used? Is cross matching necessary?
It is a blood product obtained by the centrifugation of plasma.
Main constituents: Fibrinogen, von Willebrand factor, factor VIII, factor XIII and fibronectin.
Used in bleeding due to haemophilia when factor concentrates are not available. Bleeding following massive transfusion.
Cross matching is not strictly necessary, though it is commonly done. For plasma products its the reverse of the blood group.
- Blood product made from plasma
- Usually transfused as 6 unit pool
- Indications include massive haemorrhage and uncontrolled bleeding due to haemophilia
Composition:
- Factor VIII: 100IU
- Fibrinogen: 250mg
- von Willebrand factor: Variable
- Factor XIII: Variable
One of the complications following tonsillectomy is haemorrhage. Describe the different types of haemorrhage that may occur following tonsillectomy and explain why they occur?
Tonsillectomy is a recognised cause of both primary and secondary haemorrhage. This is a particular problem in this patient group for two reasons, firstly because the tonsillar bed is highly vascular and secondly because excessive bleeding can result in airway compromise. Both primary and secondary haemorrhage can complicate tonsillectomy. Primary haemorrhage is the result of vessel injury or dislodgement of a clot. When guillotine tonsillectomy was popular, pressure haemostasis and clot formation was the usual haemostatic method employed. In the immediate post operative period the clot would dislodge and brisk haemorrhage would then ensue. Secondary haemorrhage is usually a delayed event and typically occurs 7-14 days following surgery. In the case of tonsillectomy, the tonsillar bed becomes infected and then bleeds as a result of sloughing of vessel walls.
Uncontrolled haemorrhage will ultimately result in hypovolaemic shock. This can be the starting point for a complex cycle of tissue hypoperfusion, localised hypoxia and acidosis which further inhibits tissue metabolism and localised hypothermia. Since these factors inhibit the effective functioning of the coagulation cascade they can all contribute to the progression of haemorrhage. In addition, significant haemorrhage can result in the consumption of clotting products which further exacerbates the problem. It is therefore important to both identify and treat haemorrhage promptly. In surgical practice haemorrhage can be described as primary and secondary, surgical and non surgical. Primary haemorrhage is an immediate or early event and is either the result of technical failure (e.g. knot slippage) , unrecognised vessel trauma or dislodgement of clot. Secondary haemorrhage is caused by the sloughing of a vessel wall and typically occurs 7-14 days post operatively. Causes of secondary haemorrhage include infection, pressure necrosis or malignancy. Surgical haemorrhage typically occurs as a direct result of the surgical process. Non surgical haemorrhage is the generalised oozing that can be seen from all raw surfaces and is often due to coagulopathy. The practical relevance of these categories is that primary, surgical haemorrhage usually calls for an immediate surgical solution. Intra operatively, the usual method is to control the bleeding through use of ligatures, clips or stapling devices. Occasionally, the cause of bleeding is from exposed raw surface, iatrogenic splenic injury is a classic cause of this, and such events may require use of additional agents such as haemostatic therapies such as argon plasma coagulation or application of topical haemostatic agents. Primary non surgical haemorrhage should usually be avoided by anticipating and treating coagulopathy before it becomes established. The only realistic option in such circumstances is to pack the affected area and return the patient to a critical care environment to normalise their physiology for 24 hours or so prior to returning to theatre and removing the packs. Identification of haemorrhage in the post operative patient can be surprisingly difficult and in addition to standard bedside haemodynamic parameters (pulse, BP, capillary refill and urine output) it is worth checking devices such as drains and the wound itself to ensure that bleeding is not being overlooked
Imagine that you are called to review a 74 year old man following a revision total hip arthroplasty because the nursing staff are concerned that there may be a post operative haemorrhage. Outline how you would assess such a patient.
I would assess their airway, breathing and circulation. I would pay particular attention to their temperature, pulse , blood pressure and capillary refill. I would inspect the wound for evidence of bleeding and if a drain had been inserted I would check that it was on free drainage and that there was no blood present in it. I would check the patients FBC. However, it is not uncommon for this to be normal initially.
Uncontrolled haemorrhage will ultimately result in hypovolaemic shock. This can be the starting point for a complex cycle of tissue hypoperfusion, localised hypoxia and acidosis which further inhibits tissue metabolism and localised hypothermia. Since these factors inhibit the effective functioning of the coagulation cascade they can all contribute to the progression of haemorrhage. In addition, significant haemorrhage can result in the consumption of clotting products which further exacerbates the problem. It is therefore important to both identify and treat haemorrhage promptly. In surgical practice haemorrhage can be described as primary and secondary, surgical and non surgical. Primary haemorrhage is an immediate or early event and is either the result of technical failure (e.g. knot slippage) , unrecognised vessel trauma or dislodgement of clot. Secondary haemorrhage is caused by the sloughing of a vessel wall and typically occurs 7-14 days post operatively. Causes of secondary haemorrhage include infection, pressure necrosis or malignancy. Surgical haemorrhage typically occurs as a direct result of the surgical process. Non surgical haemorrhage is the generalised oozing that can be seen from all raw surfaces and is often due to coagulopathy. The practical relevance of these categories is that primary, surgical haemorrhage usually calls for an immediate surgical solution. Intra operatively, the usual method is to control the bleeding through use of ligatures, clips or stapling devices. Occasionally, the cause of bleeding is from exposed raw surface, iatrogenic splenic injury is a classic cause of this, and such events may require use of additional agents such as haemostatic therapies such as argon plasma coagulation or application of topical haemostatic agents. Primary non surgical haemorrhage should usually be avoided by anticipating and treating coagulopathy before it becomes established. The only realistic option in such circumstances is to pack the affected area and return the patient to a critical care environment to normalise their physiology for 24 hours or so prior to returning to theatre and removing the packs. Identification of haemorrhage in the post operative patient can be surprisingly difficult and in addition to standard bedside haemodynamic parameters (pulse, BP, capillary refill and urine output) it is worth checking devices such as drains and the wound itself to ensure that bleeding is not being overlooked
You are involved in a challenging cholecystectomy. The gallbladder is densely adherent to surrounding structures and during the course of surgery there is damage to the common hepatic artery will significant blood loss and a time consuming repair. Finally, the surgeon dissects the gallbladder off the liver and following this process there is an on-going and constant ooze from the raw liver surface. What are the principles that should govern the management this?
The patient has undergone a long and complex procedure with significant blood loss. Coagulopathy is likely. It is reasonable to apply topical haemostatic agents in an attempt to control the situation. However, if this is not rapidly achieved, then the safest option is to pack the liver and normalise the physiology before returning to theatre to remove the packs 24 hours later.
Uncontrolled haemorrhage will ultimately result in hypovolaemic shock. This can be the starting point for a complex cycle of tissue hypoperfusion, localised hypoxia and acidosis which further inhibits tissue metabolism and localised hypothermia. Since these factors inhibit the effective functioning of the coagulation cascade they can all contribute to the progression of haemorrhage. In addition, significant haemorrhage can result in the consumption of clotting products which further exacerbates the problem. It is therefore important to both identify and treat haemorrhage promptly. In surgical practice haemorrhage can be described as primary and secondary, surgical and non surgical. Primary haemorrhage is an immediate or early event and is either the result of technical failure (e.g. knot slippage) , unrecognised vessel trauma or dislodgement of clot. Secondary haemorrhage is caused by the sloughing of a vessel wall and typically occurs 7-14 days post operatively. Causes of secondary haemorrhage include infection, pressure necrosis or malignancy. Surgical haemorrhage typically occurs as a direct result of the surgical process. Non surgical haemorrhage is the generalised oozing that can be seen from all raw surfaces and is often due to coagulopathy. The practical relevance of these categories is that primary, surgical haemorrhage usually calls for an immediate surgical solution. Intra operatively, the usual method is to control the bleeding through use of ligatures, clips or stapling devices. Occasionally, the cause of bleeding is from exposed raw surface, iatrogenic splenic injury is a classic cause of this, and such events may require use of additional agents such as haemostatic therapies such as argon plasma coagulation or application of topical haemostatic agents. Primary non surgical haemorrhage should usually be avoided by anticipating and treating coagulopathy before it becomes established. The only realistic option in such circumstances is to pack the affected area and return the patient to a critical care environment to normalise their physiology for 24 hours or so prior to returning to theatre and removing the packs. Identification of haemorrhage in the post operative patient can be surprisingly difficult and in addition to standard bedside haemodynamic parameters (pulse, BP, capillary refill and urine output) it is worth checking devices such as drains and the wound itself to ensure that bleeding is not being overlooked
What is an open fracture? Do you know of any grading systems for open fractures? What is the usual immediate management of open fractures?
A fracture that occurs in communication with the breach of the surrounding skin or viscera.
The Gustilo and Anderson is a commonly used system and is relatively reproducible. The system considers three grades of injury, 1-3, depending upon the size of the wound, degree of contamination and bony disruption. The third category is subdivided to consider the effects of contamination and vascular injury.
Mx: Careful assessment and management of associated injuries. It is important to determine the nature and extent of injury with imaging and clinical examination. This should be followed by administration of antibiotics and tetanus toxoid. Early debridement of the wound and temporary fracture stabilisation should usually occur within 6 hours or on the following trauma list.
The term open fracture refers to a disruption of the bony cortex associated with a breach in the overlying skin. Any wound that is present in the same limb as a fracture should be suspected as being representative of an open fracture. One of the main problems with open fractures is the associated injuries to the surrounding soft tissues. Whilst the skin is usually relatively resistant to trauma, underlying muscle can be damaged or devitalised, nerves, blood vessels and periosteum may all be disrupted the degree to which this occurs correlates with the severity of the injury and the outcome. These can be graded using the Gustilo and Anderson system (see below).
GradeInjury
- 1: Low energy wound <1cm
- 2: Greater than 1cm wound with moderate soft tissue damage
- 3: High energy wound > 1cm with extensive soft tissue damage
- 3 A Adequate soft tissue coverage
- 3 B Inadequate soft tissue coverage
- 3 C Associated arterial injury
In Type IIIc injuries, the mangled extremity scoring system (MESS) can help to predict the need for primary amputation.
Initial management should focus on careful patient examination to check for associated injuries, control of haemorrhage and the extent of injury. The area should be carefully imaged, distal neurovascular status established the wound covered with a dressing and antibiotics administered. Early debridement is the cornerstone of the management of open fractures. The aim of the debridement is to remove foreign material and devitalised tissue. In most cases the wound is left open. The wound should be irrigated, generally, 6 litres of saline is used. The fracture should be stabilised and an external fixator is often used in the first instance
How would you debride an open fracture? In what circumstances should the wound be closed primarily?
Under general anaesthesia I would carefully debride all non viable skin and the wound edges as a minimum. I would assess the underlying muscle for its viability and remove any non viable fat or muscle. I would remove all foreign material and bony fragments. Having completed this process I would irrigate the wound with at least 6 litres of saline and stabilise the fracture with an external fixation device.
With the exception of small uncontaminated type I wounds, they should not be primarily closed and re-look and plastic surgical reconstruction is usually needed.
The term open fracture refers to a disruption of the bony cortex associated with a breach in the overlying skin. Any wound that is present in the same limb as a fracture should be suspected as being representative of an open fracture. One of the main problems with open fractures is the associated injuries to the surrounding soft tissues. Whilst the skin is usually relatively resistant to trauma, underlying muscle can be damaged or devitalised, nerves, blood vessels and periosteum may all be disrupted the degree to which this occurs correlates with the severity of the injury and the outcome. These can be graded using the Gustilo and Anderson system (see below).
GradeInjury
- 1: Low energy wound <1cm
- 2: Greater than 1cm wound with moderate soft tissue damage
- 3: High energy wound > 1cm with extensive soft tissue damage
- 3 A Adequate soft tissue coverage
- 3 B Inadequate soft tissue coverage
- 3 C Associated arterial injury
In Type IIIc injuries, the mangled extremity scoring system (MESS) can help to predict the need for primary amputation.
Initial management should focus on careful patient examination to check for associated injuries, control of haemorrhage and the extent of injury. The area should be carefully imaged, distal neurovascular status established the wound covered with a dressing and antibiotics administered. Early debridement is the cornerstone of the management of open fractures. The aim of the debridement is to remove foreign material and devitalised tissue. In most cases the wound is left open. The wound should be irrigated, generally, 6 litres of saline is used. The fracture should be stabilised and an external fixator is often used in the first instance
What is meant by the term neurogenic shock? At what level(s) would you consider spinal cord injury to be compatible with the development of neurogenic shock? In what setting would neurogenic shock be accompanied by bradycardia and why? How is neurogenic shock managed?
This is a form of distributive shock characterised by hypotension where the underlying cause is a loss of systemic vascular resistance owing to a damage to the sympathetic outflow tract following spinal cord injury.
Injury to levels T6 and above. Injuries significantly below this level seldom produce sufficient sympathetic disruption to cause significant neurogenic shock and an alternative cause for shock should be carefully considered in such circumstances.
Injuries above T1 are associated with bradycardia owing to unopposed vagal activity on the heart.
In the first instance conventional resuscitation with intravenous fluids is commenced with the intention of the expanding the circulating blood volume. Thereafter, some patients may require vasopressor infusion and those with bradycardia may benefit from administration of atropine.
Spinal cord injury may produce hypotension due to loss of peripheral sympathetic vasopressor tone. Because of the possibility that hypovolaemia may co-exist with neurogenic shock (since spinal transection is seldom isolated), this should be addressed initially with appropriate fluid resuscitation. Neurogenic shock may mask the normal physiological response to hypovolaemia. An associated head injury is present in up to 25% of spinal cord injury patients.
Neurogenic shock classically occurs in spinal injuries above the level of T6 and is due to loss of sympathetic autonomic outflow below this level. The main presenting feature of all cases of distributive shock occurs secondary to loss of SVR. The CVP is usually unaffected unless there is co-existing hypovolaemia. Cardiac output remains the same or may even be elevated. Where the injury is above the level of T6 there is hypotension and when the level is above T1 there is an associated bradycardia because there is then the added component of unopposed vagal tone.
Management is with intravenous fluid resuscitation to expand the circulating volume and administration of supplementary oxygen. The use of nor adrenaline and / or atropine may also be necessary.
What clinical features are suggestive of a haemothorax? How much blood needs to be present for signs to appear on an erect CXR? What is meant by the term massive haemothorax? What are massive haemothoraces usually due to ?
- Dyspnoea
- Chest pain
- Haemodynamic compromise
- Decreased air entry
- Dull percussion note
Approximately 400ml is needed to blunten the costophrenic angle.
The term massive haemothorax refers the initial drainage of 1000-1500ml of blood or the drainage of 200-250ml of blood per hour for 3-4 hours. - usually due to major vessel injury.
Haemothorax can result from blunt or penetrating chest trauma and small haemothoraces are common. The source of bleeding depends upon the mechanism of injury and ranges from damage to minor intercostal vessels through to disruption of the great vessels. One of the challenging features of significant haemothoraces is that the causative structure is seldom readily accessible for simple compression. Parenchymal lacerations are often low pressure bleeds and will often cease spontaneously. However, significant bleeding is usually suggestive of hilar disruption and the need for surgical exploration. Massive haemothorax is defined as the initial drainage of 1000-1500ml or a drainage rate of 200-250ml per hour over 3-4 hours. On clinical examination the signs of a significant haemothorax are often very obvious. Collapsed neck veins and signs of haemorrhagic shock all suggest blood loss and this coupled with decreased air entry and a dull percussion note together will a history of chest trauma should prompt consideration of the diagnosis. The only pitfall is failing to appreciate its appearances on a supine chest film as there will not be a meniscus and the hazy opacity of the affected lung may not be appreciated. On erect CXR volumes of blood >400ml will usually obscure the costophrenic angle. The widespread use of FAST scanning has led to earlier detection of haemothoraces. The treatment of a haemothorax is insertion of a widebore intercostal chest tube. Massive haemothorax is usually an indication for thoracotomy.
What are the key clinical signs of a tension pneumothorax? Which group of patients are at greatest risk of tension pneumothorax? What are the features on a chest x-ray that are suggestive of a tension pneumothorax?
Chest pain, dyspnoea, hypoxia, hypotension, tracheal deviation, ipsilateral hyperpercussion note, decreased air entry.
Patients with penetrating chest trauma who are mechanically ventilated are at greatest risk.
CXR:
- Lung collapse towards the hilum
- Diaphragmatic depression
- Increased rib separation
- Increased thoracic volume
- Ipsilateral flattening of the heart border
- Contra lateral mediastinal deviation
Tension pneumothorax is a state of positive pressure within a pneumothorax throughout the respiratory cycle. A breach in the pleura allows air into the intra pleural space via a one way valve. The initial pressure pneumothorax expands until positive pressure is present throughout the respiratory cycle. The risk is greatest in the ventilated trauma patient as positive pressure is used. Undiagnosed tension pneumothorax accounts for 3.8% of trauma deaths.
Clinically, the classic features include chest pain, dyspnoea, hypoxia, hypotension, tracheal deviation, ipsilateral hyperpercussion note, decreased air entry. In ventilated patients, cardiovascular disturbance and sub cutaneous emphysema are relatively common and more so than in a case where the patient is breathing spontaneously.
Chest x-ray features
- Lung collapse towards the hilum
- Diaphragmatic depression Increased rib separation
- Increased thoracic volume
- Ipsilateral flattening of the heart border
- Contra lateral mediastinal deviation
Management: Immediate needle decompression followed by definitive wide bore chest drain insertion
What are the biochemical abnormalities associated with pyloric stenosis and their explanation?
The typical abnormality is hypokalaemic hypochloraemic alkalosis associatied with hypovolvaemia and haemoconcentration. The urine is acidic. Within the stomach the parietal cells generate hydrogen and bicarbonate ions, the hydrogen ions enter the stomach lumen and combines with chloride to form hydrochloric acid. Bicarbonate ions enter the circulation. In pyloric stenosis there is preferential loss of hydrochloric acid (because duodenal secretions are reabsorbed). Loss of hydrogen ions causes increased gastric production. Within the kidney, there is a exchange between sodium and hydrogen ions with the result in attempted conservation of sodium and excretion of hydrogen and the generation of acidic urine. As the loss of hydrogen ions progresses, the kidney then exchanges sodium for potassium ions with the subsequent loss of potassium and resultant hypokalaemia.
Pyloric stenosis typically presents in the second to fourth weeks of life with vomiting, although rarely may present later at up to four months. It is caused by hypertrophy of the circular muscles of the pylorus
Epidemiology
- incidence of 4 per 1,000 live births
- 4 times more common in males
- 10-15% of infants have a positive family history
- first-borns are more commonly affected
Features
- ‘projectile’ vomiting, typically 30 minutes after a feed
- constipation and dehydration may also be present
- a palpable mass may be present in the upper abdomen
- hypochloraemic, hypokalaemic alkalosis due to persistent vomiting
Diagnosis is most commonly made by ultrasound or test feed
Management is with Ramstedt pyloromyotomy
As a surgical trainee you are called to review a 73 year old lady who is noted by the nursing staff to be hypoxic with oxygen saturations of 91% on 35% oxygen. Outline how you would investigate this patient?
She underwent a distal gastrectomy as an open procedure 3 days previously. What is the most likely underlying cause?
What ECG changes would make you suspicious of a pulmonary emboli? If a pulmonary embolus were suspected how would you investigate this?
This is a very straightforward scenario and a slick and immediate response is vital. I would investigate this patient with arterial blood gas measurement, chest x-ray, full blood count and an ECG. At the same time I would also administer high flow oxygen via a non re-breathe mask.
The most likely cause is atelectasis. Gastric surgery is often performed through an upper abdominal incision and if inadequate analgesia is administered, then under ventilation of the lung bases is very common.
PE: Whilst the ECG may be normal, a tachycardia is common. More specific signs include signs of RBBB or S1, Q3, T3. Ix: CTPA
Hypoxia is a common problem encountered in surgical patients. It may be asymptomatic and be an incidental finding on routine monitoring. Alternatively, it may be present with symptoms ranging from confusion through to chest pain. Assessment and management usually occur concomitantly. Initial resuscitation is usually based on the administration of high flow oxygen whilst the cause is identified. Symptoms to identify include chest pain, dyspnoea, cough and haemoptysis. A chest examination will usually identify many of the common causes including ventilation induced pneumothorax, atelectasis and chest infection. The clinical examination may be unremarkable in those who have suffered and embolic event or non ST elevation myocardial events. Diagnostic work up usually includes arterial blood gas estimation, chest x-ray, ECG and measurement of the full blood count. Other investigations may be required depending upon the suspected underlying cause. These may include CT pulmonary angiography for suspected pulmonary emboli. Management is directed towards the underlying cause. One of the commonest causes is the development of atelectasis due to hypoventilation of the lung bases (often due to inadequate analgesia). If this common problem is mismanaged then it may progress to hospital acquired pneumonia. Pneumothoraces are managed with either observation or tube decompression, the latter is mandatory if the patient is being mechanically ventilated as they can easily develop a tension pneumothorax. Pulmonary emboli are managed with anticoagulation. Massive PEs cannot usually be thrombolysed in surgical patients because of their recent surgery.
What is the commonest malignant liver lesion?
Commonest malignant liver lesion: Metastatic cancer, primary liver tumours are far less common.
What types of primary liver malignancy are you familiar with?
Hepatoblastoma, cholangiocarcinoma, sarcoma, carcinoid and hepatocellular carcinoma. Hepatocellular carcinoma is the most common primary liver malignancy.
Primary liver tumours
The most common primary tumours are cholangiocarcinoma and hepatocellular carcinoma. Overall metastatic disease accounts for 95% of all liver malignancies making the primary liver tumours comparatively rare.
Primary liver tumours include:
- Cholangiocarcinoma
- Hepatocellular carcinoma
- Hepatoblastoma
- Sarcomas (Rare)
- Lymphomas
- Carcinoids (most often secondary although primary may occur)
Hepatocellular carcinoma
These account for the bulk of primary liver tumours (75% cases). Its worldwide incidence reflects its propensity to occur on a background of chronic inflammatory activity. Most cases arise in cirrhotic livers or those with chronic hepatitis B infection, especially where viral replication is actively occurring. In the UK it accounts for less than 5% of all cancers, although in parts of Asia its incidence is 100 per 100,000.
The majority of patients (80%) present with existing liver cirrhosis, with a mass discovered on screening ultrasound.
Diagnosis
- CT/ MRI (usually both) are the imaging modalities of choice
- a-fetoprotein is elevated in almost all cases
- Biopsy should be avoided as it seeds tumours cells through a resection plane.
- In cases of diagnostic doubt serial CT and αFP measurements are the preferred strategy.
Treatment
- Patients should be staged with liver MRI and chest, abdomen and pelvic CT scan.
- The testis should be examined in males (testicular tumours may cause raised AFP). PET CT may be used to identify occult nodal disease.
- Surgical resection is the mainstay of treatment in operable cases. In patients with a small primary tumour in a cirrhotic liver whose primary disease process is controlled, consideration may be given to primary whole liver resection and transplantation.
- Liver resections are an option but since most cases occur in an already diseased liver the operative risks and post-operative hepatic dysfunction are far greater than is seen following metastectomy.
- These tumours are not particularly chemo or radiosensitive however, both may be used in a palliative setting. Tumour ablation is a more popular strategy.
Survival - Poor, overall survival is 15% at 5 years.
Cholangiocarcinoma
This is the second most common type of primary liver malignancy. As its name suggests these tumours arise in the bile ducts. Up to 80% of tumours arise in the extra hepatic biliary tree. Most patients present with jaundice and by this stage the majority will have disease that is not resectable.
Primary sclerosing cholangitis is the main risk factor. In deprived countries typhoid and liver flukes are also major risk factors.
Diagnosis
- Patients will typically have an obstructive picture on liver function tests.
- CA 19-9, CEA and CA 125 are often elevated
- CT/ MRI and MRCP are the imaging methods of choice.
Treatment
- Surgical resection offers the best chance of cure. Local invasion of peri hilar tumours is a particular problem and this coupled with lobar atrophy will often contra indicate surgical resection.
- Palliation of jaundice is important, although metallic stents should be avoided in those considered for resection.
Survival- poor, approximately 5-10% 5 year survival.
What are the cells of origin or hepatocellular carcinoma and cholangiocarcinoma?
What are the main risk factors for hepatocellular carcinoma? What is the main tumour marker used in the diagnosis of hepatocellular carcinoma? What is the main treatment of hepatocellular carcinoma?
What is the main risk factor for cholangiocarcinoma?
Hepatocellular carcinomas arise from hepatocytes and cholangiocarcinoma from the cells lining the bile ducts.
The main risk factors for hepatocellular carcinoma include infection with hepatitis B and C or long standing cirrhosis. AFP is main tumour marker - it is a major plasma protein produced by the yolk sac and the liver during fetal development. It is thought to be the fetal form of serum albumin.
The main risk factors for cholangiocarcinoma Primary sclerosing cholangitis and liver fluke infections are the main risk factors.
The main treatment is surgical resection. However, important factors to consider include anatomical location, likely residual liver remnant function and absence of metastatic disease. Hepatocellular carcinoma is one of the very few malignancies where the presence of malignancy is not a contra indication to organ transplantation since very selected patients may be treated with total liver resection and immediate transplantation. However, only a very few selected patients are suitable for this modality of treatment and this coupled with organ shortage means that it is rarely used.
Primary liver tumours
The most common primary tumours are cholangiocarcinoma and hepatocellular carcinoma. Overall metastatic disease accounts for 95% of all liver malignancies making the primary liver tumours comparatively rare.
Primary liver tumours include:
- Cholangiocarcinoma
- Hepatocellular carcinoma
- Hepatoblastoma
- Sarcomas (Rare)
- Lymphomas
- Carcinoids (most often secondary although primary may occur)
Hepatocellular carcinoma
These account for the bulk of primary liver tumours (75% cases). Its worldwide incidence reflects its propensity to occur on a background of chronic inflammatory activity. Most cases arise in cirrhotic livers or those with chronic hepatitis B infection, especially where viral replication is actively occurring. In the UK it accounts for less than 5% of all cancers, although in parts of Asia its incidence is 100 per 100,000.
The majority of patients (80%) present with existing liver cirrhosis, with a mass discovered on screening ultrasound.
Diagnosis
- CT/ MRI (usually both) are the imaging modalities of choice
- a-fetoprotein is elevated in almost all cases
- Biopsy should be avoided as it seeds tumours cells through a resection plane.
- In cases of diagnostic doubt serial CT and αFP measurements are the preferred strategy.
Treatment
- Patients should be staged with liver MRI and chest, abdomen and pelvic CT scan.
- The testis should be examined in males (testicular tumours may cause raised AFP). PET CT may be used to identify occult nodal disease.
- Surgical resection is the mainstay of treatment in operable cases. In patients with a small primary tumour in a cirrhotic liver whose primary disease process is controlled, consideration may be given to primary whole liver resection and transplantation.
- Liver resections are an option but since most cases occur in an already diseased liver the operative risks and post-operative hepatic dysfunction are far greater than is seen following metastectomy.
- These tumours are not particularly chemo or radiosensitive however, both may be used in a palliative setting. Tumour ablation is a more popular strategy.
Survival - Poor, overall survival is 15% at 5 years.
Cholangiocarcinoma
This is the second most common type of primary liver malignancy. As its name suggests these tumours arise in the bile ducts. Up to 80% of tumours arise in the extra hepatic biliary tree. Most patients present with jaundice and by this stage the majority will have disease that is not resectable.
Primary sclerosing cholangitis is the main risk factor. In deprived countries typhoid and liver flukes are also major risk factors.
Diagnosis
- Patients will typically have an obstructive picture on liver function tests.
- CA 19-9, CEA and CA 125 are often elevated
- CT/ MRI and MRCP are the imaging methods of choice.
Treatment
- Surgical resection offers the best chance of cure. Local invasion of peri hilar tumours is a particular problem and this coupled with lobar atrophy will often contra indicate surgical resection.
- Palliation of jaundice is important, although metallic stents should be avoided in those considered for resection.
Survival- poor, approximately 5-10% 5 year survival.
How is oxygen transported?
Describe the shape of the oxygen dissociation curve. Why is it this shape? What is the meant by the term Bohr effect?
Almost all oxygen is transported by binding to haemoglobin and less than 1% is dissolved in solution. The oxygen dissociation curve is sigmoidal in shape, this is because when haemoglobin binds with a single oxygen molecule it results in a conformational change in the protein structure that facilitates binding of the next molecule.
The Bohr effect refers to a shift of the oxygen dissociation curve to the right. This indicates that there is a reduction in the oxygen affinity of the molecule. It occurs as a result of increased temperature, increased acidity, increased 2,3 diphosphoglycerate and hypercarbia. With the exception of 2,3 DGP, these conditions are typically found in metabolically active tissues and thus it facilitates oxygen release at the site of greatest need.
Oxygen transport
Almost all oxygen is transported within erythrocytes. It has limited solubility and only 1% is carried as solution. Therefore the amount of oxygen transported will depend upon haemoglobin concentration and its degree of saturation.
Haemoglobin
Globular protein composed of 4 subunits. Haem consists of a protoporphyrin ring surrounding an iron atom in its ferrous state. The iron can form two additional bonds; one with oxygen and the other with a polypeptide chain. There are two alpha and two beta subunits to this polypeptide chain in an adult and together these form globin. Globin cannot bind oxygen but is able to bind to carbon dioxide and hydrogen ions, the beta chains are able to bind to 2,3 diphosphoglycerate. The oxygenation of haemoglobin is a reversible reaction. The molecular shape of haemoglobin is such that binding of one oxygen molecule facilitates the binding of subsequent molecules.
The oxygen dissociation curve describes the relationship between the percentage of saturated haemoglobin and partial pressure of oxygen in the blood. It is not affected by haemoglobin concentration.
Chronic anaemia causes 2, 3 DPG levels to increase, hence shifting the curve to the right
Haldane effect: Shifts to left = for given oxygen tension there is increased saturation of Hb with oxygen i.e. Decreased oxygen delivery to tissues
Bohr effect: Shifts to right = for given oxygen tension there is reduced saturation of Hb with oxygen i.e. Enhanced oxygen delivery to tissues

What is haemoglobin?
It is a globular protein consisting of a haem moiety and a globin chain. The haem moiety consists of ferrous ion and a protoporphrin ring. In adults, the globin component consists of 2 alpha and 2 beta chains. A total of 4 oxygen molecules can bind to each haemoglobin molecule.
Oxygen transport
Almost all oxygen is transported within erythrocytes. It has limited solubility and only 1% is carried as solution. Therefore the amount of oxygen transported will depend upon haemoglobin concentration and its degree of saturation.
Haemoglobin
Globular protein composed of 4 subunits. Haem consists of a protoporphyrin ring surrounding an iron atom in its ferrous state. The iron can form two additional bonds; one with oxygen and the other with a polypeptide chain. There are two alpha and two beta subunits to this polypeptide chain in an adult and together these form globin. Globin cannot bind oxygen but is able to bind to carbon dioxide and hydrogen ions, the beta chains are able to bind to 2,3 diphosphoglycerate. The oxygenation of haemoglobin is a reversible reaction. The molecular shape of haemoglobin is such that binding of one oxygen molecule facilitates the binding of subsequent molecules.
The oxygen dissociation curve describes the relationship between the percentage of saturated haemoglobin and partial pressure of oxygen in the blood. It is not affected by haemoglobin concentration.
Chronic anaemia causes 2, 3 DPG levels to increase, hence shifting the curve to the right
Haldane effect: Shifts to left = for given oxygen tension there is increased saturation of Hb with oxygen i.e. Decreased oxygen delivery to tissues
Bohr effect: Shifts to right = for given oxygen tension there is reduced saturation of Hb with oxygen i.e. Enhanced oxygen delivery to tissues

What are the main sensors responsible for the control of respiration? What is the most important driver for an increase in the respiratory rate of an otherwise well person?
Whilst intrinsic respiratory drive is provided by the respiratory centres in the pons and medulla. The main sensors that modulate respiratory activity are the centrally and peripherally located chemoreceptors. Central chemoreceptors are located on the central surface of the medulla and are sensitive to changes in the pH of CSF. Peripheral chemoreceptors are located in the carotid bodies and aortic arch and are more sensitive to changes in oxygen levels.
An increase in the partial pressure of carbon dioxide is the most important drive for respiratory rate in an otherwise well person.
- Control of ventilation is coordinated by the respiratory centres, chemoreceptors, lung receptors and muscles.
- Automatic, involuntary control of respiration occurs from the medulla.
- The respiratory centres control the respiratory rate and the depth of respiration.
Respiratory centres
- Medullary respiratory centre: Inspiratory and expiratory neurones. Has ventral group which controls forced voluntary expiration and the dorsal group controls inspiration. Depressed by opiates.
- Apneustic centre: Lower pons. Stimulates inspiration - activates and prolongs inhalation. Overridden by pneumotaxic control to end inspiration
- Pneumotaxic centre: Upper pons, inhibits inspiration at a certain point. Fine tunes the respiratory rate.
Ventillatory variables
- Levels of pCO2 most important in ventilation control
- Levels of O2 are less important.
- Peripheral chemoreceptors: located in the bifurcation of carotid arteries and arch of the aorta. They respond to changes in reduced pO2, increased H+ and increased pCO2 in ARTERIAL BLOOD.
- Central chemoreceptors: located in the medulla. Respond to increased H+ in BRAIN INTERSTITIAL FLUID to increase ventilation. NB the central receptors are NOT influenced by O2 levels.
Lung receptors include:
- Stretch receptors: respond to lung stretching causing a reduced respiratory rate
- Irritant receptors: respond to smoke etc causing bronchospasm
- J (juxtacapillary) receptors
Describe how central chemoreceptors are stimulated?
Within the blood and plasma, carbon dioxide highly soluble and dissociates to form carbonic acid. However, the hydrogen ions that result from its dissociation cannot pass the blood brain barrier. However, the carbon dioxide that is dissolved in the blood, is readily transported across the blood brain barrier and into the CSF. Here, it can once again form carbonic. However, the hydrogen ions that are then produced serve as a potent stimulus of the centrally located receptors.
- Control of ventilation is coordinated by the respiratory centres, chemoreceptors, lung receptors and muscles.
- Automatic, involuntary control of respiration occurs from the medulla.
- The respiratory centres control the respiratory rate and the depth of respiration.
Respiratory centres
- Medullary respiratory centre: Inspiratory and expiratory neurones. Has ventral group which controls forced voluntary expiration and the dorsal group controls inspiration. Depressed by opiates.
- Apneustic centre: Lower pons. Stimulates inspiration - activates and prolongs inhalation. Overridden by pneumotaxic control to end inspiration
- Pneumotaxic centre: Upper pons, inhibits inspiration at a certain point. Fine tunes the respiratory rate.
Ventillatory variables
- Levels of pCO2 most important in ventilation control
- Levels of O2 are less important.
- Peripheral chemoreceptors: located in the bifurcation of carotid arteries and arch of the aorta. They respond to changes in reduced pO2, increased H+ and increased pCO2 in ARTERIAL BLOOD.
- Central chemoreceptors: located in the medulla. Respond to increased H+ in BRAIN INTERSTITIAL FLUID to increase ventilation. NB the central receptors are NOT influenced by O2 levels.
Lung receptors include:
- Stretch receptors: respond to lung stretching causing a reduced respiratory rate
- Irritant receptors: respond to smoke etc causing bronchospasm
- J (juxtacapillary) receptors
What airway devices are you familiar with?
The airways devices in common use include;
- oropharyngeal airway
- laryngeal mask
- endotracheal tube
- tracheostomy
Oropharyngeal airway
- Easy to insert and use
- No paralysis required
- Ideal for very short procedures
- Most often used as bridge to more definitive airway
Laryngeal mask
- Widely used
- Very easy to insert
- Device sits in pharynx and aligns to cover the airway
- Poor control against reflux of gastric contents
- Paralysis not usually required
- Commonly used for wide range of anaesthetic uses, especially in day surgery
- Not suitable for high pressure ventilation (small amount of PEEP often possible)
Tracheostomy
- Reduces the work of breathing (and dead space)
- May be useful in slow weaning
- Percutaneous tracheostomy widely used in ITU
- Dries secretions, humidified air usually required
Endotracheal tube
- Provides optimal control of the airway once cuff inflated
- May be used for long or short term ventilation
- Errors in insertion may result in oesophageal intubation (therefore end tidal CO2 usually measured)
- Paralysis often required
- Higher ventilation pressures can be used
In what circumstances is a laryngeal mask a potentially dangerous airway? What hazards may accompany endotracheal intubation? How can oesophageal intubation be prevented? How do the endotracheal tubes used in adults differ from those used in young children and babies?
LMA: When there is the potential for reflux of gastric contents. The laryngeal mask does not occlude the trachea and therefore in the event of a significant reflux event, patients may aspirate.
Endotracheal intubation hazards: These include; damage to dentition, incorrectly intubating the oesophagus, damage to oropharynx/ trachea, single lung intubation and formation of pneumothorax with positive pressure ventilation.
Prevention oesophageal intubation: Training and familiarity with landmarks, auscultation of the chest and abdomen following intubation and attaching and end tidal carbon dioxide monitor to the circuit.
Paediatric endotracheal tubes do not have a cuff.
Oropharyngeal airway:
- Easy to insert and use
- No paralysis required
- Ideal for very short procedures
- Most often used as bridge to more definitive airway
Laryngeal mask
- Widely used
- Very easy to insert
- Device sits in pharynx and aligns to cover the airway
- Poor control against reflux of gastric contents
- Paralysis not usually required
- Commonly used for wide range of anaesthetic uses, especially in day surgery
- Not suitable for high pressure ventilation (small amount of PEEP often possible)
Tracheostomy
- Reduces the work of breathing (and dead space)
- May be useful in slow weaning
- Percutaneous tracheostomy widely used in ITU
- Dries secretions, humidified air usually required
Endotracheal tube
- Provides optimal control of the airway once cuff inflated
- May be used for long or short term ventilation
- Errors in insertion may result in oesophageal intubation (therefore end tidal CO2 usually measured)
- Paralysis often required
- Higher ventilation pressures can be used
How are thyroid hormones synthesised? What are the effects of thyroid hormone? Which thyroid hormone is more biologically active? How are thyroid hormones transported in the blood stream? How is the release of thyroid hormones controlled?
Iodide ions in the blood stream are transported via an active process from the extracellular space to the follicular epithelium. Once these enter the colloid filled spaces they are then converted to iodine. This combines with tyrosine. Two forms are produced; monoiodotyrosine and diiodotyrosine. These combine to produce the two thyroid hormones. Triiodothyronine is produced through the combination of monoiodotyrosine and diiodotyrosine. Thyroxine is produced by the combination of diiodotyrosine with diiodotyrosine.
Upon entering the cell, T4 is converted to T3. This then binds to nuclear receptors. Systems thus affected include increase in basal metabolic rate, increased glucose absorption and synthesis, fatty acid break down, increased protein turnover. In the cardiorespiratory system, the respiratory rate increases and so too does the heart rate. Cardiac output is increased. Thyroid hormones have a sympathomimetic effect with many effects similar to beta adrenergic stimulation.
T3 is the more active thyroid hormone. Although, it has a shorter half life.
Transport in the blood stream: They are usually bound. Either to albumin or thyroxine binding globulin.
The stimulus for the release begins in the hypothalamus, this releases thyrotropin releasing hormone. This stimulates the anterior pituitary to release thyroid stimulating hormone. TSH acts on the gland to absorb thyroglobulin into follicular cells this is broken down to release T3 and T4. These are released into the systemic circulation. In turn, they exert a negative feedback effect on TRH and TSH release.
Hormones of the thyroid gland:
- Triiodothyronine T3: Major hormone active in target cells
- Thyroxine T4: Most prevalent form in plasma, less biologically active than T3
- Calcitonin: Lowers plasma calcium
Synthesis and secretion of thyroid hormones:
- Thyroid actively concentrates iodide to twenty five times the plasma concentration.
- Iodide is oxidised by peroxidase in the follicular cells to atomic iodine which then iodinates tyrosine residues contained in thyroglobulin.
- Iodinated tyrosine residues in thyroglobulin undergo coupling to either T3 or T4.
- Process is stimulated by TSH, which stimulates secretion of thyroid hormones.
- The normal thyroid has approximately 3 month reserves of thyroid hormones.
LATS and Graves disease
In Graves disease patients develop IgG antibodies to the TSH receptors on the thyroid gland. This results in chronic and long term stimulation of the gland with release of thyroid hormones. The typically situation is raised thyroid hormones and low TSH. Thyroid receptor autoantibodies should be checked in individuals presenting with hyperthyroidism as they are present in up to 85% cases.
A 79 year old female is admitted following a minor trip at home. Following assessment in the emergency department an x-ray of the hip is obtained.
What are the main risk factors for this condition?
What are the key principals of managing these injuries?
What surgical procedure should be performed in this case and why? Outline the stages of this procedure

There is evidence of an intertrochanteric fracture with comminution and separation of the lesser trochanter.
Risk Factors: These are usually pathological fractures which occur in elderly females on a background of underlying osteoporosis. Other risk factors are essentially those of pathological fractures since high velocity injuries affecting otherwise normal bone are rare in this age group
Key principles Mx: The immediate priority is to provide analgesia and stabilise the patient. They should be admitted to an orthopaedic unit and undergo a comprehensive history and examination. Many of these elderly patients will have co-morbidities, polypharmacy and other factors that may either impact on any planned surgery or complicate the recovery process. All patients should be optimised with a view to early surgical intervention and fracture fixation.
In the post operative period there should be close liaison with a geriatrician and surgeon with a focus on early and intensive rehabilitation. In most cases the underlying cause is one of osteoporosis secondary prevention should be commenced and consists of a bisphosphonate and calcium supplements which are continued long term.
This particular fracture lies outside the joint capsule and thus will not compromise the vascularity of the femoral head. Therefore fixation with a dynamic hip screw or similar would be sufficient management.
The patient will require suitable anaesthesia either regional or general. They are carefully positioned on a fracture table and an image intensifier is used to allow the operating surgeon to position the leg in such a way as to reduce the fracture prior to making the skin incision. After the skin is prepared and draped a longitudinal incision centered on the greater trochanter is made. Once the bony surface is exposed a guide wire is inserted into the femoral head under image guidance. This is exchanged for a cannulated compression screw which approximates the displaced fragments. The screw is attached to a plate that runs along the lateral aspect of the upper femur. Screws are placed into the plate to hold the reduction. The wound are closed in layers. A drain can be used if deemed necessary.
Hip fractures
Background
Neck of femur (NOF) fracture is a common orthopaedic presentation, with over 65000 fractures in the UK per year. Like many orthopaedic injuries, there is a bimodal age distribution. It is imperative to distinguish between the high energy injury in a young patient, and the low energy osteoporotic fracture in the elderly, as their management aims are very different:
Young patient - Usually high energy trauma (e.g road traffic accident, horse riding) and needs treating in accordance with Advanced Trauma Life Support (ATLS) principles. Will often have associated injuries. Aim is to retain the patients own anatomy, and optimise their function.
Elderly patient - Predominantly female, fall from standing height (fragility fracture). Often patients have multiple comorbidities that will ultimately dictate their prognosis. Aim of orthopaedic treatment is to immediately regain patient mobility so that morbidity (infection, thromboembolic events, pressure sores etc) and mortality associated with prolonged bed rest is avoided. Left untreated, a neck of femur fracture can be considered a terminal event. Historically, mortality associated with elderly hip fracture is 10% at one month, and 30% at one year. However, this has been improved in the UK with the introduction of multidisciplinary, orthogeriatric lead care and the National Hip Fracture Database and Best Practice Tariff.
Pertinent anatomy
Osteology - normal neck-shaft angle is 130 +/- 7 degrees, and 10 +/- 7 degrees of neck anteversion.
Vascular supply - The predominant blood supply to the femoral head and neck is from the medial and lateral femoral circumflex arteries (branches of profunda femoris). These anastomose and pierce the joint capsule at the base of the neck, mainly posteriorly. There is a small vascular contribution from the artery of the ligament teres. Understanding the blood supply is fundamental to the decision making process in treating NOF fractures.
Presentation and initial management
Typically, patients present with pain in the hip/groin, a shortened, abducted, externally rotated leg (due to the unopposed pull of the muscles that act across the hip joint) and the inability to straight-leg-raise. With undisplaced fractures, signs are more subtle.
High energy injuries should be treated in line with ATLS principles. All patients should be fluid resuscitated, have adequate pain relief (often with a fascio-iliiaca nerve block), and be optimised for surgery. In addition, elderly patients should be assessed by an orthogeriatrician.
Imaging
Anteroposterior and cross-table lateral plain radiographs are sufficient to diagnose the majority of NOF fractures. If the fracture extends below the level of the lesser trochanter, or there is any possibility of pathological fracture, full length femur views are essential to plan surgery.
Where there is a high index of suspicion of fracture, but plain radiographs are inconclusive, gold standard investigation is MRI. However, if unavailable within 24 hours, or if the patient will not tolerate MRI, CT is appropriate. The majority of fractures can be seen with modern CT techniques, and so this is becoming first line in many hospitals.
Classification
There has been a move away from named classification systems towards descriptive classification systems.
Two main types of NOF exist: Intra-capsular, and extra-capsular. Extra-capsular fractures are further divided into pertrochanteric or subtrochanteric (within 5cm distal to the lesser trochanter). All fractures are then described as undisplaced, minimally displaced, or displaced.
Femoral neck and head blood supply disruption is common with intracapsular NOF fractures, and rare with extracapsular fractures. This fundamental principle underpins the practise of arthroplasty for intracapsular fractures, and fixation for extracapsular fractures.
If you wish to use a named classification system, the most commonly used are below:
Elderly intracapsular - Garden Classification
Young intrasapsular - Pauvels Classification
Intertrochanteric - Evans
Subtrochanteric - Russell Taylor
Treatment
In general, NOF fractures are treated operatively except if the patient is deemed unlikely to survive an anaesthetic. Best Practice Tarif (BPT) dictates that surgery should happen within 36 hours, as delay of greater than 48 hours is associated with increased morbidity and mortality. Below are suggested algorithms for the treatment of NOF.
* The priority with the young patient is to retain the femoral head if possible, even with a displaced intracapsular fracture. The risk of avascular necrosis and non-union (and therefore revision surgery) associated with internal fixation needs weighing up against the sequelae of total hip replacement in the young (wear, dislocation, revision). Discussion is necessary with the patient, on a case by case basis.
** Undisplaced fractures in the elderly can be treated with internal fixation, often with cannulated screws. This is appropriate for valgus impacted subcapital fractures which are inherently stable, to prevent secondary displacement. This does still carry the risk of AVN or non-union, and therefore a future revision. For this reason, many surgeons advocate arthroplasty as a single surgery.
*** NICE guidance - patients who fulfil these criteria should be offered total hip replacement which conveys better function and prosthetic survivorship, compared with hemiarthroplasty, but at an increased risk of dislocation.
Intertrochanteric fractures vary greatly in their stability. If the trochanter (and therefore lateral wall), and medial calcar is in tact, then the fracture configuration bears stability. This can be treated with a DHS, as collapse of the fracture is predictable. Where either or both structures are involved in the fracture, stability becomes compromised and many surgeons will favour using an intramedullary device. This is an ongoing debate, and difficult to test in an exam setting.
Post operative management
Patients should be mobilised fully weight bearing where possible. Care is multidisciplinary in its delivery. Elderly patients should have orthogeriatrician assessment of comorbidity, and bone health with secondary prevention measures if appropriate. There should be early involvement of physiotherapy and occupational therapy services. For further guidance see sources listed below.
NICE clinical guidance on hip fracture: https://www.nice.org.uk/guidance/cg124
Best Practice Tarif: www.nhfd.co.uk/20/hipfractureR…/Best%20Practice%20Tariff%20User%20Guide.pdf
National Hip Fracture Database: www.nhfd.co.uk/
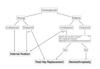
What is the commonest malignant lesion to affect the pancreas?
How do most cases of pancreatic cancer present?
What is Courvoisier’s law?
How is pancreatic cancer staged?
What tumour marker can be helpful in monitoring pancreatic cancer?
Where a potentially operable pancreatic head cancer presents with obstructive jaundice, how should this be managed?
Most pancreatic malignancies are adenocarcinomas. Whilst malignant endocrine tumours such as insulinomas and glucagonomas can occur in the pancreas, these are rare.
Most cases present as new onset epigastric pain and/ or weight loss. Lesions in the pancreatic head may present with obstructive jaundice.
Courvoisier’s law states that when the gallbladder is distended and palpable in the presence of jaundice that the underlying cause of the jaundice is unlikely to be due to gallstones. This is because gallstones, where present, often result in a degree of gallbladder wall thickening and fibrosis that precludes distension.
Pancreatic cancer is staged in a systematic and stepwise fashion. Sadly, most cases will be incurable and irresectable. Once a staging modality has demonstrated that the condition is incurable or non resectable further attempts at staging should cease. The first staging process of usually a CT scan of the chest, abdomen and pelvis. If this shows no evidence of metastatic disease or invasion of the SMA/SMV then the next step is to perform a PET/CT to look for occult distant disease that was missed by CT scanning alone. Finally, a diagnostic laparoscopy is performed to identify peritoneal disease as this can be missed by CT.
CA19-9 this stands for carbohydrate antigen 19-9. Note that this marker is not used for screening.
Potentially operable pancreatic head Ca Mx: By ERCP and insertion of a plastic stent. Metallic stents can compromise resectability and should not be used in potentially operable cases.
Pancreatic cancer
- Adenocarcinoma
- Risk factors: Smoking, diabetes, adenoma, familial adenomatous polyposis
- Mainly occur in the head of the pancreas (70%)
- Spread locally and metastasizes to the liver
- Carcinoma of the pancreas should be differentiated from other periampullary tumours with better prognosis
Clinical features
- Weight loss
- Painless jaundice
- Epigastric discomfort (pain usually due to invasion of the coeliac plexus is a late feature)
- Pancreatitis
- Trousseau’s sign: migratory superficial thrombophlebitis
Investigations
- USS: May miss small lesions
- CT Scanning (pancreatic protocol). If unresectable on CT then no further staging needed
- PET/CT for those with operable disease on CT alone
- ERCP/ MRI for bile duct assessment
- Staging laparoscopy to exclude peritoneal disease
Management
- Head of pancreas: Whipple’s resection (SE dumping and ulcers). Newer techniques include pylorus preservation and SMA/ SMV resection
- Carcinoma body and tail: poor prognosis, distal pancreatectomy, if operable
- Usually adjuvent chemotherapy for resectable disease
- ERCP and stent for jaundice and palliation
- Surgical bypass may be needed for duodenal obstruction
A 53 year old man presents with a mass lesion in the right side of the neck. On examination, it arises from the right lobe of the thyroid gland. What investigations would you perform?
Triple Assessment: Ex, Imaging, Bx
Thyroid function tests (to identify a potentially functional nodule)
USS of the thyroid
Fine needle aspiration cytology
An FNAC is reported as showing a THY 3f lesion. Imaging demonstrates a right sided nodule within the thyroid gland. What does this mean and how should it be managed?
Are there any circumstances when a core biopsy of the thyroid gland should be performed?
It means that a follicular neoplasm is present. The distinction between follicular adenoma and carcinoma is based on histological demonstration of capsular invasion and cannot be made by FNAC alone. Therefore the patient should undergo a hemithyroidectomy.
The interpretation of thyroid cytology is outlined below:
Result: Interpretation –> Action
THY 1: Inadequate –> Repeat (or follow up USS if cyst only)
THY 2: Non neoplastic (with the descriptive report documenting the features consistent with a colloid nodule or thyroiditis). Cysts may be classified as Thy2 if benign epithelial cells are present. –> Repeat USS +/- FNA at 3-6 months
THY 3 (a/f): Atypical cells (a) or follicular lesion (f) –> Hemithyroidectomy (if follicular cells)
THY 4: Suspicious of malignancy –> Surgical resection (unless lymphoma where core Bx may be considered)
THY 5: Diagnostic of malignancy –> Surgical resection (except lymphoma or if non operable)
Core biopsy if : the diagnosis is suspected as being a lymphoma, since these are best treated with chemo and or radiotherapy rather than with surgery.
What is the primary mode of metastatic spread of follicular cancers?
If the lesion were a medullary lesion what type of surveillance might you initiate?
Histologically, what are the defining features of papillary thyroid cancers?
What is the single biggest risk factor for the development of differentiated thyroid cancer?
They typically metastasise haematogenously and bone is a well recognised site. In contrast to papillary lesions, lymphatic metastases are rare.
Medullary cancers are derived from the parafollicular c cells and secrete calcitonin. This can be measured as part of follow up and be used as a marker to identify recurrent disease.
Papillary Thyr: They are associated with dystrophic calcification and psammoma bodies (which are calcium deposits) may be identified. Large empty looking nuclei are classically seen and termed “orphan Annie” nuclei. Invasion of surrounding tissue must also be present.
Differentiated thyroid cancers which include papillary and follicular lesions are the most common types of primary thyroid cancer. The greatest risk factor for the development of such lesions is radiation exposure to the thyroid gland. The earlier in life the exposure occurs, the greater the risk. There is also a clear relationship to the radiation dose. Historically, cases of thyroid cancer were noted in survivors of atomic disasters such as Chernobyl and also in children who have undergone high dose therapeutic head and neck irradiation.
Thyroid cancer is a relatively rare condition and overall will comprise approximately 1-2% of all solid tumours in a 1 year period. They are classified as being papillary, follicular, anaplastic, lymphoma and sarcomatous.
Presenting features:
- Typically presents as a discrete nodule or mass
- Lymph node or haematogenous metastasis may be present
- Locally advanced disease may invade/ compress adjacent structures with symptoms of dysphagia, dyspnoea or speech changes arising from nerve involvement
Key points in the history:
- Pattern of symptom onset
- Any association with pain (cancers are usually painless)
- Patients age (cancers most common in those aged >60 years)
- History of radiation exposure is significant as this increases the risk
- Family history of endocrine disease (MEN I/II)
Examination:
- Adequate exposure of the neck
- Assess peripheral stigmata of thyroid status (most cancers occur in euthyroid patients)
- Any overt stigmata of MEN
- Is the mass visible?
- Palpate the patient’s neck stood behind them
- Palpate the mass whilst asking the patient to swallow to determine its relationship to the thyroid
- Examine carefully for palpable neck nodes
- Attempts to elicit Pembertons sign by having the patient elevate their arms may be useful in establishing the presence of a sub sternal goitre
Diagnosis
- In all cases a USS must be performed
- Where a lesion is identified an FNAC is the usual first line management
- FNAC cannot accurately diagnose follicular lesions or lymphoma
- Staging is with chest x-ray and sometimes bone scans. Where an adverse prognosis is suspected CT scanning is usually performed.
Lesions:
- Follicular adenoma: Usually present as a solitary thyroid nodule. Malignancy can only be excluded on formal histological assessment
- Papillary carcinoma: Usually contain a mixture of papillary and colloidal filled follicles. Histologically tumour has papillary projections and pale empty nuclei. Seldom encapsulated. Lymph node metastasis predominate. Haematogenous metastasis rare. Account for 60% of thyroid cancers
- Follicular carcinoma: May appear macroscopically encapsulated, microscopically capsular invasion is seen. Without this finding the lesion is a follicular adenoma. Vascular invasion predominates. Multifocal disease rare. Account for 20% of all thyroid cancers.
- Anaplastic carcinoma: Most common in elderly females. Local invasion is a common feature. Account for 10% of thyroid cancers. Treatment is by resection where possible, palliation may be achieved through isthmusectomy and radiotherapy. Chemotherapy is ineffective.
- Medullary carcinoma: Tumours of the parafollicular cells (C Cells). C cells derived from neural crest and not thyroid tissue. Serum calcitonin levels often raised. Familial genetic disease accounts for up to 20% cases. Both lymphatic and haematogenous metastasis are recognised, nodal disease is associated with a very poor prognosis.
Management:
Lymphoma: Chemotherapy
- Anaplastic cancer: Local debulking surgery, palliative radiotherapy
- Papillary thyroid cancer: Hemithyroidectomy (T1 disease) or total thyroidectomy and central compartmental nodal dissection (T2 or greater)
- Follicular thyroid cancer: Total thyroidectomy
- Follicular adenoma: Hemithyroidectomy (the diagnosis is based on resected tissue analysis)
- Medullary thyroid cancer: Total thyroidectomy
What is the abnormality demonstrated in this 23 year old male?
When taking a history from such a patient what specific points should you focus on?
If your investigations failed to demonstrate an obvious underlying cause, what treatment options are available?

In this 23 year old male the overt abnormality demonstrated is the presence of severe, bilateral gynaecomastia.
Key features to address in Hx:
- Tempo of onset
- Drug and alcohol use
- Other co morbidities, particularly liver disease
- Testicular problems, particularly previous orchidopexy (as undescended testes have an increased risk of subsequent development of hormone secreting testicular tumours)
- Visual disturbance (pituitary tumours)
Investigation of gynaecomastia
- Clinical breast examination
- Breast USS
- Blood testing for prolactin levels, LFT’s, βHCG
- Testicular examination +/- testicular USS
If no obvious cause Mx Options include:
- Conservative management
- Tamoxifen
- Liposuction
The cosmetic outcomes following subareaolar incision and excision of the excess tissue are usually inferior to those obtained with liposuction.
Gynaecomastia describes an abnormal amount of breast tissue in males and is usually caused by an increased oestrogen:androgen ratio. It is important to differentiate the causes of galactorrhoea (due to the actions of prolactin on breast tissue) from those of gynaecomastia
Causes of gynaecomastia:
- physiological: normal in puberty
- syndromes with androgen deficiency: Kallman’s, Klinefelter’s
- testicular failure: e.g. Mumps
- liver disease
- testicular cancer e.g. Seminoma secreting HCG
- ectopic tumour secretion
- hyperthyroidism
- haemodialysis
- drugs: see below
Drug causes of gynaecomastia
- spironolactone (most common drug cause)
- cimetidine
- digoxin
- cannabis
- finasteride
- oestrogens, anabolic steroids
Very rare drug causes of gynaecomastia
- tricyclics
- isoniazid
- calcium channel blockers
- heroin
- busulfan
- methyldopa
Treatment options
- identify and manage any overt underlying cause
- liposuction provides the best cosmetic outcome
What is meant by the term acute pancreatitis?
What diagnostic modalities are most helpful in identifying an individual with acute pancreatitis?
How would you identify an individual as having a severe attack of pancreatitis?
What is the mortality associated with a mild or severe attack of pancreatitis?
What specific complications may occur in severe pancreatitis?
The term acute pancreatitis refers to the acute inflammation of the pancreas gland in which there is interstitial oedema, cellular destruction with the release of pancreatic enzymes and sometimes haemorrhage. A rise in the serum levels of pancreatic enzymes is often seen.
Where it is elevated, the serum amylase or lipase, together with a compatible history and examination findings remain sensitive. Where there is doubt a CT scan is helpful in making the diagnosis.
Pancreatitis
Both acute and chronic pancreatitis are recognised. Acute pancreatitis typically presents with relatively sudden onset of abdominal pain, coupled by a serum rise in the pancreatic enzymes. The likely underlying mechanism of injury in acute pancreatitis is premature activation of enzymes within the substance of the pancreas gland. Once cellular injury has been initiated, the inflammatory process can result in interstitial oedema, haemorrhage and ultimately, necrosis.
The typical presenting features are severe epigastric pain that radiates to the back. Nausea and vomiting occur frequently. Where the diagnosis is suspected (and it should be considered on the list of differentials of most cases of abdominal pain), a blood test for serum amylase or lipase is taken. Amylase rises sharply in the acute phase of the illness but the serum levels decline after the first 48 hours or so. A normal amylase does not, therefore, exclude the condition. Serum lipase is less prone to a false negative result as its serum levels remain elevated for longer. Where both are normal or there is diagnostic doubt, a CT scan with contrast can be useful in refining the diagnosis. Except for cases of diagnostic uncertainty, a CT scan is not usually performed in the acute phase of pancreatitis.
Severity scoring
The mortality of patients with mild pancreatitis is around 1%, this rises to between 20 and 50% for those with a severe attack. Two scoring systems in mainstream use include the Ranson and Glasgow scoring systems, a score of 3 or more factors with either system is predictive of a severe attack.
A serum CRP of >150 at 48 hours also predicts a severe attack. The obese are also at higher risk of a severe attack.
Imaging
USS in all patients
CXR in all patients
CT scanning at presentation in cases of diagnostic uncertainty. Other wise CT is performed in those with a severe attack at 7 days to identify necrosis.
Management
In mild cases this is supportive. Severe cases should be admitted to a critical care unit. Patients with gallstones pancreatitis should undergo cholecystectomy within the same admission, once recovered, or soon afterwards. Feeding is beneficial.
During a severe attack due to gallstones, there should be consideration given to early ERCP.
Where there is a severe attack and necrosis there is equipoise about the use of antibiotics.
Local complications
Acute fluid collection: Most resolve without intervention. Treat only if exerting a pressure effect
Pancreatic necrosis: Conservative management if not infected. If infection suspected, then FNA is required. If infected pancreatic necrosis is present then it can be drained percutaneously, if this fails then surgical necrosectomy may be necessary
Pancreatic abscess: Circumscribed intra abdominal collection of pus adjacent to the pancreas, managed with percutaneous drainage
Pancreatic effusion: Secondary to diaphragmatic irritation, may require drainage
Haemorrhage: From retroperitoneal vessels, may be managed using endovascular techniques
Portal or splenic vein thrombosis: Challenging to manage as anticoagulation in pancreatitis is controversial. May result in portal hypertension
Pseudocyst: Occurs 4 weeks or more after the acute attack. Those over 6cm and persist for >12 weeks and which cause symptoms may require intervention. Most pseudocysts do not require treatment. A cystogastrostomy is one option for those deemed to require intervention. There are also numerous minimally invasive options
Complications of severe pancreatitis:
- Early in the process, the complications are usually the result of systemic organ dysfunction as a result so of the inflammatory process. ARDS and renal failure are two particular risks. Haemodynamic instability also results in organ dysfunction and there is considerable microvascular hypoperfusion, capillary leak and oedema formation.
- After around a week, local complications become more prevalent, it is for this reason that patients with severe pancreatitis should undergo an abdominal CT scan at this stage. Local complications include acute fluid collections, peripancreatic abscesses, pancreatic necrosis, haemorrhage, effusions and splenic vein thrombosis.
- In the longer term, the fluid collections can reach a considerable size and the wall of the acute collection matures, after 4 weeks or more these collections are then termed pseudocysts.
Severe attack pancreatitis: It is tempting here to simply regurgitate the scoring systems (which you should know). However, it is worth taking a moment to be a little more systematic.
Identification of an individual with severe pancreatitis is based on both clinical and biochemical features. The clinical parameters that suggest a severe attack include obesity, hypoxia, haemodynamic compromise and signs of haemorrhage (Cullens and Grey Turners signs). Biochemically, either the Ranson or Glasgow scoring systems can be used. These allocated scores based on age, liver enzymes, renal function, serum glucose, serum calcium, serum LDH, albumin, oxygen saturation and the WCC. The two systems differ as to whether they count the parameter on admission or at 48 hours (e.g. LDH). Both systems define a severe attack as one which is characterised by derangement of 3 or more parameters.
In addition to the established scoring systems, a CRP >150 at 48 hours also suggests a severe attack.
Mild attacks have a mortality around 1%, severe attacks have a mortality of between 20 and 50%.

What are the disadvantages of using serum amylase levels to make a diagnosis of pancreatitis?
What are the treatment options for pancreatic necrosis?
A serum amylase that is elevated to >3 times the normal range is strongly suggestive of the diagnosis. Less marked elevations may represent alternative abdominal pathology or the fact that the acute amylase rise was missed.
Tx Pancreatic Necrosis: If there is no evidence of infection, then the correct treatment remains nutritional support via the enteral route, close monitoring and some advocate prophylactic antibiotics though there is conflicting evidence for this. If infection is suspected, the radiologically guided aspiration of the pancreas for microscopy and culture is required. If there infection associated with necrosis then this too often managed with minimally invasive techniques. If all these fail then the patient may require a surgical necrosectomy.
Pancreatitis
Both acute and chronic pancreatitis are recognised. Acute pancreatitis typically presents with relatively sudden onset of abdominal pain, coupled by a serum rise in the pancreatic enzymes. The likely underlying mechanism of injury in acute pancreatitis is premature activation of enzymes within the substance of the pancreas gland. Once cellular injury has been initiated, the inflammatory process can result in interstitial oedema, haemorrhage and ultimately, necrosis.
The typical presenting features are severe epigastric pain that radiates to the back. Nausea and vomiting occur frequently. Where the diagnosis is suspected (and it should be considered on the list of differentials of most cases of abdominal pain), a blood test for serum amylase or lipase is taken. Amylase rises sharply in the acute phase of the illness but the serum levels decline after the first 48 hours or so. A normal amylase does not, therefore, exclude the condition. Serum lipase is less prone to a false negative result as its serum levels remain elevated for longer. Where both are normal or there is diagnostic doubt, a CT scan with contrast can be useful in refining the diagnosis. Except for cases of diagnostic uncertainty, a CT scan is not usually performed in the acute phase of pancreatitis.
Severity scoring
The mortality of patients with mild pancreatitis is around 1%, this rises to between 20 and 50% for those with a severe attack. Two scoring systems in mainstream use include the Ranson and Glasgow scoring systems, a score of 3 or more factors with either system is predictive of a severe attack.
A serum CRP of >150 at 48 hours also predicts a severe attack. The obese are also at higher risk of a severe attack.
Imaging
USS in all patients
CXR in all patients
CT scanning at presentation in cases of diagnostic uncertainty. Other wise CT is performed in those with a severe attack at 7 days to identify necrosis.
Management
In mild cases this is supportive. Severe cases should be admitted to a critical care unit. Patients with gallstones pancreatitis should undergo cholecystectomy within the same admission, once recovered, or soon afterwards. Feeding is beneficial.
During a severe attack due to gallstones, there should be consideration given to early ERCP.
Where there is a severe attack and necrosis there is equipoise about the use of antibiotics.
Local complications
Acute fluid collection: Most resolve without intervention. Treat only if exerting a pressure effect
Pancreatic necrosis: Conservative management if not infected. If infection suspected, then FNA is required. If infected pancreatic necrosis is present then it can be drained percutaneously, if this fails then surgical necrosectomy may be necessary
Pancreatic abscess: Circumscribed intra abdominal collection of pus adjacent to the pancreas, managed with percutaneous drainage
Pancreatic effusion: Secondary to diaphragmatic irritation, may require drainage
Haemorrhage: From retroperitoneal vessels, may be managed using endovascular techniques
Portal or splenic vein thrombosis: Challenging to manage as anticoagulation in pancreatitis is controversial. May result in portal hypertension
Pseudocyst: Occurs 4 weeks or more after the acute attack. Those over 6cm and persist for >12 weeks and which cause symptoms may require intervention. Most pseudocysts do not require treatment. A cystogastrostomy is one option for those deemed to require intervention. There are also numerous minimally invasive options

You are involved in the treatment of a patient who is taken to theatre with a suspected perforated peptic ulcer. At operation you find some serous fluid in the abdomen and evidence of acute pancreatitis due to gallstones. The gallbladder is thin walled with a few small stones palpable within it. There is an obvious fluid collection in the lesser sac. What is the correct course of action?
The safest option is to perform a cholecystectomy and on table cholangiogram. If ductal stones are identified then these can be cleared using ERCP or transcystic CBD exploration. Open CBD exploration at the time of a laparotomy for acute pancreatitis is controversial.
Pancreatitis
Both acute and chronic pancreatitis are recognised. Acute pancreatitis typically presents with relatively sudden onset of abdominal pain, coupled by a serum rise in the pancreatic enzymes. The likely underlying mechanism of injury in acute pancreatitis is premature activation of enzymes within the substance of the pancreas gland. Once cellular injury has been initiated, the inflammatory process can result in interstitial oedema, haemorrhage and ultimately, necrosis.
The typical presenting features are severe epigastric pain that radiates to the back. Nausea and vomiting occur frequently. Where the diagnosis is suspected (and it should be considered on the list of differentials of most cases of abdominal pain), a blood test for serum amylase or lipase is taken. Amylase rises sharply in the acute phase of the illness but the serum levels decline after the first 48 hours or so. A normal amylase does not, therefore, exclude the condition. Serum lipase is less prone to a false negative result as its serum levels remain elevated for longer. Where both are normal or there is diagnostic doubt, a CT scan with contrast can be useful in refining the diagnosis. Except for cases of diagnostic uncertainty, a CT scan is not usually performed in the acute phase of pancreatitis.
Severity scoring
The mortality of patients with mild pancreatitis is around 1%, this rises to between 20 and 50% for those with a severe attack. Two scoring systems in mainstream use include the Ranson and Glasgow scoring systems, a score of 3 or more factors with either system is predictive of a severe attack.
A serum CRP of >150 at 48 hours also predicts a severe attack. The obese are also at higher risk of a severe attack.
Imaging
- USS in all patients
- CXR in all patients
- CT scanning at presentation in cases of diagnostic uncertainty. Other wise CT is performed in those with a severe attack at 7 days to identify necrosis.
Management
In mild cases this is supportive. Severe cases should be admitted to a critical care unit. Patients with gallstones pancreatitis should undergo cholecystectomy within the same admission, once recovered, or soon afterwards. Feeding is beneficial.
During a severe attack due to gallstones, there should be consideration given to early ERCP.
Where there is a severe attack and necrosis there is equipoise about the use of antibiotics.
Local complications
- Acute fluid collection: Most resolve without intervention. Treat only if exerting a pressure effect
- Pancreatic necrosis: Conservative management if not infected. If infection suspected, then FNA is required. If infected pancreatic necrosis is present then it can be drained percutaneously, if this fails then surgical necrosectomy may be necessary
- Pancreatic abscess: Circumscribed intra abdominal collection of pus adjacent to the pancreas, managed with percutaneous drainage
- Pancreatic effusion: Secondary to diaphragmatic irritation, may require drainage
- Haemorrhage: From retroperitoneal vessels, may be managed using endovascular techniques
- Portal or splenic vein thrombosis: Challenging to manage as anticoagulation in pancreatitis is controversial. May result in portal hypertension
- Pseudocyst: Occurs 4 weeks or more after the acute attack. Those over 6cm and persist for >12 weeks and which cause symptoms may require intervention. Most pseudocysts do not require treatment. A cystogastrostomy is one option for those deemed to require intervention. There are also numerous minimally invasive options

You are the CT 2 on call in general surgery. You are called to the ward by the nursing staff who are concerned about Mrs. Strong who underwent a total thyroidectomy earlier in the day as treatment for Graves disease. She is becoming increasingly distressed and irritable. On examination she is haemodynamically stable with oxygen saturations of 98% on air. Her wound is clean and dry. Outline how you will proceed.
From the history described it does not sound like the patient has developed bleeding as a source of her distress. It is therefore possible that she may be developing hypocalcaemia. The clues to this are provided by the fact that she has undergone a total thyroidectomy for Graves disease which confers the greatest risk of this complication. I would take blood tests to measure her serum calcium and obtain an ECG.
Thyroidectomy
Indications
- Thyroid gland tumours
- Symptomatic multinodular goitre
- Diagnostic uncertainty
- Hyperthyroidism
Operative work up
- Thyroid function tests
- If thyroid dysfunction then ensure cardiac work up (ECG, echocardiogram, CXR)
- If hyperthyroid then consider Lugol’s iodine to reduce vascularity of the gland
- Vocal cord check
Consent
- Indications - will require explanation
- Alternatives to surgery, mainly in the context of hyperthyroidism - medical therapy
- Generic risks, including bleeding (with risks to airway)
- Injury to parathyroid glands
- Injury to recurrent and superior laryngeal nerves (including neuropraxia)
- Outlook for thyroid function with hemi or sub total thyroidectomy
Operative technique
- General anaesthesia, endotracheal intubation
- Head in head ring, with neck extended (care in patients with cervical spine pathology), sand bag under shoulders
- Reverse Trendelenberg position
- Standard head and neck drape
- Transverse collar incision
- Platysma divided
- Strap muscles retracted
- Middle thyroid vein divided
- Superior thyroid vessels controlled by downwards traction of the gland and ligation of the vessels near to the gland capsule (to avoid injury to the superior laryngeal nerve)
- Control of inferior aspect of the gland and lift gland medially, remember the parathyroid glands and take care to preserve them
- Ligate or clip the branches of the inferior thyroid artery, the recurrent laryngeal nerve will need to be positively identified and preserved during this process
- Eventually, the gland will be tethered to the trachea by Berry’s ligament, this will require division.
- If the operation is a hemithyroidectomy then the isthmus of the gland will need to be divided and oversewn, otherwise the contralateral lobe is dealt with in an identical fashion
- Care should be taken to ensure that haemostasis is perfect, many surgeons choose to leave a drain
- The pretracheal fascia is closed and the platysma and its overlying thin fascia are approximated
- Skin is closed either with clips or sub cuticular sutures
Post operative management
- Close monitoring for bleeding or signs of respiratory compromise
- Check of serum calcium on day 1 post operatively
- Drains (if used) remove on day 1
- Over longer term, check of thyroid function annually (if hemithyroidectomy)
Her blood tests demonstrate a corrected calcium of 1.7mmol/L. Outline how you will manage this.
Why do patients who have a post operative haemorrhage following thyroid surgery develop such profound airway compromise?
I would secure intravenous access and administer intravenous calcium chloride. I would prescribe daily oral calcium and vitamin D3 supplements and arrange for daily measurements of her serum calcium levels. When she is well enough to be discharged home, I would arrange for regular calcium level checks as an outpatient since parathyroid injury is usually transient and it may be that her oral calcium supplementation can be discontinued over time.
During thyroid surgery, the closure technique involves closure of the fascial planes around the neck. As a result, post operative haematomas can develop within a confined space and result in impaired laryngeal venous return and the development of laryngeal oedma. The risks are further compounded in a patient with a degree of tracheomalacia that is sometimes seen with very large thyroid glands. As a result of the oedema, the airway is compromised. It is important to note that in the absence of tracheomalacia, the development of a haematoma does not primary lead to airway compression. It is for this reason that the immediate management consists of opening the wound to release the tension and thereby hasten the resolution of the oedema. Such patients should be promptly returned to theatre, a senior surgeon should be promptly called since failure to control the airway can result in the need for an emergency tracheostomy.
Thyroidectomy
Indications
- Thyroid gland tumours
- Symptomatic multinodular goitre
- Diagnostic uncertainty
- Hyperthyroidism
Operative work up
- Thyroid function tests
- If thyroid dysfunction then ensure cardiac work up (ECG, echocardiogram, CXR)
- If hyperthyroid then consider Lugol’s iodine to reduce vascularity of the gland
- Vocal cord check
Consent
- Indications - will require explanation
- Alternatives to surgery, mainly in the context of hyperthyroidism - medical therapy
- Generic risks, including bleeding (with risks to airway)
- Injury to parathyroid glands
- Injury to recurrent and superior laryngeal nerves (including neuropraxia)
- Outlook for thyroid function with hemi or sub total thyroidectomy
Operative technique
- General anaesthesia, endotracheal intubation
- Head in head ring, with neck extended (care in patients with cervical spine pathology), sand bag under shoulders
- Reverse Trendelenberg position
- Standard head and neck drape
- Transverse collar incision
- Platysma divided
- Strap muscles retracted
- Middle thyroid vein divided
- Superior thyroid vessels controlled by downwards traction of the gland and ligation of the vessels near to the gland capsule (to avoid injury to the superior laryngeal nerve)
- Control of inferior aspect of the gland and lift gland medially, remember the parathyroid glands and take care to preserve them
- Ligate or clip the branches of the inferior thyroid artery, the recurrent laryngeal nerve will need to be positively identified and preserved during this process
- Eventually, the gland will be tethered to the trachea by Berry’s ligament, this will require division.
- If the operation is a hemithyroidectomy then the isthmus of the gland will need to be divided and oversewn, otherwise the contralateral lobe is dealt with in an identical fashion
- Care should be taken to ensure that haemostasis is perfect, many surgeons choose to leave a drain
- The pretracheal fascia is closed and the platysma and its overlying thin fascia are approximated
- Skin is closed either with clips or sub cuticular sutures
Post operative management
- Close monitoring for bleeding or signs of respiratory compromise
- Check of serum calcium on day 1 post operatively
- Drains (if used) remove on day 1
- Over longer term, check of thyroid function annually (if hemithyroidectomy)
You are the CT1 in orthopaedic surgery and are called to the ward to review Mr. Jones who underwent insertion of an antegrade tibial intradullary nail 4 hours earlier for an tibial shaft fracture. He is complaining of post operative pain and discomfort in spite of the fact that he is usual his patient controlled analgesia system. Discuss his immediate assessment and management.
I would proceed to assessment of the patients vital signs and confirm that the patient’s PCA was in situ, with patent cannula and actually being used. I would then assess the lower limb. I would inspect the wound and check the distal neurovascular status. I would apply passive flexion to the foot and determine the effect of this manoeuvre on the patient’s discomfort. The concern in this situation is that the patient has developed a lower limb compartment syndrome.
I would therefore make arrangements to contact my senior to review the patient with a view to obtaining consent for a return to theatre for compartmental pressure measurements and performing fasciotomy is compartment syndrome was diagnosed or strongly suspected.
Compartment syndrome
This is a particular complication that may occur following fractures (or following ischaemia re-perfusion injury in vascular patients). It is characterised by raised pressure within a closed anatomical space.
The raised pressure within the compartment will eventually compromise tissue perfusion resulting in necrosis. The two main fractures carrying this complication include supracondylar fractures and tibial shaft injuries.
Symptoms and signs
- Pain, especially on movement (even passive)
- Parasthesiae
- Pallor may be present
- Arterial pulsation may still be felt as the necrosis occurs as a result of microvascular compromise
- Paralysis of the muscle group may occur
Diagnosis: measurement of intracompartmental pressure measurements. Pressures in excess of 20mmHg are abnormal and >40mmHg is diagnostic.
Treatment
- This is essentially prompt and extensive fasciotomies
- In the lower limb the deep muscles may be inadequately decompressed by the inexperienced operator when smaller incisions are performed
- Myoglobinuria may occur following fasciotomy and result in renal failure and for this reason these patients require aggressive IV fluids
- Where muscle groups are frankly necrotic at fasciotomy they should be debrided and amputation may have to be considered
- Death of muscle groups may occur within 4-6 hours
What complications may occur following compartment syndrome?
What complication has occurred?

Complications following compartment syndrome
- Muscle group death
- Renal failure
- Subsequent ischemic contractures
The patient has developed rhabdomyolysis. Due to muscle breakdown, myoglobin has entered the systemic circulation. This then filtered the glomerulus. As water is absorbed, the myglobin forms casts in the nephron that then obstruct flow. Eventually, this can result in acute tubular necrosis. The usual management is to overhydrate the patient and sometimes to administer a loop diuretic. Once renal failure is established, patients may require renal replacement therapy.
Compartment syndrome
This is a particular complication that may occur following fractures (or following ischaemia re-perfusion injury in vascular patients). It is characterised by raised pressure within a closed anatomical space.
The raised pressure within the compartment will eventually compromise tissue perfusion resulting in necrosis. The two main fractures carrying this complication include supracondylar fractures and tibial shaft injuries.
Symptoms and signs
- Pain, especially on movement (even passive)
- Parasthesiae
- Pallor may be present
- Arterial pulsation may still be felt as the necrosis occurs as a result of microvascular compromise
- Paralysis of the muscle group may occur
Diagnosis: measurement of intracompartmental pressure measurements. Pressures in excess of 20mmHg are abnormal and >40mmHg is diagnostic.
Treatment
- This is essentially prompt and extensive fasciotomies
- In the lower limb the deep muscles may be inadequately decompressed by the inexperienced operator when smaller incisions are performed
- Myoglobinuria may occur following fasciotomy and result in renal failure and for this reason these patients require aggressive IV fluids
- Where muscle groups are frankly necrotic at fasciotomy they should be debrided and amputation may have to be considered
- Death of muscle groups may occur within 4-6 hours
A 22 year old male is admitted whilst becoming injured during a game of football. His investigations include plain films of his right lower leg which are demonstrated below.
How would you assess and manage this injury?

These films demonstrate a spiral fracture of the fibula which extends inferiorly to involve the syndesmosis with injury to the malleolus. This particular fracture pattern is accorded the eponymous term of a Maisonneuve injury.
I would assess the patient carefully for other injuries and the distal neurovascular status the limb. I would carefully search for any skin breaches that could indicate open communication of the fracture. The most urgent course of action is to temporarily stabilise the fracture in a temporary incomplete cast to protect the skin overlying the malleoli which can be compromised. Having achieved this one would then need to consider the merits of conservative management in a cast versus surgical fixation. In this case, considering the age of the patient and mechanism of injury, I would generally advocate surgical fixation as it unlikely that this fracture would remain stable enough in a cast for satisfactory healing and a good functional outcome
Fracture management
Bony injury resulting in a fracture may arise from trauma (excessive forces applied to bone), stress related (repetitive low velocity injury) or pathological (abnormal bone which fractures during normal use of following minimal trauma)
Diagnosis involves not just evaluating the fracture ; such as site and type of injury but also other associated injuries and distal neurovascular deficits. This may entail not just clinical examination but radiographs of proximal and distal joints.
When assessing x-rays it is important to assess for changes in length of the bone, the angulation of the distal bone, rotational effects, presence of material such as glass.
Fracture types
- Oblique fracture: Fracture lies obliquely to long axis of bone
- Comminuted fracture >2 fragments
- Segmental fracture: More than one fracture along a bone
- Transverse fracture: Perpendicular to long axis of bone
- Spiral fracture: Severe oblique fracture with rotation along long axis of bone
Open Vs Closed
It is also important to distinguish open from closed injuries. The most common classification system for open fractures is the Gustilo and Anderson classification system :
- 1: Low energy wound <1cm
- 2: Greater than 1cm wound with moderate soft tissue damage
- 3: High energy wound > 1cm with extensive soft tissue damage
- A: Adequate soft tissue coverage
- B: Inadequate soft tissue coverage
- C: Associated arterial injury
Key points in management of fractures
- Immobilise the fracture including the proximal and distal joints
- Carefully monitor and document neurovascular status, particularly following reduction and immobilisation
- Manage infection including tetanus prophylaxis
- IV broad spectrum antibiotics for open injuries
- As a general principle all open fractures should be thoroughly debrided ( and internal fixation devices avoided or used with extreme caution)
- Open fractures constitute an emergency and should be debrided and lavaged within 6 hours of injury
In what circumstances would you consider using a Biers block?
What pre requisites must be met in order to safely proceed with a Biers block? When inflating the tourniquet, what pressure setting would you select for a typical adult male?
What local anaesthetic agents must not be used in a Biers block and why?
A Biers block provides excellent regional anaesthesia for upper limb procedures. If facilities are available it is the anaesthetic modality of choice for the manipulation of distal radius fractures.
Two medical practitioners must be present, both should have experience of administration of Biers blocks. A fully serviced tourniquet system which is free from leaks, regularly serviced and fitted with an integral pressure monitoring system must be used. An exsanguination bandage should be available.
I would inflate the tourniquet 100mmHg above the systolic blood pressure.
Bupivicaine should not be used in a Bier’s block, because it is cardiotoxic.
A 72 year old lady falls onto an outstretched hand and is brought to the emergency department. She has an obvious deformity of the distal radius with no distal neurovascular deficit. X-rays of the injury are obtained:
What abnormalities are present?
What are the management options for this type of injury?

These x-rays demonstrate evidence of a distal radius fracture, the fracture fragment is dorsally angulated. In addition there is an associated fracture of the ulnar styloid.
Mx: Having established that there is not distal neurovascular deficit, the options lie between conservative management in a cast, following reduction of the fracture using a haematoma block. In view of the avulsion of the ulnar styloid I would have a low threshold for recommending operative fixation, particularly if the post reduction images looked potentially unstable. I would also initiate treatment for osteoporosis.
Distal radius fracture
- Common, usual mechanism is fall onto an outstretched hand in elderly females with underlying osteoporosis
- Typically it is a distal radius fracture occurring about 1 inch proximal to the wrist joint with dorsal angulation of the fracture fragment. The distal end of the ulna is sometimes involved
- Management is usually conservative with reduction of the fracture under either a haematoma or Biers block and immobilisation in a cast
- Potentially unstable injuries should be managed with surgical fixation. Factors favoring instability include; dorsal tilt of more than 20 degrees, comminuted fracture, injury to the ulnar styloid, intra articular disruption
- Young patients, who typically have a higher energy mechanism of injury are usually managed surgically
- In the elderly it is important to initiate treatment for osteoporosis
A 38 year old man is undergoing emergency surgery for an incarcerated paraumbilical hernia. Anaesthetic induction includes a rapid sequence induction and then maintenance with a propofol infusion. The anaesthetic team become concerned because the patient develops profound cardiac arrhythmias and becomes pyrexial with a temperature of 40oC. What is the most likely explanation for this event?
There are two potential explanations; the first is that the paraumbilical hernia contained bowel, following administration of muscle relaxant, the perfusion to the bowel returns and this results in a re-perfusion phenomenon where toxic metabolites return to the heart. Whilst a SIRS type response may occur in conjunction with this, resulting in pyrexia, such a rapid increase in the core temperature would be unusual. The alternative and more likely explanation is that the patient has developed malignant hyperthermia.
What clinical signs would lead you to suspect that a patient had developed malignant hyperthermia?
What causes malignant hyperthermia? How is malignant hyperthermia treated?
If a patient in the surgical outpatients informs the team that they have a strong family history of malignant hyperthermia, what can be done perioperatively to reduce the risk of them developing malignant hyperthermia?
A close temporal relationship of exposure to likely precipitant drugs (suxamethonium, for example) is a key feature, onset in the post operative period is rare. Clinically, a hypercatabolic state is the typical finding, end tidal carbon dioxide production increases, there is tissue hypoxia, tacchyarrhymias, fever, muscle rigidity, acidosis and rhabdomyolysis.
In many cases it is inherited as an autosomal dominant disorder. However, it is usual asymptomatic unless exposed to an environmental trigger, these include depolarising muscle relaxants and anaesthetic gases such as halothane. On a cellular level abnormalities of calcium channels result in the uncontrolled influx of calcium into the sarcoplasmic reticulum causes sustained uncontrolled muscle contraction.
The agent Dantrolene is the only known treatment, it is a muscle relaxant that works directly on cellular receptors to prevent the release of calcium.
Because malignant hyperthermia is inherited in an autosomal dominant fashion, the presence of a strong family history should be taken seriously. The safest option is to proceed with an anaesthetic combination that does not include triggering agents, the non depolarising muscle relaxants, propofol and lignocaine are all considered safe.
Malignant hyperthermia:
- Condition seen following administration of anaesthetic agents ( rate of 1 in 15,000)
- Characterised by hyperpyrexia and muscle rigidity
- Cause by excessive release of Ca2+ from the sarcoplasmic reticulum of skeletal muscle
- Associated with defects in a gene on chromosome 19 encoding the ryanodine receptor, which controls Ca2+release from the sarcoplasmic reticulum
- Neuroleptic malignant syndrome may have a similar aetiology
Causative agents
- Halothane
- Suxamethonium
- Other drugs: antipsychotics (neuroleptic malignant syndrome)
Investigations
CK raised
Contracture tests with halothane and caffeine
Management
Dantrolene - prevents Ca2+ release from the sarcoplasmic reticulum
Please examine this persons foot.
What is the usual treatment option for this condition?

Our background which follows this section details the points to identify on foot and ankle examination.
In the examination, key points to note:
Proper introductions and hand hygiene
Inspection reveals an abnormal foot with collapsed arches, fungal nail infections and obvious loss of contour around medial malleolus. The surfaces seen, do not demonstrate any scars and the most likely explanation is ankle joint arthritis that has led to loss of contour around the ankle joint. The resultant biomechanical disruptions has most likely contributed to her flat foot.
Flat feet are typically managed conservatively, with shoe inserts being the mainstay of treatment. Ankle arthritis is often managed symptomatically, severe cases can benefit from arthroplasty or even arthrodesis. The outcomes following arthroplasty are less marked than those seen following major joint replacement.
Foot and ankle examination: The look, feel, move system should be used.
When describing the foot, it is necessary to appreciate the difference in nomenclature in describing foot motions vs foot positions. Motions of the foot are described as axes of rotation about the ankle (Y, Z and X axes) and about the foot (Y,Z and X axes).
Motions of the foot and ankle
Sagittal (X axis): Dorsiflexion, Plantar flexion
Frontal (Coronal / Z-axis): Inversion, Eversion
Transverse (Y axis): Forefoot/ midfoot, Adduction, Abduction, Ankle/ hindfoot, Internal rotation, External rotation
Triplanar motion: Supination, Adduction, Inversion, Plantar flexion, Pronation, Abduction. Eversion, Dorsiflexion
The foot positions are described differently, these include; varus, valgus, abduction, adduction and equinus.
On inspection: Examine the patient both standing and sitting. Proper exposure means being able to see the knee and below so the patient is usually wearing shorts.
With the patient standing: Look from all aspects at the symmetry of the foot, comment on obvious deformity, surgical stigmata, absent arches, foot eversion, genu valgum and intoeing.
With the patient sitting: Look for evidence of bony deformities or protrusions (exostoses) or deformity suggestive of an old fracture. Obvious deformity of the ankle joint may well be visible and could suggest old malleolar fractures.
Examine the soles of the feet for corns, callus, skin lesions or thickening to suggest plantar fasciitis
Look at the toes, comment on evidence of evidence of hallux valgus (common), bunions (common), clawing, hammer toe or signs of gouty tophi.
Palpation: Palpate the main bony prominences and comment on sites of focal tenderness, bony deformity or bursitis
Palpate the dorsalis pedis pulse (alongside the tendon of extensor hallucis longus), and posterior tibial pulses
Check sensation is normal (classically impaired in longstanding diabetes)
Move
Best undertaken with the patient sitting and you crouch or sit.
Be sure to ask about pain before moving
Grasp the heel firmly and move the foot (there is usually around 50o of plantar flexion and 15o of dorsiflexion.
Assessment of ankle ligaments - location and how to test:
- Deltoid: Medial malleolus - Attempt to evert the foot
- Lateral ligament: Palpate below the lateral malleolus - Invert the foot
- Tibiofibular ligament (inferior): Palpate anteriorly just about the joint - Dorsiflex the foot and move the talus laterally. If disrupted then the talus will displace laterally. Be careful as this manoeuvre can be painful if the joint is unstable
Then check sub talar joint inversion and eversion ; take care to eliminate tibiotalar tilt when assessing sub talar joint motion
To assess the forefoot (mid tarsal and tarsometatarsal joints); hold the heel still and grip the forefoot, there will usually be 15o of inversion and 10oof eversion.
Check the toe movements next.
Finally, ask the patient to walk. One full gait cycle from heel strike to heel strike is termed a stride. Each stride comprises a stance phase (heel strike to toe off=62% of cycle) and a swing phase (toe off to heel strike = 38% of the cycle)
Typical cases:
- Pes Planus: Common in children. In adults, the flattening of the arches is often due to degenerative changes (often secondary to obesity)
- Plantar fasciitis: Tearing of the calcaneal attachment of the plantar fascia, usually thickened and tender on examination
- Hallux Valgus: Lateral deviation of the great toe. First metatarsal head moves off the sesamoids increasing the intermetatarsal angle. Abnormal corns and callus are seen. The affected area may be tender
- Charcot foot: Marked bony deformity. Insensate foot. Foot often hyperaemic. Stigmata of arterial insufficiency may be seen. Sensation is impaired (if normal then suspect alternative diagnosis)
- Mortons neuroma: Plantar/ digital neuroma affected the plantar nerve between the 3rd and 4th metatarsal heads. Burning pain and paraesthesia of affected toes. Palpation between and just distal to the metatarsal heads produces pain. Metatarsal compression may produce a palpable click (Mulder click)
- Charcot Marie Tooth disease: Most common inherited neuropathy. Variable sensory deficit. Neuropathic arthropathy. Deformity and awkward gait present. Symmetrical elevation of the arches. Plantar flexed first ray. Hindfoot varus. Claw toes. Decreased ankle jerks. Flat foot. Marionette gait (heel toe walking)
- Anterior metatarsalgia: Pain under metatarsal heads. Foot widening is seen. Flattened medial arch (too many toes visible laterally when viewed from behind). Claw toes and callosities are seen
What is hepatocellular carcinoma?
What tumour marker is associated with hepatocellular carcinoma?
What factors increase the risk of hepatocellular carcinoma?
How is hepatocellular carcinoma diagnosed?
Is hepatocellular carcinoma a contra indication to liver transplantation?
Hepatocellular carcinoma is a tumour derived from hepatocytes. It is the commonest primary liver tumour.
It is associated with alpha feto-protein: a major plasma protein produced by the yolk sac and foetal liver during embryonic development. After birth, the liver matures and AFP production decreases. As a result, rising AFP levels can be associated with hepatocellular carcinoma.
Worldwide, the biggest risk factor for HCC is infection with hepatitis B virus. Any condition associated with chronic liver inflammation and cirrhosis increases the risks of the condition. Hepatitis C is therefore another significant risk factor. Liver adenomas are also associated with subsequent HCC development and are removed for this reason.
Where a hepatocellular carcinoma is suspected, the initial step is to measure serum AFP levels and perform a liver USS. If AFP levels are raised and USS shows a discrete lesion, then the next step is to perform a liver MRI scan. The decision to proceed with resection is generally based on imaging and AFP levels. Biopsy is not generally performed as it can precipitate tumour seeding and compromise an otherwise potentially curative resection.
No, hepatocellular carcinoma is one malignancy where transplantation is not a contra indication. Liver transplantation is a treatment option for hepatocellular cancer under specific situations where resection of the entire liver is potentially curative and the only treatment option. Such patients have to be very carefully staged and have to be fully optimised for surgery.
Hepatocellular carcinoma is the second leading cause of cancer deaths globally. Up to 750,000 cases are reported annually. Unfortunately the incidence approximates to the death rate so there are few long term survivors[1]. The disease occurs most commonly in those with chronic hepatitis and established liver cirrhosis. Therefore, these individuals should be closely screened for the development of HCC with serum AFP and liver USS every 6-12 months. Rising AFP and liver USS showing a nodule greater than 1cm in diameter makes HCC much more likely and such patients should then undergo MRI scanning.
The presence of adenomas in an otherwise healthy liver is a recognised risk factor for HCC [2, 3] and many surgeons will remove liver adenomas for this reason[4].
Diagnosis
The aim is to avoid unnecessary percutaneous biopsy. Radiologically on CT the classical feature is a suspicious lesion which is highlighted during the arterial phase with washout during the venous phase, this reflects the hypervascularity of the lesions.The risk of tumour seeding as a result of a liver biopsy is 2.7% with a median time interval between biopsy and seeding of 17 months[5].
Barcelona Clinic Liver Classification
There are many classification systems for addressing the management and prognosis, the BCLC system has the convenience of categorising disease extent with treatment and prognostic outcomes. In determining the ideal treatment modality for HCC the key points are not just disease extent, but also the functional state of the liver and patient.
In selected patients the best outcomes are achieved with surgical resection, or transplantation where surgical resection is precluded. Anatomical resections with minimum 2cm margins provide the best outcomes.
At the present time there is no evidence to recommend treatment with adjuvant chemotherapy[6].
Sorafenib
This is an oral multi tyrosine kinase inhibitor. It is the only drug that has been currently demonstrated to extend survival in individuals with advanced hepatocellular cancer[7]. The improvement in survival is from a median of 7 months to 10 months.

What type of muscle relaxants are you familiar with? What is the difference between them?
Can any muscle relaxants be reversed?
Muscle relaxants are drugs which are used to provide paralysis to facilitate surgical procedures and permit safe endotracheal intubation. Two main types are in common use; depolarising and non depolarising drugs.
Depolarising muscle relaxants of which suxamethonium is the drug is common use, work by binding to the post synaptic Ach receptor at the muscle end plate (which is then activated, albeit briefly). It is then hydrolysed quite rapidly by plasma acetylcholinesterase to allow normal return of neuromuscular function. Non depolarising muscle relaxants compete with Ach at the post synaptic receptor, they do not cause depolarisation and therefore a brief period of fasciculation is not seen following administration. They are degraded in a number of ways over a longer time frame than suxamethonium.
Non depolarising muscle relaxants can be reversed by increasing the amount of Ach present within the synaptic cleft. This is achieved by the administration of an anticholinesterase such as neostigmine. This will affect the parasympathetic nervous system too, so an antimuscarinic drug such as atropine is administered simultaneously.
These drugs work by preventing acetylcholine interacting with the post synaptic (nicotinic) receptors on the motor end plate of skeletal muscle. They are described as being either depolarising or non depolarising according to their mode of action.
Depolarising neuromuscular blocking drugs
Suxamethonium is the only commonly used drug in this category. Following injection there is a brief period of muscular fasciculation as the membrane is depolarised followed by paralysis. Recovery occurs spontaneously as the suxamethonium is hydrolysed by the enzyme plasma pseudocholinesterase. This process typically takes 4-6 minutes.
Suxamethonium has a number of important side effects which include malignant hyperpyrexia in susceptible patients, increased intra ocular pressure, prolonged apoea in those with pseudocholinesterase deficiency, a rise in serum potassium (which is most marked in burns and crush injury patients).
Pseudocholinesterase deficiency
Approximately 50 in 1000 will have slightly reduced enzyme activity and the paralysis effects may last for up to 20 minutes. In those with true and complete enzyme deficiency the apnoea can lasts for up to 2 hours, the incidence of this is <1 per 1000. Patients who display an enzyme lack will required prolonged ventillatory support and subsequently should be warned of this and the fact clearly recorded in patient notes.
Non depolarising neuromuscular blocking drugs
These drugs compete with acetylcholine and block its access at the post synaptic receptor sites on the muscle. They do not cause depolarisation. They have a slower duration of onset and a longer duration of action than suxamethonium. In many cases an anticholinesterase may be administered to hasten recovery. This results in an increase in acetylcholine at the receptor site which then competes with the paralysing drug at the receptor site. Reversal drugs are not administered until there is some evidence of returning neuromuscular function to avoid rebound paralysis following recovery from anaesthesia. An antimuscarinic drug is used concomitantly with reversal agents to avoid the parsympathetic surge that would otherwise accompany a rise in AcH levels at the parasympathetic receptors with associated bradycardia and salivation. Neostigmine is the reversal agent in common use and it is often administered with atropine or glycopyrrolate to avoid the adverse effects outline above.
When would you use a depolarising muscle relaxant? What complications of suxamethonium may occur?
Suxamethonium is most commonly used when a rapid and complete muscular paralysis is required. This is usually during induction of anaesthesia to permit safe and rapid endotracheal intubation, particularly during a rapid sequence induction.
The immediate complications that may occur following suxamethonium stem from the fact that the end plate is depolarised before paralysis occurs. As a result of widespread fasciculation, potassium is released in to the systemic circulation. In patients with severe burns or crush injuries, the potassium release may be significant enough to result in cardiac arrest.
In susceptible individuals, malignant hyperpyrexia may occur.
In a small number of patients, there may be deficiency of pseudocholinesterase, this can result in prolonged recovery from the effects of the muscle relaxant.
These drugs work by preventing acetylcholine interacting with the post synaptic (nicotinic) receptors on the motor end plate of skeletal muscle. They are described as being either depolarising or non depolarising according to their mode of action.
Depolarising neuromuscular blocking drugs
Suxamethonium is the only commonly used drug in this category. Following injection there is a brief period of muscular fasciculation as the membrane is depolarised followed by paralysis. Recovery occurs spontaneously as the suxamethonium is hydrolysed by the enzyme plasma pseudocholinesterase. This process typically takes 4-6 minutes.
Suxamethonium has a number of important side effects which include malignant hyperpyrexia in susceptible patients, increased intra ocular pressure, prolonged apoea in those with pseudocholinesterase deficiency, a rise in serum potassium (which is most marked in burns and crush injury patients).
Pseudocholinesterase deficiency
Approximately 50 in 1000 will have slightly reduced enzyme activity and the paralysis effects may last for up to 20 minutes. In those with true and complete enzyme deficiency the apnoea can lasts for up to 2 hours, the incidence of this is <1 per 1000. Patients who display an enzyme lack will required prolonged ventillatory support and subsequently should be warned of this and the fact clearly recorded in patient notes.
Non depolarising neuromuscular blocking drugs
These drugs compete with acetylcholine and block its access at the post synaptic receptor sites on the muscle. They do not cause depolarisation. They have a slower duration of onset and a longer duration of action than suxamethonium. In many cases an anticholinesterase may be administered to hasten recovery. This results in an increase in acetylcholine at the receptor site which then competes with the paralysing drug at the receptor site. Reversal drugs are not administered until there is some evidence of returning neuromuscular function to avoid rebound paralysis following recovery from anaesthesia. An antimuscarinic drug is used concomitantly with reversal agents to avoid the parsympathetic surge that would otherwise accompany a rise in AcH levels at the parasympathetic receptors with associated bradycardia and salivation. Neostigmine is the reversal agent in common use and it is often administered with atropine or glycopyrrolate to avoid the adverse effects outline above.
These drugs work by preventing acetylcholine interacting with the post synaptic (nicotinic) receptors on the motor end plate of skeletal muscle. They are described as being either depolarising or non depolarising according to their mode of action.
Depolarising neuromuscular blocking drugs
Suxamethonium is the only commonly used drug in this category. Following injection there is a brief period of muscular fasciculation as the membrane is depolarised followed by paralysis. Recovery occurs spontaneously as the suxamethonium is hydrolysed by the enzyme plasma pseudocholinesterase. This process typically takes 4-6 minutes.
Suxamethonium has a number of important side effects which include malignant hyperpyrexia in susceptible patients, increased intra ocular pressure, prolonged apoea in those with pseudocholinesterase deficiency, a rise in serum potassium (which is most marked in burns and crush injury patients).
Pseudocholinesterase deficiency
Approximately 50 in 1000 will have slightly reduced enzyme activity and the paralysis effects may last for up to 20 minutes. In those with true and complete enzyme deficiency the apnoea can lasts for up to 2 hours, the incidence of this is <1 per 1000. Patients who display an enzyme lack will required prolonged ventillatory support and subsequently should be warned of this and the fact clearly recorded in patient notes. Sugamedex reversal.
Non depolarising neuromuscular blocking drugs
These drugs compete with acetylcholine and block its access at the post synaptic receptor sites on the muscle. They do not cause depolarisation. They have a slower duration of onset and a longer duration of action than suxamethonium. In many cases an anticholinesterase may be administered to hasten recovery. This results in an increase in acetylcholine at the receptor site which then competes with the paralysing drug at the receptor site. Reversal drugs are not administered until there is some evidence of returning neuromuscular function to avoid rebound paralysis following recovery from anaesthesia. An antimuscarinic drug is used concomitantly with reversal agents to avoid the parsympathetic surge that would otherwise accompany a rise in AcH levels at the parasympathetic receptors with associated bradycardia and salivation. Neostigmine is the reversal agent in common use and it is often administered with atropine or glycopyrrolate to avoid the adverse effects outline above.
What are the normal changes to blood pressure that would be expected to occur in an otherwise well 30 year old male undergoing an open inguinal hernia repair under general anaesthesia?
Even during routine surgery, there are expected changes to blood pressure that occur. During the induction of anaesthesia, the blood pressure often falls. During the initial phase of surgery, the blood pressure rises owing to a pressor response. During the main part of the procedure the pressure then stabilises. This is followed by a rise in blood pressure during the extubation process.
Blood pressure can vary hugely in surgical patients. We consider here, two important aspects of blood pressure in the surgical patient. The risks of hypertension in the surgical patient and the normal perioperative changes in blood pressure that are seen during and following surgery.
Hypertension
Hypertension is generally diagnosed when the blood pressure is consistently recorded as being greater than or equal to 140/90mmHg. Several readings are generally taken and sometimes, ambulatory blood pressure recordings are taken in those whose diagnosis is questionable. A blood pressure of 180 mmHg systolic or 110mmHg diastolic is consistent with severe hypertension and immediate treatment is generally started.
Hypertension and it’s associated complications greatly increase the risks of surgery and where a new diagnosis of hypertension is made during pre-operative assessment, it is generally best to arrange a referral to the patients general practitioner to initiate therapy and defer surgery until this is done.
Adverse risk factors in surgical hypertensive patients
- Age >55 yr (male); >65 yr (female)
- Smoking
- Hypercholesterolaemia >6.5 mmol litre1
- Diabetes
- Family history of cardiovascular events
Evidence of target organ damage
- Left ventricular hypertrophy
- Proteinuria or elevated creatinine
- Atheroma (carotid, aorta, peripheral vessels)
- Abnormalities of retinal arteries
Cardiovascular events
- Vascular events including transient ischaemic attacks
- Ischaemic heart disease
- Congestive heart failure
- Diabetic nephropathy
- Severe hypertensive retinopathy
Peri-operative use of anti hypertensive agents
In patients with mild or moderate hypertension, chronic treatment with calcium channel blockers, ACE inhibitors, diuretics, and β-blockers does not cause exaggerated hypotensive responses to induction of anaesthesia. However, ACE inhibitors have been reported to cause hypotension if they are given on the morning of surgery, especially if large doses are used. Therefore, some authors recommend omitting the morning dose of ACE inhibitors. This practice, however, may increase the need for active management of hypertensive episodes. The need to stop therapy the day before surgery is recommended for angiotensin II receptor antagonists because of the risk of refractory hypotension.
Blood pressure and surgery
All patients undergo changes in their blood pressure during surgery performed under general anaesthesia. These are independent of any special considerations such as pre-existing cardiac disease.
Changes during surgery
- During induction: Fall in blood pressure
- Initiation of surgery: Pressor response and rise in blood pressure
- During procedure: Stabilisation of blood pressure
- During extubation and waking: Rise in blood pressure
For these reasons, routine monitoring of blood pressure during procedures is mandatory.
A number of additional factors can impact of the blood pressure of patients, both during and after surgery. These include:
- Effects of hypovolaemia
- Anaesthetic agents used
- Presence of epidural and spinal anaesthetic agents
- Use of inotropes
- Use of antihypertensive agents
- Laparoscopic surgery
How would you manage a 65 year old man who is found to have a systolic blood pressure of 160/95mmHg during pre-operative assessment for a total hip replacement?
I would repeat the measurement ensuring that a cuff of an appropriate size was used. I would take a full history from the patient to identify any associated cardiovascular risk factors and symptoms of end organ dysfunction. I would arrange for a urine test for protein, serum U+E measurement and an ECG. I would then arrange for the patient to consult with their general practitioner to consider further management of their hypertension and defer this otherwise elective procedure until this has been done.
Blood pressure can vary hugely in surgical patients. We consider here, two important aspects of blood pressure in the surgical patient. The risks of hypertension in the surgical patient and the normal perioperative changes in blood pressure that are seen during and following surgery.
Hypertension
Hypertension is generally diagnosed when the blood pressure is consistently recorded as being greater than or equal to 140/90mmHg. Several readings are generally taken and sometimes, ambulatory blood pressure recordings are taken in those whose diagnosis is questionable. A blood pressure of 180 mmHg systolic or 110mmHg diastolic is consistent with severe hypertension and immediate treatment is generally started.
Hypertension and it’s associated complications greatly increase the risks of surgery and where a new diagnosis of hypertension is made during pre-operative assessment, it is generally best to arrange a referral to the patients general practitioner to initiate therapy and defer surgery until this is done.
Adverse risk factors in surgical hypertensive patients
- Age >55 yr (male); >65 yr (female)
- Smoking
- Hypercholesterolaemia >6.5 mmol litre1
- Diabetes
- Family history of cardiovascular events
Evidence of target organ damage
- Left ventricular hypertrophy
- Proteinuria or elevated creatinine
- Atheroma (carotid, aorta, peripheral vessels)
- Abnormalities of retinal arteries
Cardiovascular events
- Vascular events including transient ischaemic attacks
- Ischaemic heart disease
- Congestive heart failure
- Diabetic nephropathy
- Severe hypertensive retinopathy
Peri-operative use of anti hypertensive agents
In patients with mild or moderate hypertension, chronic treatment with calcium channel blockers, ACE inhibitors, diuretics, and β-blockers does not cause exaggerated hypotensive responses to induction of anaesthesia. However, ACE inhibitors have been reported to cause hypotension if they are given on the morning of surgery, especially if large doses are used. Therefore, some authors recommend omitting the morning dose of ACE inhibitors. This practice, however, may increase the need for active management of hypertensive episodes. The need to stop therapy the day before surgery is recommended for angiotensin II receptor antagonists because of the risk of refractory hypotension.
Blood pressure and surgery
All patients undergo changes in their blood pressure during surgery performed under general anaesthesia. These are independent of any special considerations such as pre-existing cardiac disease.
Changes during surgery
- During induction: Fall in blood pressure
- Initiation of surgery: Pressor response and rise in blood pressure
- During procedure: Stabilisation of blood pressure
- During extubation and waking: Rise in blood pressure
For these reasons, routine monitoring of blood pressure during procedures is mandatory.
A number of additional factors can impact of the blood pressure of patients, both during and after surgery. These include:
- Effects of hypovolaemia
- Anaesthetic agents used
- Presence of epidural and spinal anaesthetic agents
- Use of inotropes
- Use of antihypertensive agents
- Laparoscopic surgery
The same 65 year old man now re-attends for his total hip replacement and has been commenced on an ACE inhibitor and diuretic for control of his hypertension. How would you manage this?
Firstly, I would ensure that the patient has a urea and electrolytes blood test performed. This is because this combination of agents is associated with a risk of renal dysfunction and electrolyte disturbance. I would discuss the patient with the anaesthetist to determine their preferences about the continuation of these agents during the peri-operative period.
Blood pressure can vary hugely in surgical patients. We consider here, two important aspects of blood pressure in the surgical patient. The risks of hypertension in the surgical patient and the normal perioperative changes in blood pressure that are seen during and following surgery.
Hypertension
Hypertension is generally diagnosed when the blood pressure is consistently recorded as being greater than or equal to 140/90mmHg. Several readings are generally taken and sometimes, ambulatory blood pressure recordings are taken in those whose diagnosis is questionable. A blood pressure of 180 mmHg systolic or 110mmHg diastolic is consistent with severe hypertension and immediate treatment is generally started.
Hypertension and it’s associated complications greatly increase the risks of surgery and where a new diagnosis of hypertension is made during pre-operative assessment, it is generally best to arrange a referral to the patients general practitioner to initiate therapy and defer surgery until this is done.
Adverse risk factors in surgical hypertensive patients
- Age >55 yr (male); >65 yr (female)
- Smoking
- Hypercholesterolaemia >6.5 mmol litre1
- Diabetes
- Family history of cardiovascular events
Evidence of target organ damage
- Left ventricular hypertrophy
- Proteinuria or elevated creatinine
- Atheroma (carotid, aorta, peripheral vessels)
- Abnormalities of retinal arteries
Cardiovascular events
- Vascular events including transient ischaemic attacks
- Ischaemic heart disease
- Congestive heart failure
- Diabetic nephropathy
- Severe hypertensive retinopathy
Peri-operative use of anti hypertensive agents
In patients with mild or moderate hypertension, chronic treatment with calcium channel blockers, ACE inhibitors, diuretics, and β-blockers does not cause exaggerated hypotensive responses to induction of anaesthesia. However, ACE inhibitors have been reported to cause hypotension if they are given on the morning of surgery, especially if large doses are used. Therefore, some authors recommend omitting the morning dose of ACE inhibitors. This practice, however, may increase the need for active management of hypertensive episodes. The need to stop therapy the day before surgery is recommended for angiotensin II receptor antagonists because of the risk of refractory hypotension.
Blood pressure and surgery
All patients undergo changes in their blood pressure during surgery performed under general anaesthesia. These are independent of any special considerations such as pre-existing cardiac disease.
Changes during surgery
- During induction: Fall in blood pressure
- Initiation of surgery: Pressor response and rise in blood pressure
- During procedure: Stabilisation of blood pressure
- During extubation and waking: Rise in blood pressure
For these reasons, routine monitoring of blood pressure during procedures is mandatory.
A number of additional factors can impact of the blood pressure of patients, both during and after surgery. These include:
- Effects of hypovolaemia
- Anaesthetic agents used
- Presence of epidural and spinal anaesthetic agents
- Use of inotropes
- Use of antihypertensive agents
- Laparoscopic surgery
What surgical factors can impact on the patients peri-operative blood pressure? Why can abdominal laparoscopic procedures cause lability of the blood pressure?
These include hypovolaemia both as a result of third space losses and as a result of bleeding, cross clamping (and unclamping of major vessels during vascular procedures), use of laparoscopic techniques and the manipulation of structures like the vagus and adrenal glands during certain procedures.
There are two main processes by which the establishment and maintenance of a pneumoperitoneum can cause derangement of blood pressure. During the creation of pneumoperitoneum, the peritoneal stretching can induce vagal discharge, bradycardia and a fall in cardiac output. Once the pneumoperitoneum is established, high pressures can impede venous return and result in a fall in cardiac output as a result of decreased pre-load.
Blood pressure can vary hugely in surgical patients. We consider here, two important aspects of blood pressure in the surgical patient. The risks of hypertension in the surgical patient and the normal perioperative changes in blood pressure that are seen during and following surgery.
Hypertension
Hypertension is generally diagnosed when the blood pressure is consistently recorded as being greater than or equal to 140/90mmHg. Several readings are generally taken and sometimes, ambulatory blood pressure recordings are taken in those whose diagnosis is questionable. A blood pressure of 180 mmHg systolic or 110mmHg diastolic is consistent with severe hypertension and immediate treatment is generally started.
Hypertension and it’s associated complications greatly increase the risks of surgery and where a new diagnosis of hypertension is made during pre-operative assessment, it is generally best to arrange a referral to the patients general practitioner to initiate therapy and defer surgery until this is done.
Adverse risk factors in surgical hypertensive patients
- Age >55 yr (male); >65 yr (female)
- Smoking
- Hypercholesterolaemia >6.5 mmol litre1
- Diabetes
- Family history of cardiovascular events
Evidence of target organ damage
- Left ventricular hypertrophy
- Proteinuria or elevated creatinine
- Atheroma (carotid, aorta, peripheral vessels)
- Abnormalities of retinal arteries
Cardiovascular events
- Vascular events including transient ischaemic attacks
- Ischaemic heart disease
- Congestive heart failure
- Diabetic nephropathy
- Severe hypertensive retinopathy
Peri-operative use of anti hypertensive agents
In patients with mild or moderate hypertension, chronic treatment with calcium channel blockers, ACE inhibitors, diuretics, and β-blockers does not cause exaggerated hypotensive responses to induction of anaesthesia. However, ACE inhibitors have been reported to cause hypotension if they are given on the morning of surgery, especially if large doses are used. Therefore, some authors recommend omitting the morning dose of ACE inhibitors. This practice, however, may increase the need for active management of hypertensive episodes. The need to stop therapy the day before surgery is recommended for angiotensin II receptor antagonists because of the risk of refractory hypotension.
Blood pressure and surgery
All patients undergo changes in their blood pressure during surgery performed under general anaesthesia. These are independent of any special considerations such as pre-existing cardiac disease.
Changes during surgery
- During induction: Fall in blood pressure
- Initiation of surgery: Pressor response and rise in blood pressure
- During procedure: Stabilisation of blood pressure
- During extubation and waking: Rise in blood pressure
For these reasons, routine monitoring of blood pressure during procedures is mandatory.
A number of additional factors can impact of the blood pressure of patients, both during and after surgery. These include:
- Effects of hypovolaemia
- Anaesthetic agents used
- Presence of epidural and spinal anaesthetic agents
- Use of inotropes
- Use of antihypertensive agents
- Laparoscopic surgery
What is meant by the term brain death? What is the natural prognosis of a patient who is declared brain dead? What conditions must be met before brain stem death testing can be considered? How are brain stem death tests performed? What is done after the second set of tests if the patient is not to become an organ donor?
Brain death refers to the complete and irreversible cessation of all functions of the entire brain including the brain stem.
Half of all patients who are declared brain dead and who continue to receive full and active treatment will succumb in 24 hours. Almost all patients will die in spite of treatment within 72 hours.
The essential precondition is that the diagnosis must confirm that the patient is in a deep and irreversible coma of known aetiology. The coma must be associated with absent responses although spinal reflexes are accepted. Reversible causes must be excluded. Therefore all narcotic drugs and muscle relaxants must be stopped. Metabolic and endocrine causes such as hypoglycaemia must be excluded with certainty. The patient must be normothermic.
- Fixed pupils which do not respond to sharp changes in the intensity of incident light
- No corneal reflex
- Absent oculo-vestibular reflexes - no eye movements following the slow injection of at least 50ml of ice-cold water into each ear in turn (the caloric test)
- No response to supraorbital pressure
- No cough reflex to bronchial stimulation or gagging response to pharyngeal stimulation
- No observed respiratory effort in response to disconnection of the ventilator for long enough (typically 5 minutes) to ensure elevation of the arterial partial pressure of carbon dioxide to at least 6.0 kPa (6.5 kPa in patients with chronic carbon dioxide retention). Adequate oxygenation is ensured by pre-oxygenation and diffusion oxygenation during the disconnection (so the brain stem respiratory centre is not challenged by the ultimate, anoxic, drive stimulus)
The test should be undertaken by two appropriately experienced doctors on two separate occasions. There is no specified time interval between the two sets of tests, However, the physiological parameters must normalise prior to the commencement of the second set of tests.
Non-organ donor: The oxygen catheter is disconnected from the endotracheal tube and cardiac activity will generally cease over the next 15 minutes. The patients relatives must be appropriately supported during this time.
Conditions for brainstem death testing
1. There must be an identifiable pathology causing irremediable brain damage. This may be intra - or extra - cranial.
- The patient must be deeply unconscious.
a. Hypothermia must be excluded as the cause of unconsciousness and the patients core temperature should be over 34oC.
b. There should be no evidence that the patients state is due to depressant drugs. This refers to narcotics, hypnotics and tranquillisers as well as neuromuscular blocking drugs. A
careful drug history is required, whilst drug levels and antagonists may need to be used.
c. Potentially reversible circulatory, metabolic and endocrine disturbances must have been
excluded as the cause of the continuing unconsciousness. Some of these disturbances may occur as a result of the condition rather than the cause and these do not preclude the diagnosis of brain stem death. - The patient must be apnoeic, needing mechanical ventilation. This condition must not be secondary to the effect of sedative drugs of neuromuscular blockade. This may require testing with a nerve stimulator to show intact neuromuscular transmission. Alternatively, demonstration of tendon reflexes can also demonstrate intact transmission
Criteria for brain death
Fixed pupils which do not respond to sharp changes in the intensity of incident light
No corneal reflex
Absent oculo-vestibular reflexes - no eye movements following the slow injection of at least 50ml of ice-cold water into each ear in turn (the caloric test)
No response to supraorbital pressure
No cough reflex to bronchial stimulation or gagging response to pharyngeal stimulation
No observed respiratory effort in response to disconnection of the ventilator for long enough (typically 5 minutes) to ensure elevation of the arterial partial pressure of carbon dioxide to at least 6.0 kPa (6.5 kPa in patients with chronic carbon dioxide retention). Adequate oxygenation is ensured by pre-oxygenation and diffusion oxygenation during the disconnection (so the brain stem respiratory centre is not challenged by the ultimate, anoxic, drive stimulus)
The test should be undertaken by two appropriately experienced doctors on two separate occasions.
Please examine this patients abdomen and comment on your findings.
Do you think that this patient has any post operative complications and if so which one?
What complications may occur with the type of stoma that this person has?

Full introduction
Clean/ gel hands
Ensure patient comfortable and not in pain
Findings
There is evidence of previous abdominal surgery with a complex midline scar and a right iliac fossa stoma. The stoma is spouted and appears to be a loop stoma with spouting of the proximal end and this is likely to be a loop ileostomy. There are marks on the skin from the surrounding stoma appliance.
There should be full palpation of the abdomen and testing of the mechanical stability of the midline wound. Comment should be made if any masses are found.
You should comment that you would conclude the examination by asking if a digital rectal examination is appropriate (remember that if it is an end stoma, the rectum may be removed!).
From the appearances of the midline wound it does not look as if the wound has healed primarily and had therefore suffered a dehisence and therefore required regular dressings until the wound had united.
The complications related to the stoma can be local and systemic, early and late. The early local complications include stoma retraction, necrosis, obstruction and separation. Later local complications include those of stoma stenosis, prolapse, para stomal hernias and skin changes. Systemic complications relate to the volume of the stoma output and the distance between stoma and DJ flexure. High output stomas can result in profound electrolyte derangement, cardiac arrhythmias, renal dysfunction and death.
Abdominal examination
Examination of the abdomen is a common station in the MRCS and depending upon the scenario you may be given an open ended instruction, e.g. “examine the abdomen” or you may be pointed to a specific area. We provide an overview. However, you need to ensure that your technique is flexible enough to adapt to the examiners instructions and that you are able to answer questions from the examiners as you proceed.
Preliminary
- Introduce yourself
- Wash hands
- Consent
- Position- Supine
- Exposure- Nipples to knees
- Q: “Do you have any pain?”
Inspection
- From end of bed
- Well or ill, level of consciousness
- Distension
- Icterus, signs of hepatic decompensation
- Obvious scars, stomas, hernias, swellings or apparent masses, bruises
- Adjuncts (fluid, oxygen, drains, catheters, NG tube)
- Movement with respiration
- Temperature, pulse, blood pressure, respiratory rate
Palpation
- Q: Are you tender anywhere?
- Superficial palpation of all quadrants for swellings, masses, tenderness
- Deep palpation of all quadrants
- Palpation of specific organs; liver, spleen, kidney, aorta.
Percussion
Percuss the abdomen, this may elicit dullness or even pain and is a proxy for rebound tenderness assessment.
Auscultation
- Bowel sounds (tinkling, silent, normal)
- Bruits (e.g. renal artery stenosis/ superficially sited grafts)
To complete examination
- Digital rectal examination
- Per vaginal examination
- Hernial orifices
- Focussed to likely differential diagnosis
Left iliac fossa mass
- Sigmoid cancer
- Ovarian cancer
- Diverticular phlegmon
- Pelvic kidney/ renal transplant
Right iliac fossa mass
- Caecal cancer
- Appendix mass
- Mesenteric cyst
- Ovarian cancer
- Massive gallbladder
- Pelvic kidney /transplant (left is more common)
Right upper quadrant mass
- Enlarged gallbladder
- Empyema (sick patient)
- Liver metastasis/ primary tumour
- Hepatomegaly
- Gastric cancer
- Pancreatic cancer
- Renal cancer
Left upper quadrant mass:
- Splenomegaly
- Gastric cancer
- Splenic flexure cancers
Groin mass/ swelling
- Lymph nodes
- Hernia
- Saphena varix
- Lipoma
Decompensated liver disease
- Jaundice
- Hepatic foetor
- Ascites
- Petichae
- Confusion
- Metabolic tremor
- Caput medusae*
- Gynaecomastia
- Splenomegaly*
*=signs of raised portal pressure
Stomas
- Site
- Number
- Loop or end
- Spouted or flat
- Nature of content
- Associated scars
- Presence of complications- hernia (common), prolapse, skin changes

Please examine this patient’s neck. How would you investigate this patient?

Marking criteria
- Introduces self
- Adequately exposes neck
- Cleans hands
- Comments on obvious inspection findings of diffuse gland enlargement and presence of obvious dominant nodule
- Clinically establishes patients thyroid status
- Accurately palpates neck and demonstrates that lump is of thyroid origin
- Clinically evaluates for retrosternal extension
- Makes adequate differential diagnosis- dominant nodule within multinodular goitre
TRIPLE ASSESSMENT: I would arrange for an ultrasound of the thyroid gland and fine needle aspiration cytology of the dominant nodule. I would also check the patients thyroid function tests.
Thyroid gland - examination
The usual MRCS thyroid scenarios include examining a patient with an actual or suspected thyroid mass. Examination can be divided into two components, which should be assessed concurrently, these are examination of the gland itself and clinical determination of the patient’s thyroid status.
Preliminary:
- Introduce yourself
- Wash hands
- Consent
- Position- Sitting
- Exposure- Neck and upper chest
- Q: “Are you comfortable?”
Inspection
- Gland
- Swelling (midline or lateral)
- Distended neck veins
- Scars
- Contour of neck
Thyroid status:
- Restless/ agitated*
- Thin/ emaciated*
- Thyroid acropachy*
- Thyroid dermopathy (c.f. pre tibial myxoedema)*
- Eye signs (lid lag>exopthalmos>chemosis)*
- Peaches and cream complexion**
- Lethargic**
*=Hyperthyroid/ Graves disease
**=Hypothyroid
Palpation
- Hands: Acropachy, Palmar erythema, Tachy/ bradycardia, Resting tremor
Neck
- Full examination of the neck palpate both sides
- If swelling is evident determine whether it is discrete or diffuse or dominant nodule in multinodular goitre
- If swelling is present, stand behind the patient and palpate the lump again, a glass of water will nearly always be available, ask the patient to take a mouthful and then swallow on your command, establish that the mass moves upwards on swallowing
- Ask the patient to protrude their tongue, thyroglossal cysts (midline lesion) are elevated by this manoeuvre
- Examine the lymph node chains
Percussion
- Percuss the lower border the neck and upper chest (to check for retrosternal extension)
Auscultation
- Auscultate the gland (bruit may be heard)
To complete examination
- Perform Pembertons manoeuvre (ask patient to raise their arms), monitor carefully for signs of facial congestion and stop immediately if these are apparent, distension of neck veins occurs early
- If there are overt signs of thyroid dysfunction then suggest that you would wish to perform a full cardiovascular system examination to establish if there are any signs of cardiac failure
Be prepared for the examiners to interrupt you as you progress through the examination and they may direct you other areas.
Further investigations
- USS to identify focal abnormalities
- FNAC of palpable lesions
- Measurement of thyroid hormones

Please examine this patient with a lump in their neck. How would you investigate this patient?

Marking criteria
- Full introduction and sets patient at ease
- Cleans hands
- Positions patient appropriately
- Carefully inspects patient from front and back of face and comments on obvious mass lesion at the angle of the left side of the mandible
- Inspects the interior aspect of the oral cavity and looks for evidence of poor dentition and pharyngeal extension of the mass
- Palpates the mass and comments on consistency
- Palpates regional lymph nodes
- Tests facial nerve function
Produces likely list of differential diagnoses:
- In absence of facial nerve weakness, likely to represent pleomorphic adenoma
TRIPLE ASSESSMENT: I would arrange an ultrasound of the head and neck together with fine needle aspiration cytology.
Parotid gland - examination
Parotid gland masses may be either benign or malignant and are generally readily assessable.
Preliminary
- Introduce yourself
- Wash hands
- Consent
- Position- Sitting
- Exposure- Head and neck exposed, hair swept back
- Q: “Do you have any pain?”
Inspection
- From front and side
- Well or ill (infection vs tumour)
- Obvious distortion around the angle of the mandible
- Evidence of facial nerve impairment
- Look very carefully for scars, the incision for parotid surgery lies posterior to the angle of the mandible and be very easy to miss
- Inspect the oral cavity with pen torch to assess for pharyngeal extension of deep lobe mass
- Is there discharge from parotid duct
Palpation
- Q: Are you tender anywhere?
- Superficial palpation of mass, most parotid lesions be they malignant or benign will be firm
- Bimanual palpation via the oral cavity may be required
- Carefully palpate all lymph node chains
To complete examination
- Formal facial nerve testing
Further investigation
- USS and FNAC of all lesions is usual initial management
Please examine this patients breasts,
Why may this patient have impaired sensation in her axilla?
Why is it useful to assess the function of the thoracodorsal nerve?
What are the indications for performing a mastectomy in the treatment of breast cancer?

Marking criteria
- Fully introduces self and offers chaperone
- Cleans hands
- Positions patient
- Comments of obvious right sided mastectomy with normal left breast
- Palpates normal breast and axilla in systematic fashion
- Palpates operated breast, checks axilla and carefully feels for local recurrence
- Checks for function of long thoracic nerve and thoracodorsal nerve
- Palpates supra clavicular fossa
- Offers to perform systematic examination to assess for metastatic disease
- Sensory disturbance axilla: During axillary nodal clearance, the intercostobrachial nerves are often injured or divided. This results in sensory disruption to the axillary skin.
- Thoracodorsal nerve assessment: If reconstruction of the breast with a latissimus dorsi pedicled flap were being contemplated, impairment of this nerve is a risk factor for atrophy of this muscle which may compromise the muscle bulk and subsequent prosthesis coverage.
Mastectomy:
- Patient choice
- Large tumour whose removal would result in poor cosmesis with a conservation approach
- Multifocal lesions
- Lobular cancers (unless small)
Breast examination
Breast examination can occur more frequently than candidates may appreciate. Patients who have undergone breast surgery are common, easy to recruit and findings reproducible as large numbers can be available.
Preliminary
- Full introduction
- Ask permission to examine breasts and offer a chaperone
- Clean hands
- Position patient: Semi recumbent on couch
- Exposure: Neck, chest and abdomen should all be visible
- Q: “Are you in any pain, comfortable and happy for me to proceed? Let me know at any point if you feel uncomfortable”
Inspection
- Make a very careful assessment from the front with arms flat and with arms raised.
- Look carefully for breast asymmetry, skin changes, obvious swellings, nipple changes, tattoo from radiotherapy, surgical scars (both breast and axilla), stigmata of radiotherapy, evidence of reconstruction.
Nipple changes:
- Nipple retraction
- Nipple discharge
- Nipple eczema/ Paget type changes
Inspection pitfalls
- Look really carefully for scars, circumareaolar incisions may be very easy to miss
- Failing to comment on distortion that occurs with arms raised and suggests pectoral involvement with mass lesions
- Identifying sentinel node scars, these are small and hidden deep within axilla
- Scars from reconstructive surgery (latissimus dorsi flap scar is posterior), TRAM flap scars are at the base of the abdomen and may be hidden by underwear
Palpation
- Always palpate both breasts, start with the normal side
- Palpate all quadrants sequentially using the flat of the fingers to appreciate pathology
- For any lump comment on it’s consistency, mobility and fixation
- Palpate the axilla, supporting the arm
- Finally palpate the clavicular fossa (nodes here are classified as M1 disease)
Other areas to examine
- If a lesion is suspected as being malignant examine the chest for effusions, the abdomen for hepatomegaly and percuss the vertebral column for bony tenderness (axial skeleton commonest site for bony metastatic disease
- If evidence of previous breast surgery, comment on site of incision and nature of surgery. If the procedure was a wide local excision for cancer look for the radiotherapy tattoos as adjuvent radiotherapy is nearly always given following WLE for malignant disease
- Advanced cancers (rare in an OSCE!) may show skin changes of Peu d’orange as a result of lymphatic occlusion
- When examining the axilla check cutaneous sensation, division of the intercostobrachial nerves during an axillary nodal clearance can impair sensation in this area
- Check for long thoracic nerve and thoracodorsal nerve injury by testing serratus anterior and latissimus dorsi function
Further investigation
- Imaging with USS (all cases) and mammography (all post menopausal women)
- Image guided core biopsy of lesion
A 56 year old man was admitted with acute pancreatitis and 48 hours following admission is found to have a temperature of 38 degrees centigrade and a pulse rate of 105. He is not hypoxic and has a respiratory rate of 18. What is the most likely differential diagnosis?
At 48 hours following presentation, infected necrosis would be relatively unlikely. The normal respiratory parameters would go against ARDS. The most likely event at this stage is therefore systemic inflammatory response syndrome.
What is systemic inflammatory response syndrome? How is it treated? What is the difference between SIRS and sepsis? How is sepsis treated? What sources of sepsis are present in the ITU patient?
It is a clinical response to a non specific insult of either infective or non infective origin. It is characterised by the following physiological parameters; fever of greater than 38 degrees or temperature less than 36 degrees. A pulse rate of greater than 90, a respiratory rate of more than 20 breaths per minute and a WCC of greater than 12. It is caused by a generalised inflammatory response that is predominantly cytokine mediated.
Cause
There are many different factors that can initiate SIRS these range from bacterial infection, through to major surgery and trauma. Because of the complex nature of the immunological pathogenesis of SIRS the response of individuals to the same stimulus can vary hugely. Where haemodynamic instability accompanies a proven microbial infection the correct term is sepsis rather than SIRS.
SIRS
- Temperature more than 380 C or less than 36 0 C
- HR >90
- RR >20 or Pa CO2 less than 32 mmHg
- WCC >12
SIRS itself does not require treatment and this is predominantly supportive. Treatment is directed at the underlying cause. Treatment is, however, given to try and minimise further complications and these include prophylaxis against stress ulcer, DVT prophylaxis, correction of electrolyte abnormalities and close monitoring of cardiac, renal and respiratory function.
Management
Individuals developing SIRS are usually managed in a critical care environment. Many will require invasive monitoring and haemodynamic support. The underlying initiating stimulus should be correctly managed. Early attention should be paid to the patients nutritional state since SIRS can be profoundly catabolic. Where there are no contra indications, patients should be enterally fed. Even non nutritative feeding can be beneficial as it reduces the incidence of intestinal bacterial translocation.
Thromboprophylaxis should be instituted and since these patients are prone to stress peptic ulcers, proton pump inhibitors should be administered.
Sepsis is characterised by haemodynamic disturbance in the form of hypotension in the absence of other causes of hypotension in the presence of likely or proven infective source. SIRS itself does not specify a specific source and thus, in the presence of infection with hypotension the correct terminology is sepsis and not SIRS.
Prognosis
This depends upon the patients underlying physiological reserve and the cause. Where SIRS occurs without associated infection the 28 day mortality is of the order of 2%. This rises to 28% in those who have septic shock.
The treatment of sepsis is embodied in the principles of the surviving sepsis campaign and the use of sepsis bundles that specify specific treatment targets. These include attempting to identify a cause by liberal use of culture including blood and other bodily fluids prior to administration of antibiotics. Haemodynamic support with use of IV fluids and vasopressors may also be needed. By adopting the principles of the surviving sepsis campaign it is hoped that mortality with sepsis may be reduced by up to 25%. SEPSIS 6
ITU provides excellent support for critically ill patients. However, the use of invasive monitoring and ventillatory devices all provide conduits for the entry of bacteria. Because of the nature of patients on ITU and the widespread use of antibiotics, the organisms encountered are often unusual or resistant to standard treatments. Therefore the use of all invasive devices from catheters to monitoring lines should be regularly reviewed, removed when no longer needed or changed if there is any suspicion of infection.
- What is meant by the term abdominal compartment syndrome?
- What are the main risk factors for the development of abdominal compartment syndrome?
- How would you diagnose suspected abdominal compartment syndrome?
- How would you manage abdominal compartment syndrome?
Abdominal compartment syndrome is a sustained increase in intra abdominal pressure >20mmHg resulting in tissue hypoperfusion and end organ dysfunction.
The main risk factors are long complex abdominal operations with extensive tissue handling. Tissue hypoxia and subsequent reperfusion injury greatly increases risk. So too, does complex abdominal closure techniques, such as those which may follow incisional hernia closure where the functional size of the abdominal cavity is reduced.
Diagnosis requires measurement of intra abdominal pressure. This is usually achieved by placing an intravesical pressure transducer transurethrally. The intravesical pressure is taken as being representative of intra abdominal pressure. The diagnosis is generally made where the pressure exceeds 20mmHg and there is evidence of end organ dysfunction.
Mx: I would carefully assess the patient. If they are not in a critical care environment then I would arrange for the patient to be transferred to such an environment and I would inform senior members of the surgical team in the decision making process. In the first instance, if the patient is relatively stable, I would institute some non operative interventions, these include; insertion of NG tube, placement of urinary catheter and abdominal imaging to identify any collections which may be drained percutaneously. Finally, if the patient is unstable, or conservative management does not improve the situation then the patient could be taken to theatre and a laparostomy constructed using a Bogota bag or abdominal VAC system.
Abdominal compartment syndrome
Background
- Intra-abdominal pressure is the steady state pressure concealed within the abdominal cavity.
- In critically ill adults the normal intra abdominal pressure = 5-7mmHg
- Intra abdominal hypertension has pressures of 12-25mmHg
- Changes >15mmHg are associated with microvascular hypoperfusion
- Abdominal compartment syndrome is defined as sustained intra abdominal pressure >20mmHg coupled with new organ dysfunction / failure
- It may occur either primarily without previous surgical intervention e.g. Following intestinal ischaemia or secondarily following a surgical procedure
- Diagnosis is typically made by transvesical pressure measurements coupled with an index of clinical suspicion.
Management
Once the diagnosis is made non operative measures should be instituted including:
- Gastric decompression
- Improve abdominal wall compliance e.g. muscle relaxants/ sedation
- Drain abdominal fluid collections.
- Consider fluid restriction/ diuretics if clinically indicated.
In those whom non operative treatment is failing; the correct treatment is laparotomy and laparostomy. Options for laparostomy are many although the Bogota bag or VAC techniques are the most widely practised. Re-look laparotomy and attempts at delayed closure will follow in due course.
- How is calcium transported in the body?
- What hormones are involved in calcium homeostasis?
- Under normal circumstances, how do the kidneys process calcium and phosphate?
Calcium exists in three main states in the body, protein bound, complexed and ionised. Physiologically, it is the ionised calcium that is biologically active.
Two hormones are involved in calcium homeostasis, these include calcitonin which is released by the medullary cells of the thyroid gland and parathyroid hormone (PTH) which is released from the parathyroid glands. The former is responsible for lowering serum calcium levels and it’s release is triggered by high serum calcium levels. PTH is released when serum calcium levels are low.
Calcium and phosphate ions are freely filtered at the glomerulus. From there, the majority (65%) of calcium ions exit the proximal convoluted tubule passively, by diffusion. A further 30-35% is actively filtered in the distal convoluted tubule. Roughly 2% of all filtered calcium is excreted.
Phosphate ions generally leave in the proximal convoluted tubule via active transport (80%), a further 10% leaves in the distal convoluted tubule by diffusion. Approximately 10% of filtered phosphate ions will be excreted. This high figure reflects the fact that the human diet is generally phosphate rich.
Calcium homeostasis
Calcium ions are linked to a wide range of physiological processes. The largest store of bodily calcium is contained within the skeleton. Calcium levels are primarily controlled by parathyroid hormone, vitamin D and calcitonin.
Hormonal regulation of calcium
Parathyroid hormone (PTH):
- Increase calcium levels and decrease phosphate levels
- Increases bone resorption
- Immediate action on osteoblasts to increase ca2+ in extracellular fluid
- Osteoblasts produce a protein signaling molecule that activate osteoclasts which cause bone resorption
- Increases renal tubular reabsorption of calcium
- Increases synthesis of 1,25(OH)2D (active form of vitamin D) in the kidney which increases bowel absorption of Ca2+
- Decreases renal phosphate reabsorption
1,25-dihydroxycholecalciferol (the active form of vitamin D):
- Increases plasma calcium and plasma phosphate
- Increases renal tubular reabsorption and gut absorption of calcium
- Increases osteoclastic activity at high levels and osteoblasts at low levels
- Increases renal phosphate reabsorption
Calcitonin
- Secreted by C cells of thyroid
- Inhibits intestinal calcium absorption
- Inhibits osteoclast activity
- Inhibits renal tubular absorption of calcium
Both growth hormone and thyroxine also play a small role in calcium metabolism.
What are main processes involved in electrical activity within the heart?
What is meant by the term cardiac output and what factors affect it?
What is Starlings law of the Heart?
What effect, if any, do pericardial effusions have on cardiac output?
All cardiac myocytes have a cellular membrane that has a degree of electrochemical instability. Therefore all are capable of spontaneous depolarisation and cation flux across the membranes occurs at all times. However, the rate at which this occurs varies according to cell type. Therefore, in the sino atrial node, the usual pattern of activity is for a gradual depolarisation from -70mV to -50mV occurs. At this point there is full depolarisation and this then generates an electrical impulse that is transmitted to the AV node and then into the ventricles.
The term cardiac output refers to the amount of blood ejected by the left ventricle per minute and it is the product of the heart rate and stroke volume. It is therefore primarily affected by adjustments affecting these two parameters. To an extent, changes in heart rate can be accommodated by changes to stroke volume such that the overall output is kept constant. However, marked changes in heart rate in non conditioned individuals can result in impaired ventricular filling, a fall in end diastolic volume and therefore a fall in stroke volume overall with subsequent decrease in cardiac output.
Cardiac output is also affected by the afterload, this refers to aortic resting pressure. Aortic pressure is important because it determines the perfusion pressure of the myocardium.
The Frank Starling Law states that if all other factors are constant, increases in the end diastolic volume will result in an increase in stroke volume and thus cardiac output. This statement holds true, up to a point, beyond which, the increase in end diastolic volume exceeds the ventricular capacity to effectively contract and therefore, paradoxically, cardiac output declines.
Peri-cardial effision: A small amount of fluid is usually present in the pericardial sac and this has the effect of providing lubrication. However, excessive amounts of fluid in the pericardium can compress the heart because the pericardial fibrous tissue in not distensible - decreasing preload/increasing afterload. As a result the end diastolic volume will decrease and cardiac output will decline.
Cardiac physiology:
- The heart has four chambers ejecting blood into both low pressure and high pressure systems.
- The pumps generate pressures of between 0-25mmHg on the right side and 0-120 mmHg on the left.
- At rest diastole comprises 2/3 of the cardiac cycle.
- The product of the frequency of heart rate and stroke volume combine to give the cardiac output which is typically 5-6L per minute.
Detailed descriptions of the various waveforms are often not a feature of MRCS A (although they are on the syllabus). However, they are a very popular topic for surgical physiology in the MRCS B exam.
Electrical properties
- Intrinsic myogenic rhythm within cardiac myocytes means that even the denervated heart is capable of contraction.
- In the normal situation the cardiac impulse is generated in the sino atrial node in the right atrium and conveyed to the ventricles via the atrioventricular node.
- The sino atrial node is also capable of spontaneous discharge and in the absence of background vagal tone will typically discharge around 100x per minute. Hence the higher resting heart rate found in cardiac transplant cases. In the SA and AV nodes the resting membrane potential is lower than in surrounding cardiac cells and will slowly depolarise from -70mV to around -50mV at which point an action potential is generated.
- Differences in the depolarisation slopes between SA and AV nodes help to explain why the SA node will depolarise first. The cells have a refractory period during which they cannot be re-stimulated and this period allows for adequate ventricular filling. In pathological tachycardic states this time period is overridden and inadequate ventricular filling may then occur, cardiac output falls and syncope may ensue.
Parasympathetic fibres project to the heart via the vagus and will release acetylcholine. Sympathetic fibres release nor adrenaline and circulating adrenaline comes from the adrenal medulla. Noradrenaline binds to β 1 receptors in the SA node and increases the rate of pacemaker potential depolarisation.
Cardiac cycle
- Mid diastole: AV valves open. Ventricles hold 80% of final volume. Outflow valves shut. Aortic pressure is high.
- Late diastole: Atria contract. Ventricles receive 20% to complete filling. Typical end diastolic volume 130-160ml.
- Early systole: AV valves shut. Ventricular pressure rises. Isovolumetric ventricular contraction. AV Valves bulge into atria (c-wave). Aortic and pulmonary pressure exceeded- blood is ejected. Shortening of ventricles pulls atria downwards and drops intra atrial pressure (x-descent).
- Late systole: Ventricular muscles relax and ventricular pressures drop. Although ventricular pressure drops the aortic pressure remains constant owing to peripheral vascular resistance and elastic property of the aorta. Brief period of retrograde flow that occurs in aortic recoil shuts the aortic valve. Ventricles will contain 60ml end systolic volume. The average stroke volume is 70ml (i.e. Volume ejected).
- Early diastole: All valves are closed. Isovolumetric ventricular relaxation occurs. Pressure wave associated with closure of the aortic valve increases aortic pressure. The pressure dip before this rise can be seen on arterial waveforms and is called the incisura. During systole the atrial pressure increases such that it is now above zero (v- wave). Eventually atrial pressure exceed ventricular pressure and AV valves open - atria empty passively into ventricles and atrial pressure falls (y -descent )
The negative atrial pressures are of clinical importance as they can allow air embolization to occur if the neck veins are exposed to air. This patient positioning is important in head and neck surgery to avoid this occurrence if veins are inadvertently cut, or during CVP line insertion.
Mechanical properties
- Preload = end diastolic volume
- Afterload = aortic pressure
It is important to understand the principles of Laplace’s law in surgery.
- It states that for hollow organs with a circular cross section, the total circumferential wall tension depends upon the circumference of the wall, multiplied by the thickness of the wall and on the wall tension.
- The total luminal pressure depends upon the cross sectional area of the lumen and the transmural pressure. Transmural pressure is the internal pressure minus external pressure and at equilibrium the total pressure must counterbalance each other.
- In terms of cardiac physiology the law explains that the rise in ventricular pressure that occurs during the ejection phase is due to physical change in heart size. It also explains why a dilated diseased heart will have impaired systolic function.
Starlings law
- Increase in end diastolic volume will produce larger stroke volume.
- This occurs up to a point beyond which cardiac fibres are excessively stretched and stroke volume will fall once more. It is important for the regulation of cardiac output in cardiac transplant patients who need to increase their cardiac output.
Baroreceptor reflexes
- Baroreceptors located in aortic arch and carotid sinus.
- Aortic baroreceptor impulses travel via the vagus and from the carotid via the glossopharyngeal nerve.
- They are stimulated by arterial stretch.
- Even at normal blood pressures they are tonically active.
- Increase in baroreceptor discharge causes:
*Increased parasympathetic discharge to the SA node.
*Decreased sympathetic discharge to ventricular muscle causing decreased contractility and fall in stroke volume.
*Decreased sympathetic discharge to venous system causing increased compliance.
*Decreased peripheral arterial vascular resistance
Atrial stretch receptors
- Located in atria at junction between pulmonary veins and vena cava.
- Stimulated by atrial stretch and are thus low pressure sensors.
- Increased blood volume will cause increased parasympathetic activity.
- Very rapid infusion of blood will result in increase in heart rate mediated via atrial receptors: the Bainbridge reflex.
- Decreases in receptor stimulation results in increased sympathetic activity this will decrease renal blood flow-decreases GFR-decreases urinary sodium excretion-renin secretion by juxtaglomerular apparatus-Increase in angiotensin II.
- Increased atrial stretch will also result in increased release of atrial natriuretic peptide.

What do you understand by the term hypovolaemia?
What types of hypovolaemia are you familiar with?
How would you manage a patient with suspected hypovolaemia?
Normally, the body has a circulating volume that comprises plasma, erythrocytes and other cells and water. Loss of any of these components can result in hypovolaemia.
Hypovolaemia may be overt or covert, compensated or uncompensated. Uncompensated hypovolaemia is characterised by haemodynamic disturbance and is therefore referred to as shock. In surgical practice, most hypovolaemia is covert and compensated and typically occurs as a result of intra operative fluid losses through transpiration. Because the splancnic circulation can vasoconstrict, it is possible for a degree of autotransfusion to occur to compensate for these changes. Overt hypovolaemia in surgical patients usually manifests as changes to physiological parameters that are monitored such as urine output or a visible losses, such as blood, in surgical drains.
I would fully assess the patient and determine acute parameters such as airway, breathing and circulation. I would be keen to ascertain, at the outset, the degree of haemodynamic compromise present. I would inspect any indwelling drains and catheters. Finally, I would test skin turgor and capillary return. Having established the cause, extent and degree of hypovolaemia I would then be in a position to determine treatment. This may range from simple volume replacement the rate and volume of which would be titrated to estimated and ongoing losses through to return to theatre for control of bleeding. In the event that simple interventions were either not indicated or successful I would seek senior surgical and anaesthetic input.
ypovolaemia and the surgical patient
Hypovolaemia often represents the end point of multiple pathological processes. It may be divided into the following categories; overt compensated hypovolaemia, covert compensated hypovolaemia and decompensated hypovolaemia. Of these three categories the covert compensated subtype of hypovolaemia remains the commonest and is accounted for by the fact that class I shock will often produce no overtly discernible clinical signs. This is due, in most cases, to a degree of splanchnic autotransfusion. The most useful diagnostic test for detection of covert compensated hypovolaemia remains urinanalysis. This often shows increased urinary osmolality and decreased sodium concentration.
In overt compensated hypovolaemia the blood pressure is maintained although other haemodynamic parameters may be affected. This correlates to class II shock. In most cases assessment can be determined clinically. Where underlying cardiopulmonary disease may be present the placement of a CVP line may guide fluid resuscitation. Severe pulmonary disease may produce discrepancies between right and left atrial filling pressures. This problem was traditionally overcome through the use of Swann-Ganz catheters.
Untreated, hypovolaemia may ultimately become uncompensated with resultant end organ dysfunction. Microvascular hypoperfusion may result in acidosis with a subsequent myocardial depressive effect, thereby producing a vicious circle.
The treatment of hypovolaemia is with intravenous fluids. In the first instance a fluid challenge such as the rapid infusion of 250ml of crystalloid will often serve as both a diagnostic and resuscitative measure. In the event that this fails to produce the desired response the patient will need to be re-evaluated clinically. More fluid may be needed. However, it is important not to overlook mechanical ureteric obstruction in the anuric, normotensive patient.
What factors control the rate of gastric emptying?
What surgical procedures have the greatest impact on gastric emptying?
What agents are useful in increasing the rate of gastric emptying?
Gastric motility is controlled by three main factors, the nature of gastric contents, vagal inputs and local endocrine factors. The nature of food consumed has a direct bearing on gastric motility, liquids pass through the pylorus faster than solids. In the latter group those foodstuffs such as carbohydrates that are already part disgested pass more rapidly than fats and proteins that are relatively undigested. The main controlling factor in gastric emptying is the vagal inputs. The stomach is primarily under the control of the parasympathetic nervous system and two vagal nerves pass down and branch over the stomach. Vagal activity increases gastric activity and thus emptying. Finally, hormonal inputs also have a direct local effect. Gastrin tends to increase gastric activity. In contrast, CCK and gastric inhibitory peptide will tend to decrease gastric emptying. These hormonal signals have a direct overlap with the foodstuffs consumed since these will directly affect CCK release, for example.
The most potent impact on gastric emptying occurred following truncal vagotomy which is a operation that was performed for peptic ulcer disease in the era before acid lowering agents were available. The effects of this procedure were so significant that a procedure to facilitate gastric emptying was always performed in association. Other procedures that impact on gastric emptying include the method of reconstruction following distal gastric resection. A number of options are available, these include Roux en Y reconstruction (best function) through to anterior gastro-enterostomy (worst function). Pancreatic resections of the head of the gland also require some form of gastric reconstruction. The exceptions to are the newer pylorus preserving Whipples procedure, though emptying complications can occur with this procedure too.
One of the best agents was a drug called cisapride. However, this was withdrawn as a result of cardiac side effects. The dopaminergic drug metoclopramide increases both gastric and oesophageal motility and its effects are vagally mediated. The drug domperidone has similar effects. Neither agent is useful in cases of diabetic autonomic gastropathy since the neuronal inputs are, by definition, compromised. In these cases the antibiotic erythromycin is used, its has potent effects at increasing gastric emptying and its effects are not vagally mediated. However, the resulting diarrhoea can impede its use.
Gastric emptying
The stomach serves both a mechanical and immunological function. Solid and liquid are retained in the stomach during which time repeated peristaltic activity against a closed pyloric sphincter will cause fragmentation of food bolus material. Contact with gastric acid will help to neutralise any pathogens present.
The amount of time material spends in the stomach is related to its composition and volume. For example a glass of water will empty more quickly than a large meal. The presence of amino acids and fat will all serve to delay gastric emptying.
Controlling factors
Neuronal stimulation of the stomach is mediated via the vagus and the parasympathetic nervous system will tend to favor an increase in gastric motility. It is for this reason that individuals who have undergone truncal vagotomy will tend to routinely require either a pyloroplasty or gastro-enterostomy as they would otherwise have delayed gastric emptying.
The following hormonal factors are all involved:
- Delay emptying: Gastric inhibitory peptide, Cholecystokinin, Enteroglucagon
- Increase emptying: Gastrin
Diseases affecting gastric emptying
All diseases that affect gastric emptying may result in bacterial overgrowth, retained food and eventually the formation of bezoars that may occlude the pylorus and make gastric emptying even worse. Fermentation of food may cause dyspepsia, reflux and foul smelling belches of gas.
Iatrogenic
Gastric surgery can have profound effects on gastric emptying. As stated above any procedure that disrupts the vagus can cause delayed emptying. Whilst this is particularly true of vagotomy, this operation is now rarely performed. Surgeons are divided on the importance of vagal disruption that occurs during an oesophagectomy, some will routinely perform a pyloroplasty and others will not.
When a distal gastrectomy is performed, the type of anastomosis performed will impact on emptying. When a gastro-enterostomy is constructed, a posterior, retrocolic gastroenterostomy will empty better than an anterior one.
Diabetic gastroparesis
This is predominantly due to neuropathy affecting the vagus nerve. The stomach empties poorly and patients may have episodes of repeated and protracted vomiting. Diagnosis is made by upper GI endoscopy and contrast studies, in some cases a radio nucleotide scan is needed to demonstrate the abnormality more clearly. In treating these conditions, drugs such as metoclopramide will be less effective as they exert their effect via the vagus nerve. One of the few prokinetic drugs that do not work in this way is the antibiotic erythromycin.
Malignancies
Obviously a distal gastric cancer may obstruct the pylorus and delay emptying. In addition, malignancies of the pancreas may cause extrinsic compression of the duodenum and delay emptying. Treatment in these cases is by gastric decompression using a wide bore nasogastric tube and insertion of a stent or, if that is not possible, by a surgical gastroenterostomy. As a general rule gastroenterostomies constructed for bypass of malignancy are usually placed on the anterior wall of the stomach (in spite of the fact that they empty less well). A Roux en Y bypass may also be undertaken, but the increased number of anastomoses for this, in malignant disease that is being palliated, is probably not justified.
Congenital Hypertrophic Pyloric Stenosis
This is typically a disease of infancy. Most babies will present around 6 weeks of age with projectile non bile stained vomiting. It has an incidence of 2.4 per 1000 live births and is more common in males. Diagnosis is usually made by careful history and examination and a mass may be palpable in the epigastrium (often cited seldom felt!). The most important diagnostic test is an ultrasound that usually demonstrates the hypertrophied pylorus. Blood tests may reveal a hypochloraemic metabolic alkalosis if the vomiting is long standing. Once the diagnosis is made the infant is resuscitated and a pyloromyotomy is performed (either open or laparoscopically). Once treated there are no long term sequelae.
What types of thoracic trauma are you familiar with?
How would you manage a patient with a suspected thoracic trauma?
Thoracic trauma can be blunt or penetrating, superficial or deep. The mechanism of injury has a considerable bearing on the injury pattern that may be seen. For example, deceleration injury and associated blunt trauma can account for the lethal combination of great vessel disruption and associated parenchymal lung injury. In contrast, penetrating injuries such as a stabbing can result in creating of parenchymal flaps of lung which allow the development of tension pneumothorax.
Ideally, patients with suspected thoracic trauma should be managed in a level three trauma centre with full trauma team and support facilities available. Significant thoracic injuries will usually trigger a trauma call and as a result, the trauma team will usually be available when the patient arrives. As a result, a number of individuals will be present who will have preassigned roles. The most important, particularly in thoracic trauma is the primary survey. Thoracic injuries can affect all components of the primary survey and some, such a tension pneumothorax will require immediate management.
Once the primary survey is completed and the patient stabilised, a detailed secondary survey and appropriate cross sectional imaging is required to completely assess the patient.
Management is tailored to the findings of these investigations.
Types of thoracic trauma:
Tension pneumothorax:
- Often laceration to lung parenchyma with flap
- Pressure develops in thorax
- Most common cause is mechanical ventilation in patient with pleural injury
- Symptoms overlap with cardiac tamponade, hyper-resonant percussion note is more likely in tension pnemothorax
Flail chest:
- Chest wall disconnects from thoracic cage
- Multiple rib fractures (at least two fractures per rib in at least two ribs)
- Associated with pulmonary contusion
- Abnormal chest motion
- Avoid over hydration and fluid overload
Pneumothorax:
- Most common cause is lung laceration with air leakage
- Most traumatic pneumothoraces should have a chest drain
- Patients with traumatic pneumothorax should never be mechanically ventilated until a chest drain is inserted
Haemothorax
- Most commonly due to laceration of lung, intercostal vessel or internal mammary artery
- Haemothoraces large enough to appear on CXR are treated with large bore chest drain
- Surgical exploration is warranted if >1500ml blood drained immediately
Cardiac tamponade
- Beck’s triad: elevated venous pressure, reduced arterial pressure, reduced heart sounds
- Pulsus paradoxus
- May occur with as little as 100ml blood
Pulmonary contusion
- Most common potentially lethal chest injury
- Arterial blood gases and pulse oximetry important
- Early intubation within an hour if significant hypoxia
Blunt cardiac injury
- Usually occurs secondary to chest wall injury
- ECG may show features of myocardial infarction
- Sequelae: hypotension, arrhythmias, cardiac wall motion abnormalities
Aorta disruption
- Deceleration injuries
- Contained haematoma
- Widened mediastinum
Diaphragm disruption
- Most due to motor vehicle accidents and blunt trauma causing large radial tears (laceration injuries result in small tears)
- More common on left side
- Insert gastric tube, may pass into intrathoracic stomach
Mediastinal traversing wounds
- Entrance wound in one hemithorax and exit wound/foreign body in opposite hemithorax
- Mediastinal haematoma or pleural cap suggests great vessel injury
- Mortality is 20%
What is a flail chest injury?
When would you consider it suitable for a patient to undergo an emergency room thoracotomy? What are the main steps involved in an emergency room thoracotomy?
A flail chest injury is said to occur when the chest wall is injured in such a way that at least three or more ribs are broken in 2 or more places. The result of this process is that is creates a segment of chest wall that is relatively inactive and cannot participate in chest expansion. This has ventialtory consequences. The usual mechanism of injury is blunt trauma. There are several reasons why flail injuries are so significant. Firstly, they imply a significant chest wall injury, particularly in the young. Secondly, there is the real potential for associated thoracic injuries such as pneumothorax. Thirdly, there is always a degree of underlying pulmonary contusion that impairs oxygen exchange. Finally, there are ventilatory effects of the flail segment itself.
Emerg room thoracotomy: The indications for this procedure are largely confined to witnessed cardiac arrest following penetrating chest trauma. Outcomes in patients who have blunt trauma or a non witnessed arrest are abysmal and the procedure almost never justified in such cases.
Safety is paramount with these procedures, working conditions are poor, the environment crowded and there is real potential for injury to healthcare workers. The most senior surgeon (with the relevant experience!) should be summoned.
The procedure is performed by placing the patient supine. Incisions are made in the fifth interspace and extended medially. At this point a Roberts or similar type clamp is tunneled under the sternum, the end of a Gigli saw is then grasped and pulled under the sterum. The Gigli saw is then used to open the sternum. The result is a clamshell type thoracotomy. A Finichetto retractor is inserted. The pericardial sac is opened and then both pleura. If there is a cardiac puncture wound then the opening of the sac will release the tamponade, a Foley catheter is then placed into the wound and the balloon inflated with saline, this should be performed carefully, breakage of the balloon will result in fragments of rubber being ejected from the heart and this has adverse effects if such fragments lodge in the CNS. If the heart has no injury or once you have temporised any that are present the chest is quickly inspected. If there is any major bleeding then the best option is to cross clamp the hilum with an atraumatic clamp such as an intestinal clamp. The patient should then be transferred to theatre for definitive surgery.
Types of thoracic trauma:
Tension pneumothorax:
- Often laceration to lung parenchyma with flap
- Pressure develops in thorax
- Most common cause is mechanical ventilation in patient with pleural injury
- Symptoms overlap with cardiac tamponade, hyper-resonant percussion note is more likely in tension pnemothorax
Flail chest:
- Chest wall disconnects from thoracic cage
- Multiple rib fractures (at least two fractures per rib in at least two ribs)
- Associated with pulmonary contusion
- Abnormal chest motion
- Avoid over hydration and fluid overload
Pneumothorax:
- Most common cause is lung laceration with air leakage
- Most traumatic pneumothoraces should have a chest drain
- Patients with traumatic pneumothorax should never be mechanically ventilated until a chest drain is inserted
Haemothorax
- Most commonly due to laceration of lung, intercostal vessel or internal mammary artery
- Haemothoraces large enough to appear on CXR are treated with large bore chest drain
- Surgical exploration is warranted if >1500ml blood drained immediately
Cardiac tamponade
- Beck’s triad: elevated venous pressure, reduced arterial pressure, reduced heart sounds
- Pulsus paradoxus
- May occur with as little as 100ml blood
Pulmonary contusion
- Most common potentially lethal chest injury
- Arterial blood gases and pulse oximetry important
- Early intubation within an hour if significant hypoxia
Blunt cardiac injury
- Usually occurs secondary to chest wall injury
- ECG may show features of myocardial infarction
- Sequelae: hypotension, arrhythmias, cardiac wall motion abnormalities
Aorta disruption
- Deceleration injuries
- Contained haematoma
- Widened mediastinum
Diaphragm disruption
- Most due to motor vehicle accidents and blunt trauma causing large radial tears (laceration injuries result in small tears)
- More common on left side
- Insert gastric tube, may pass into intrathoracic stomach
Mediastinal traversing wounds
- Entrance wound in one hemithorax and exit wound/foreign body in opposite hemithorax
- Mediastinal haematoma or pleural cap suggests great vessel injury
- Mortality is 20%
What is meant by the term cerebral perfusion pressure? What factors affect the cerebral perfusion pressure and how is it calculated? What specific factors should be considered when measuring the mean arterial pressure of severely injured patients with associated head injuries?
The cerebral perfusion pressure is the gradient that exists across the vascular network of the brain and accounts for the supply of blood to the CNS.
The brain typically autoregulates its blood supply over a range of blood pressures (usually between 70-130mmHg). The cerebral perfusion pressure can be calculated by taking the patients mean arterial pressure and subtracting the intra cranial pressure from this value. The CPP is affected by processes within and outside the cranial cavity. The most important external factor is the blood pressure, within the CNS, the most significant factor is the vasoactive events by which the brain autoregulates its blood supply, namely vasoconstriction or dilatation. Another factor are the changes to intra cranial pressure and this can be affected by mass lesions, trauma or inflammatory processes.
The mean arterial pressure can be calculated indirectly by measurement of the blood pressure indirectly. However, in the critical care setting, the MAP is usually measured using an indwelling arterial line. The pressure transducer for this device is usually located in a level with the heart and measurements referenced to this. However, in patients with head injuries the precise calculation of the CPP is required and for this to be accurate the MAP of the brain should be used. In patients who are supine there should be little difference between heart and head. However, if the patient is not level then the transducer should be placed externally on the same level as the Foramen of Munro.
The brain autoregulates it’s blood supply to maintain a cerebral perfusion pressure of around 70 mmHg. The cerebral perfusion pressure is related to the mean arterial pressure and intra cranial pressure.
CPP= MAP - ICP
Note that the mean arterial pressure is used for this calculation
Measurement of MAP is usually measured invasively in patients with head injury. Where MAP measurements are used to guide management of head injured patients, the transducer should be placed on the level of the Foramen of Munro rather than the heart as measurement at heart level can result in overestimating the MAP of blood reaching the brain (especially if the patient’s head is elevated).
Factors affecting the cerebral perfusion pressure
Intra cranial:
Raised ICP
- Mass lesions
- Inflammatory disorders
- CNS trauma
- Vasoconstriction/ dilatation
- CNS venous thrombosis
Extra cranial
- Changes in blood pressure
- Arterial lesions
- Raised venous pressure
- Drugs
- The PaCO2 is the most potent CNS vasoactive mediator and this can be exploited by hyperventilating patients with head injuries
What is parathyroid hormone?
It is an 84 amino acid polypeptide hormone released from the parathyroid glands into the systemic circulation. It release is controlled by serum calcium levels. It has a very short half life in the systemic circulation of around 4 minutes.The main effects of parathyroid hormone are to increase the concentration of plasma calcium by increasing the release of calcium and phosphate from bone matrix, increasing calcium reabsorption by the kidney, and increasing renal production of 1,25-dihydroxyvitamin D-3, which increases intestinal absorption of calcium. Thus, overproduction of parathyroid hormone results in elevated levels of plasma calcium. Parathyroid hormone also causes phosphaturia, thereby decreasing serum phosphate levels.
Parathyroid hormone is secreted by the chief cells of the parathyroid glands. It acts to increase serum calcium concentration by stimulation of the PTH receptors in the kidney and bone. PTH has a plasma half life of 4 minutes.
- Bone: Binds to osteoblasts which signal to osteoclasts to cause resorption of bone and release calcium.
- Kidney: Active reabsorption of calcium and magnesium from the distal convoluted tubule. Decreases reabsorption of phosphate.
- Intestine via kidney: Increases intestinal calcium absorption by increasing activated vitamin D. Activated vitamin D increases calcium absorption.
The secretion of PTH is directly related to the serum concentration of ionised calcium.
Hyperparathyroidism
Three main forms of the condition are recognised.
Indications for surgery in primary hyperparathyroidism:
- Symptomatic hypercalcaemia
- Deteriorating renal function
- Reduced bone density
- Urinary tract calculi
Imaging
- USS (identifies around 75% of enlarged glands)
- Technetium labeled sestamibi (MIBI) isotope scans
- SPECT
- USS alone is usually all that is required prior to primary neck exploration
Consent for parathyroidectomy
- Persistent hyperparathyroidism 5%
- Recurrent laryngeal nerve injury 1%
- Haemorrhage 1%
- Permanent hypoparathyroidism
- Recurrence

What is the commonest cause of hypercalcaemia in a patient in the community? What is the key difference between primary and secondary hyperparathyroidism?
What are the treatment options for managing primary hyperparathyroidism? What factors should be considered in the operative work up prior to parathyroidectomy for primary hyperparathyroidism?
Following removal of the suspect gland and before closing the wound, what strategies may be used to ensure the culprit gland has been removed?
Primary hyperparathyroidism is the commonest cause in community patients. In hospitalised patients, the commonest cause of hypercalcaemia is malignant disease.
Primary hyperparathyroidism is most commonly due to a parathyroid adenoma that occurs sporadically and results in the excessive release of PTH. Secondary hyperparathyroidism occurs as a result of chronic renal failure. As a result, the kidney cannot convert vitamin D into physiologically active 1,25 cholecalciferol. This results in reduced intestinal absorption of calcium resulting in low serum calcium, and elevated phosphate due to the inability of the kidney to excrete phosphate. This leads to increased release of PTH and hyperplasia of all the parathyroid glands.
Secondary hyperparathyroidism may reverse following renal transplantation if it persists then it is termed tertiary hyperparathyroidism
Mx Primary hyperPTH: The immediate priority is to assess the patient and if they are acutely unwell then this will require supportive care. Patients with very high serum calcium levels may need a bisphosphonate infusion.
Patients with very minimal elevations of serum calcium and no symptoms (i.e. incidentally diagnosed) can be managed conservatively.
For the majority of patients, the main management of primary hyperparathyroidism is surgical removal of the affected parathyroid gland.
Pre-op assessment:
- The affected gland should be localised, in 75% of cases, imaging of the neck with USS should identify the culprit gland.
- The patient should be fully optimised and any co- morbidities addressed. A careful check should be made to ensure that the patient is not part of the MEN disease spectrum.
- The patient should be fully consented for surgery, risks of laryngeal nerve injury, failure to localise the gland, permanent hypothyroidism and recurrence should all be mentioned (though all are rare).
- Some surgeons commence an infusion of methylene blue perioperatively as it preferentially stains parathyroid tissue.
Strategies to ensure culprit gland removed: There are two main options, the first is frozen section analysis of the gland. The second is serum measurement of PTH. Because the hormone has a very short half life, if the correct gland has been removed, the serum PTH levels should fall to normal within 30 minutes.
Parathyroid hormone is secreted by the chief cells of the parathyroid glands. It acts to increase serum calcium concentration by stimulation of the PTH receptors in the kidney and bone. PTH has a plasma half life of 4 minutes.
- Bone: Binds to osteoblasts which signal to osteoclasts to cause resorption of bone and release calcium.
- Kidney: Active reabsorption of calcium and magnesium from the distal convoluted tubule. Decreases reabsorption of phosphate.
- Intestine via kidney: Increases intestinal calcium absorption by increasing activated vitamin D. Activated vitamin D increases calcium absorption.
The secretion of PTH is directly related to the serum concentration of ionised calcium.
Hyperparathyroidism
Three main forms of the condition are recognised.
Indications for surgery in primary hyperparathyroidism:
- Symptomatic hypercalcaemia
- Deteriorating renal function
- Reduced bone density
- Urinary tract calculi
Imaging
- USS (identifies around 75% of enlarged glands)
- Technetium labeled sestamibi (MIBI) isotope scans
- SPECT
- USS alone is usually all that is required prior to primary neck exploration
Consent for parathyroidectomy
- Persistent hyperparathyroidism 5%
- Recurrent laryngeal nerve injury 1%
- Haemorrhage 1%
- Permanent hypoparathyroidism
- Recurrence

What is the American Society of anesthesiologists physical status scoring system, and why is it used?
What are the various categories?
Are you aware of any other scoring systems in mainstream use?
The ASA system is now over 50 years old and was introduced in the US to allow clinicians to rapidly, easily and reproducibly to physically classify patients.
There are 5 groups in regular use, these range from ASA 1, which describes a fit and well person, through to ASA 5 which describes a moribund patient who may well not survive the next 24 hours without surgery. A group, ASA 6, is used for a patient whose organs are being donated and who is brain dead.
Other scoring systems in use include the APACHE II system which is largely used for patients being admitted to the Intensive Care Unit and which considers a number of physiological and biochemical parameters and allows for accurate risk stratification. Because it is usually only applied to ITU patients it is less useful in determining risk in surgical patients. The POSSUM scoring system (Physiological and Operative Severity Score for the enUmeration of Mortality and Morbidity) can be usefully used to predict mortality and morbidity for a range of different surgical procedures and considers a range of biochemical and physiological parameters. It differs from the ASA system in that it can assign a percentage risk at an individual patient level.
- 1: No organic physiological, biochemical or psychiatric disturbance. The surgical pathology is localised and has not invoked systemic disturbance
- 2: Mild or moderate systemic disruption caused either by the surgical disease process or though underlying pre-existing disease
- 3: Severe systemic disruption caused either by the surgical pathology or pre-existing disease
- 4: Patient has severe systemic disease that is a constant threat to life
- 5: A patient who is moribund and will not survive without surgery
What is meant by the term diverticulum? Which areas of the alimentary tract can be affected by diverticular disease and why?
The term diverticulum means a blind ending tube leading from a cavity or passage.
Diverticular disease can present at any site in the alimentary tract. Proximally, they typically occur through Killians dehiscence, resulting in a pharyngeal pouch. They rarely form in the oesophagus and stomach. They can also affect the small bowel, in the duodenum, they are typically located in close proximity to the ampulla (which can make ERCP difficult). The jejunum is more commonly affected than the ileum and the anti mesenteric border is the commonest site. However, it is the colon which is the commonest site for the development of diverticulum. The sigmoid colon is the site most typically affected and is by far the commonest site to develop diverticulae in the alimentary tract as a whole.
The pathogenesis of diverticular disease is poorly understood and whilst absence of dietary fibre is implicated in the pathogenesis of colonic diverticular disease, it is likely that there are additional confounders that have yet to be fully elucidated. In the colon, the diverticulae tend to form at sites where vessels enter the muscularis to supply the mucosa. The rectum, which lacks tenia coli, rarely develops diverticulae.
Diverticular disease is a common surgical problem. It consists of herniation of colonic mucosa through the muscular wall of the colon. The usual site is between the taenia coli where vessels pierce the muscle to supply the mucosa. For this reason, the rectum, which lacks taenia, is often spared.
Symptoms
- Altered bowel habit
- Bleeding
- Abdominal pain
Complications
- Diverticulitis
- Haemorrhage
- Development of fistula
- Perforation and faecal peritonitis
- Perforation and development of abscess
- Development of diverticular phlegmon
Diagnosis
Patients presenting in clinic will typically undergo either a colonoscopy, CT cologram or barium enema as part of their diagnostic work up. All tests can identify diverticular disease. It can be far more difficult to confidently exclude cancer, particularly in diverticular strictures.
Acutely unwell surgical patients should be investigated in a systematic way. Plain abdominal films and an erect chest x-ray will identify perforation. An abdominal CT scan (not a CT cologram) with oral and intravenous contrast will help to identify whether acute inflammation is present but also the presence of local complications such as abscess formation.
Severity Classification- Hinchey
- I Para-colonic abscess
- II Pelvic abscess
- III Purulent peritonitis
- IV Faecal peritonitis
Treatment
- Increase dietary fibre intake.
- Mild attacks of diverticulitis may be managed conservatively with antibiotics.
- Peri colonic abscesses should be drained either surgically or radiologically.
- Recurrent episodes of acute diverticulitis requiring hospitalisation are a relative indication for a segmental resection.
- Hinchey IV perforations (generalised faecal peritonitis) will require a resection and usually a stoma. This group have a very high risk of post operative complications and usually require HDU admission.
In the case of colonic diverticular disease, what complications are recognized? What investigative modalities are indicated in identifying a case of suspected diverticulosis in a 53 year old male with left iliac fossa pain?
What is the treatment of choice for a 73 year old lady who had been admitted with large bowel obstruction due to a fibrotic sigmoid stricture arising from an area of diverticular disease who has now recovered?
The commonest complication of colonic diverticular disease is inflammation, diverticulitis. Bleeding is the second commonest complication and diverticular associated bleeding is one of the commonest causes of lower GI bleeding. Other complications include colonic perforation at the site of a diverticulum which may result in peritonitis or localized abscess formation. Recurrent attacks of low grade inflammation can result in the development of inflammatory phlegmons or chronic fibrotic strictures.
The investigations will be determined by the patients physical status and co-morbidities. Acutely unwell patients requiring hospital admission will generally require CT scanning to determine whether there is acute inflammation present or a complication such as a peri-colic abscess.
In patients who are relatively well, investigations can be undertaken on an outpatient basis. Here the choice lies between CT colonoscopy or conventional colonoscopy. Since barium enema lacks the diagnostic accuracy of these two investigative techniques, it is seldom indicated. The main reason for carefully investigating these patients is to exclude an underlying cancer.
73 yr old lady: The choices here lie between conservative management or operative intervention. Conservative management would involve the patient adopting a low residue diet and taking stool softeners. There is a risk that the patient may go on to develop a further episode of large bowel obstruction which makes this strategy unattractive.
Colonic stents function poorly in diverticular strictures and are not indicated.
The surgical options include segmental resection, in this case a high anterior resection, diverting loop colostomy or Hartmann’s procedure. In an otherwise fit patient with no continence issues, a resection and primary anastomosis would seem reasonable. If the patient undergoes surgery in the obstructed setting then one of the two latter procedures would then be indicated.
Diverticular disease is a common surgical problem. It consists of herniation of colonic mucosa through the muscular wall of the colon. The usual site is between the taenia coli where vessels pierce the muscle to supply the mucosa. For this reason, the rectum, which lacks taenia, is often spared.
Symptoms
- Altered bowel habit
- Bleeding
- Abdominal pain
Complications
- Diverticulitis
- Haemorrhage
- Development of fistula
- Perforation and faecal peritonitis
- Perforation and development of abscess
- Development of diverticular phlegmon
Diagnosis
Patients presenting in clinic will typically undergo either a colonoscopy, CT cologram or barium enema as part of their diagnostic work up. All tests can identify diverticular disease. It can be far more difficult to confidently exclude cancer, particularly in diverticular strictures.
Acutely unwell surgical patients should be investigated in a systematic way. Plain abdominal films and an erect chest x-ray will identify perforation. An abdominal CT scan (not a CT cologram) with oral and intravenous contrast will help to identify whether acute inflammation is present but also the presence of local complications such as abscess formation.
Severity Classification- Hinchey
- I Para-colonic abscess
- II Pelvic abscess
- III Purulent peritonitis
- IV Faecal peritonitis
Treatment
- Increase dietary fibre intake.
- Mild attacks of diverticulitis may be managed conservatively with antibiotics.
- Peri colonic abscesses should be drained either surgically or radiologically.
- Recurrent episodes of acute diverticulitis requiring hospitalisation are a relative indication for a segmental resection.
- Hinchey IV perforations (generalised faecal peritonitis) will require a resection and usually a stoma. This group have a very high risk of post operative complications and usually require HDU admission.


