MRCS Part B Anatomy Flashcards
(85 cards)
Popliteal Fossa: Which structures are demonstrated by labels 1, 2, and 3?

The structures are:
- Tibial nerve
- Common peroneal nerve
- Sural nerve
Boundaries of the popliteal fossa
Laterally: Biceps femoris above, lateral head of gastrocnemius and plantaris below
Medially: Semimembranosus and semitendinosus above, medial head of gastrocnemius below
Floor: Popliteal surface of the femur, posterior ligament of knee joint and popliteus muscle
Roof: Superficial and deep fascia
Contents:
Popliteal artery and vein
Small saphenous vein
Common peroneal nerve
Tibial nerve
Posterior cutaneous nerve of the thigh
Genicular branch of the obturator nerve
Lymph nodes

Popliteal Fossa: Which structures are demonstrated by labels 1, 2, 3, 4 and 5?

The structures are:
- Semitendinosus
- Semimembranosus
- Gracilis
- Gastrocnemius
- Biceps femoris
Boundaries of the popliteal fossa
Laterally: Biceps femoris above, lateral head of gastrocnemius and plantaris below
Medially: Semimembranosus and semitendinosus above, medial head of gastrocnemius below
Floor: Popliteal surface of the femur, posterior ligament of knee joint and popliteus muscle
Roof: Superficial and deep fascia
Contents:
Popliteal artery and vein
Small saphenous vein
Common peroneal nerve
Tibial nerve
Posterior cutaneous nerve of the thigh
Genicular branch of the obturator nerve
Lymph nodes

Which structure is located deepest in the popliteal fossa?
The popliteal artery is located immediately adjacent to the posterior surface of the femur and the most deeply located structure. The vein lies superficial to it.
Popliteal fossa
Boundaries of the popliteal fossa
Laterally: Biceps femoris above, lateral head of gastrocnemius and plantaris below
Medially: Semimembranosus and semitendinosus above, medial head of gastrocnemius below
Floor: Popliteal surface of the femur, posterior ligament of knee joint and popliteus muscle
Roof: Superficial and deep fascia
Contents:
Popliteal artery and vein
Small saphenous vein
Common peroneal nerve
Tibial nerve
Posterior cutaneous nerve of the thigh
Genicular branch of the obturator nerve
Lymph nodes

Femur: Please point out the key bony landmarks visible on this bone.

Being handed a femur in the anatomy section is a gift. A slick and well practised answer is essential. Begin your answer by naming the bone and orientating it. You should then move on to describe the key landmarks. Since you will have the bone in the exam you can use this as a prompt.
Salient points to identify include the head, neck and body, the greater and lesser trochanters, the adductor tubercle. You should also identify the condyles.
Femur
Extends from a rounded head, which articulates with the acetabulum down to the knee joint where the two large condyles at it’s inferior aspect articulate with the tibia.
The superior aspect comprises a head and neck which pass inferolaterally to the body and the two trochanters. These lie at the junction between the neck and the body.
The neck meets the body of the femur at an angle of 125o.
Developmentally, the neck is part of the body but is demarcated from it by a wide rough intertrochanteric crest, this continues inferomedially as a spiral line that runs below the lesser trochanter. Medially, the intertrochanteric line gives attachment to the inferior end of the iliofemoral ligament. The neck is covered by synovial membrane up to the intertrochanteric line. The posterior aspect of the neck is demarcated from the shaft by the intertrochanteric crest and only it’s medial aspect is covered by synovium and the joint capsule.
The greater trochanter has discernible surfaces that form the site of attachment of the gluteal muscles.Laterally, the greater trochanter overhangs the body and this forms part of the origin of vastus lateralis
Viewed anteriorly, the body of the femur appears rounded. Viewed laterally, it has an anterior concavity which gives fullness to the anterior thigh. Posteriorly, there is a ridge of bone, the linea aspera. The surface of the anterior aspect of the body forms the origin of the vastus intermedius. More medially, it forms the origin of vastus medialis.
The upper and middle aspects of the linea aspera form part of the origin of the attachments of the thigh adductors. Inferiorly, it spans out to form the bony floor of the popliteal fossa. At the inferior aspect of the popliteal surface the surface curves posteriorly to form the femoral condyles.
The structures that are attached to the inferior aspect of the linea aspera split with it as it approaches the popliteal fossa. Thus the vastus medialis and adductor magnus continue with the medial split and the biceps femoris and vastus intermedius along the lateral split.
Blood supply
The femur has a rich blood supply and numerous vascular foramina exist throughout it’s length. The blood supply to the femoral head is clinically important and is provided by the medial circumflex femoral and lateral circumflex femoral arteries (Branches of profunda femoris). Also from the inferior gluteal artery. These form an anastomosis and travel to up the femoral neck to supply the head.

What is the usual angle between the femoral neck and the femoral shaft?
This can vary according to sex and age. However, it is typically around 125o.
Femur
Extends from a rounded head, which articulates with the acetabulum down to the knee joint where the two large condyles at it’s inferior aspect articulate with the tibia.
The superior aspect comprises a head and neck which pass inferolaterally to the body and the two trochanters. These lie at the junction between the neck and the body.
The neck meets the body of the femur at an angle of 125o.
Developmentally, the neck is part of the body but is demarcated from it by a wide rough intertrochanteric crest, this continues inferomedially as a spiral line that runs below the lesser trochanter. Medially, the intertrochanteric line gives attachment to the inferior end of the iliofemoral ligament. The neck is covered by synovial membrane up to the intertrochanteric line. The posterior aspect of the neck is demarcated from the shaft by the intertrochanteric crest and only it’s medial aspect is covered by synovium and the joint capsule.
The greater trochanter has discernible surfaces that form the site of attachment of the gluteal muscles.Laterally, the greater trochanter overhangs the body and this forms part of the origin of vastus lateralis
Viewed anteriorly, the body of the femur appears rounded. Viewed laterally, it has an anterior concavity which gives fullness to the anterior thigh. Posteriorly, there is a ridge of bone, the linea aspera. The surface of the anterior aspect of the body forms the origin of the vastus intermedius. More medially, it forms the origin of vastus medialis.
The upper and middle aspects of the linea aspera form part of the origin of the attachments of the thigh adductors. Inferiorly, it spans out to form the bony floor of the popliteal fossa. At the inferior aspect of the popliteal surface the surface curves posteriorly to form the femoral condyles.
The structures that are attached to the inferior aspect of the linea aspera split with it as it approaches the popliteal fossa. Thus the vastus medialis and adductor magnus continue with the medial split and the biceps femoris and vastus intermedius along the lateral split.
Blood supply
The femur has a rich blood supply and numerous vascular foramina exist throughout it’s length. The blood supply to the femoral head is clinically important and is provided by the medial circumflex femoral and lateral circumflex femoral arteries (Branches of profunda femoris). Also from the inferior gluteal artery. These form an anastomosis and travel to up the femoral neck to supply the head.
Which muscle originates from the area marked number 1 and which two muscles insert into sites 2 and 3?

Vastus intermedius originates from area 1. Gluteus minimis inserts into area 2 and psoas major inserts into area 3.
Femur
Extends from a rounded head, which articulates with the acetabulum down to the knee joint where the two large condyles at it’s inferior aspect articulate with the tibia.
The superior aspect comprises a head and neck which pass inferolaterally to the body and the two trochanters. These lie at the junction between the neck and the body.
The neck meets the body of the femur at an angle of 125o.
Developmentally, the neck is part of the body but is demarcated from it by a wide rough intertrochanteric crest, this continues inferomedially as a spiral line that runs below the lesser trochanter. Medially, the intertrochanteric line gives attachment to the inferior end of the iliofemoral ligament. The neck is covered by synovial membrane up to the intertrochanteric line. The posterior aspect of the neck is demarcated from the shaft by the intertrochanteric crest and only it’s medial aspect is covered by synovium and the joint capsule.
The greater trochanter has discernible surfaces that form the site of attachment of the gluteal muscles.Laterally, the greater trochanter overhangs the body and this forms part of the origin of vastus lateralis
Viewed anteriorly, the body of the femur appears rounded. Viewed laterally, it has an anterior concavity which gives fullness to the anterior thigh. Posteriorly, there is a ridge of bone, the linea aspera. The surface of the anterior aspect of the body forms the origin of the vastus intermedius. More medially, it forms the origin of vastus medialis.
The upper and middle aspects of the linea aspera form part of the origin of the attachments of the thigh adductors. Inferiorly, it spans out to form the bony floor of the popliteal fossa. At the inferior aspect of the popliteal surface the surface curves posteriorly to form the femoral condyles.
The structures that are attached to the inferior aspect of the linea aspera split with it as it approaches the popliteal fossa. Thus the vastus medialis and adductor magnus continue with the medial split and the biceps femoris and vastus intermedius along the lateral split.
Blood supply
The femur has a rich blood supply and numerous vascular foramina exist throughout it’s length. The blood supply to the femoral head is clinically important and is provided by the medial circumflex femoral and lateral circumflex femoral arteries (Branches of profunda femoris). Also from the inferior gluteal artery. These form an anastomosis and travel to up the femoral neck to supply the head.
What type of bone is marked by the letter “x”. What is it’s functional relevance?

The bone is the patella, it is a sesamoid bone contained within the tendon of quadriceps femoris. It plays an important role in reducing the work required to extend the knee joint.
Femur
Extends from a rounded head, which articulates with the acetabulum down to the knee joint where the two large condyles at it’s inferior aspect articulate with the tibia.
The superior aspect comprises a head and neck which pass inferolaterally to the body and the two trochanters. These lie at the junction between the neck and the body.
The neck meets the body of the femur at an angle of 125o.
Developmentally, the neck is part of the body but is demarcated from it by a wide rough intertrochanteric crest, this continues inferomedially as a spiral line that runs below the lesser trochanter. Medially, the intertrochanteric line gives attachment to the inferior end of the iliofemoral ligament. The neck is covered by synovial membrane up to the intertrochanteric line. The posterior aspect of the neck is demarcated from the shaft by the intertrochanteric crest and only it’s medial aspect is covered by synovium and the joint capsule.
The greater trochanter has discernible surfaces that form the site of attachment of the gluteal muscles.Laterally, the greater trochanter overhangs the body and this forms part of the origin of vastus lateralis
Viewed anteriorly, the body of the femur appears rounded. Viewed laterally, it has an anterior concavity which gives fullness to the anterior thigh. Posteriorly, there is a ridge of bone, the linea aspera. The surface of the anterior aspect of the body forms the origin of the vastus intermedius. More medially, it forms the origin of vastus medialis.
The upper and middle aspects of the linea aspera form part of the origin of the attachments of the thigh adductors. Inferiorly, it spans out to form the bony floor of the popliteal fossa. At the inferior aspect of the popliteal surface the surface curves posteriorly to form the femoral condyles.
The structures that are attached to the inferior aspect of the linea aspera split with it as it approaches the popliteal fossa. Thus the vastus medialis and adductor magnus continue with the medial split and the biceps femoris and vastus intermedius along the lateral split.
Blood supply
The femur has a rich blood supply and numerous vascular foramina exist throughout it’s length. The blood supply to the femoral head is clinically important and is provided by the medial circumflex femoral and lateral circumflex femoral arteries (Branches of profunda femoris). Also from the inferior gluteal artery. These form an anastomosis and travel to up the femoral neck to supply the head.
Identify the structures A-H in the image below.

A Vastus medialis
B Sartorius
C Gracilis
D Gastrocnemius
E Semitendinosus
F Semimembranosus
G Rectus femoris
H Adductor magnus tendon
Femur
Extends from a rounded head, which articulates with the acetabulum down to the knee joint where the two large condyles at it’s inferior aspect articulate with the tibia.
The superior aspect comprises a head and neck which pass inferolaterally to the body and the two trochanters. These lie at the junction between the neck and the body.
The neck meets the body of the femur at an angle of 125o.
Developmentally, the neck is part of the body but is demarcated from it by a wide rough intertrochanteric crest, this continues inferomedially as a spiral line that runs below the lesser trochanter. Medially, the intertrochanteric line gives attachment to the inferior end of the iliofemoral ligament. The neck is covered by synovial membrane up to the intertrochanteric line. The posterior aspect of the neck is demarcated from the shaft by the intertrochanteric crest and only it’s medial aspect is covered by synovium and the joint capsule.
The greater trochanter has discernible surfaces that form the site of attachment of the gluteal muscles.Laterally, the greater trochanter overhangs the body and this forms part of the origin of vastus lateralis
Viewed anteriorly, the body of the femur appears rounded. Viewed laterally, it has an anterior concavity which gives fullness to the anterior thigh. Posteriorly, there is a ridge of bone, the linea aspera. The surface of the anterior aspect of the body forms the origin of the vastus intermedius. More medially, it forms the origin of vastus medialis.
The upper and middle aspects of the linea aspera form part of the origin of the attachments of the thigh adductors. Inferiorly, it spans out to form the bony floor of the popliteal fossa. At the inferior aspect of the popliteal surface the surface curves posteriorly to form the femoral condyles.
The structures that are attached to the inferior aspect of the linea aspera split with it as it approaches the popliteal fossa. Thus the vastus medialis and adductor magnus continue with the medial split and the biceps femoris and vastus intermedius along the lateral split.
Blood supply
The femur has a rich blood supply and numerous vascular foramina exist throughout it’s length. The blood supply to the femoral head is clinically important and is provided by the medial circumflex femoral and lateral circumflex femoral arteries (Branches of profunda femoris). Also from the inferior gluteal artery. These form an anastomosis and travel to up the femoral neck to supply the head.

What is the name of the structure indicated by the arrow and which muscle inserts into it?

This is the adductor tubercle and is the point of insertion of the adductor magnus tendon.

Identify the structures A-E.

A Tibialis anterior
B Peroneus longus
C Long head of biceps femoris
D Iliotibial tract
E Vastus lateralis

Which structures insert or originate from areas 1 and 2 in the image above?

- Anterior cruciate ligament
Anterior tibia to lateral intercondylar notch of femur
Prevents tibia sliding anteriorly - Posterior cruciate ligament
Posterior tibia to medial intercondylar notch of femur
Prevents tibia sliding posteriorly
What is this structure?
Outline its key anatomical features.

This is the first cervical vertebra, also known as the atlas. Among the vertebral bodies it has a unique structure which reflects its important structural role. It consists of a ring of bone with slender anterior and posterior arches that are united by lateral bony masses that extend transversely as the two transverse processes that contain the foramen transversarium.

Atlas
The first cervical vertebra (Atlas) is a ring of bone consisting of two slender arches, one anterior and the other posterior. These are united on each side by a lateral mass on which is situated the articular facets and the transverse processes. Most of the body of the atlas joins the axis to form the dens, and the anterior arch and lateral masses represent that part of the body normally formed by the vertebral arch ossification. The facets articulate with the skull above and the axis below. The normal articular facets are missing. The foramen transversarium transmits the vertebral artery.
What is the structure that attaches to the site marked with the “x” and what is its role?
What structure passes through the foramen transversarium?

This is the site of the attachment of the transverse ligament. It’s main role is to hold the dens in place.
The foramen transversarium transmits the vertebral artery, which enters it after passing along a groove on the superior aspect of the posterior arch.
Atlas
The first cervical vertebra (Atlas) is a ring of bone consisting of two slender arches, one anterior and the other posterior. These are united on each side by a lateral mass on which is situated the articular facets and the transverse processes. Most of the body of the atlas joins the axis to form the dens, and the anterior arch and lateral masses represent that part of the body normally formed by the vertebral arch ossification. The facets articulate with the skull above and the axis below. The normal articular facets are missing. The foramen transversarium transmits the vertebral artery.

Identify the structures 1,2 and 3.
What are the main branches of structure 1?
Which nerves are closely related to the aortic arch near structure 3?

In this section of the aortic arch, the left subclavian arises close to the brachiocephalic trunk. The structures are therefore;
- Brachiocephalic trunk
- Left common carotid artery
- Left subclavian
The brachiocephalic artery branches to provide the right common carotid artery and right subclavian artery. It typically branches at the level of the right sternoclavicular joint.
The two nerves are the phrenic nerve, which continues inferiorly across the anterior surface of the pericardium and the vagus nerve, which then branches around the inferior aspect of the aorta to give rise to the left recurrent laryngeal nerve.
Aortic arch and brachiocephalic vein
The arch of the aorta lies in the superior mediastinum, opposite the lower half of the manubrium. It runs superiorly and then arches in a posterior direction. It continues to curve posteriorly and then towards the left side of the body on a level of T4 where it then becomes the descending aorta.
Anterior to the arch of the aorta lie the thymic remnants, lungs and pleura. On it’s left hand side the following structures lie between the aortic arch and the pleura; phrenic nerve, inferior cardiac branch of the left vagus, superior cervical cardiac branch of the of the left sympathetic nerve and the trunk of the left vagus. The left superior intercostal vein crosses it, superficial to the left vagus nerve and deep to the left phrenic nerve. Posteriorly, on the right hand side of the arch lie the deep cardiac plexus, trachea, left recurrent laryngeal nerve, left border of the oesophagus, thoracic duct and finally the vertebral column.
There are three main branches, brachiocephalic trunk, left common carotid and left subclavian arteries. The brachiocephalic vein is related anteriorly.
The two brachiocephalic veins are formed by the union of the internal jugular and subclavian veins. The right runs a near vertical course and is joined by the left brachiocephalic vein to form the superior vena cava. The veins have no valves.
Identify the structures 1, 2 and 3.
How many valves are typically found in structures 1 and 2?
What are the tributaries of the left brachiocephalic vein?

Structures 1 and 2 are the right and left brachiocehphalic veins. They unite to form the superior vena cava (3).
The brachiocephalic veins (and indeed also the SVC) do not usually contain any valves. This is why the wave patterns of the JVP can be readily appreciated.
The subclavian vein, internal jugular vein, thoracic duct (which joins it at the angle of the junction of the internal jugular and subclavian veins), the vertebral, internal thoracic, inferior thyroid and superior intercostal veins of its own side.
Aortic arch and brachiocephalic vein
The arch of the aorta lies in the superior mediastinum, opposite the lower half of the manubrium. It runs superiorly and then arches in a posterior direction. It continues to curve posteriorly and then towards the left side of the body on a level of T4 where it then becomes the descending aorta.
Anterior to the arch of the aorta lie the thymic remnants, lungs and pleura. On it’s left hand side the following structures lie between the aortic arch and the pleura; phrenic nerve, inferior cardiac branch of the left vagus, superior cervical cardiac branch of the of the left sympathetic nerve and the trunk of the left vagus. The left superior intercostal vein crosses it, superficial to the left vagus nerve and deep to the left phrenic nerve. Posteriorly, on the right hand side of the arch lie the deep cardiac plexus, trachea, left recurrent laryngeal nerve, left border of the oesophagus, thoracic duct and finally the vertebral column.
There are three main branches, brachiocephalic trunk, left common carotid and left subclavian arteries. The brachiocephalic vein is related anteriorly.
The two brachiocephalic veins are formed by the union of the internal jugular and subclavian veins. The right runs a near vertical course and is joined by the left brachiocephalic vein to form the superior vena cava. The veins have no valves.
What structure is this?
Identify the structures labeled 1-5.

This is the left lung
The structures are:
1. Lower left pulmonary vein
2. Oblique fissure
3. Groove for left subclavian artery
4. Left pulmonary artery
5. Upper left pulmonary vein
Left lung
Above the hilum is the furrow produced by the aortic arch, and then superiorly the groove accommodating the left subclavian artery; Behind the hilum and pulmonary ligament is a vertical groove produced by the descending aorta, and in front of this, near the base of the lung, is the lower part of the oesophagus.
The root of the left lung passes under the aortic arch and in front of the descending aorta.
Right lung
Above the hilum is the azygos vein; Superior to this is the groove for the superior vena cava and right innominate vein; behind this, and nearer the apex, is a furrow for the innominate artery. Behind the hilum and the attachment of the pulmonary ligament is a vertical groove for the oesophagus; In front and to the right of the lower part of the oesophageal groove is a deep concavity for the extrapericardiac portion of the inferior vena cava.
The root of the right lung lies behind the superior vena cava and the right atrium, and below the azygos vein.
The right main bronchus is shorter, wider and more vertical than the left main bronchus and therefore the route taken by most foreign bodies.

What structures are likely to be located at sites 1,2 and 3?

- Descending thoracic aorta
- Heart
- Arch of aorta

Lung anatomy
The right lung is composed of 3 lobes divided by the oblique and transverse fissures. The left lung has two lobes divided by the oblique fissure.The apex of both lungs is approximately 4cm superior to the sterno-costal joint of the first rib. Immediately below this is a sulcus created by the subclavian artery.
Peripheral contact points of the lung
Base: diaphragm
Costal surface: corresponds to the cavity of the chest
Mediastinal surface: Contacts the mediastinal pleura. Has the cardiac impression. Above and behind this concavity is a triangular depression named the hilum, where the structures which form the root of the lung enter and leave the viscus. These structures are invested by pleura, which, below the hilum and behind the pericardial impression, forms the pulmonary ligament
Right lung
Above the hilum is the azygos vein; Superior to this is the groove for the superior vena cava and right innominate vein; behind this, and nearer the apex, is a furrow for the innominate artery. Behind the hilum and the attachment of the pulmonary ligament is a vertical groove for the oesophagus; In front and to the right of the lower part of the oesophageal groove is a deep concavity for the extrapericardiac portion of the inferior vena cava.
The root of the right lung lies behind the superior vena cava and the right atrium, and below the azygos vein.
The right main bronchus is shorter, wider and more vertical than the left main bronchus and therefore the route taken by most foreign bodies.
Left lung
Above the hilum is the furrow produced by the aortic arch, and then superiorly the groove accommodating the left subclavian artery; Behind the hilum and pulmonary ligament is a vertical groove produced by the descending aorta, and in front of this, near the base of the lung, is the lower part of the oesophagus.
The root of the left lung passes under the aortic arch and in front of the descending aorta.
Inferior borders of both lungs
6th rib in mid clavicular line
8th rib in mid axillary line
10th rib posteriorly
The pleura runs two ribs lower than the corresponding lung level.
Identify the structures labeled 1-4.

- Foramen magnum
- Occipital condyle
- Jugular fossa
- Foramen lacerum
Foramen/Location/Contents:
- Foramen ovale - Sphenoid bone - Otic ganglion, V3 (Mandibular nerve:3rd branch of trigeminal), Accessory meningeal artery, Lesser petrosal nerve, Emissary veins
- Foramen spinosum - Sphenoid bone - Middle meningeal artery, Meningeal branch of the Mandibular nerve
- Foramen rotundum - Sphenoid bone - Maxillary nerve (V2)
- Foramen lacerum - carotid canal - Sphenoid boneBase of the medial pterygoid plate. Internal carotid artery* Nerve and artery of the pterygoid canal
- Jugular foramen - Temporal bone - Anterior: inferior petrosal sinus
Intermediate: glossopharyngeal, vagus, and accessory nerves.
Posterior: sigmoid sinus (becoming the internal jugular vein) and some meningeal branches from the occipital and ascending pharyngeal arteries. - Foramen magnum - Occipital bone - Anterior and posterior spinal arteries, Vertebral arteries, Medulla oblongata
- Stylomastoid foramen - Temporal bone, Stylomastoid artery, Facial nerve
- Superior orbital fissure - Sphenoid bone, Oculomotor nerve (III), Recurrent meningeal artery, Trochlear nerve (IV), Lacrimal, frontal and nasociliary branches of ophthalmic nerve (V1), Abducent nerve (VI), Superior ophthalmic vein
*= In life the foramen lacerum is occluded by a cartilagenous plug. The ICA initially passes into the carotid canal which ascends superomedially to enter the cranial cavity through the foramen lacerum.

What is the most important factor in maintaining the stability of the knee joint?
Outline the different roles played by these structures and outline the anatomical attachments
The main stability of the knee joint is maintained by 2 sets of strong ligaments; the cruciate ligaments and the collateral ligaments.

The cruciate ligaments provide antero-posterior stability, the collateral ligaments serve to limit both medial and lateral stressors.
Medial collateral ligament: Medial femoral epicondyle –> Tibial surface, the deeper aspect attaches to the medial meniscus - valgus stability
Lateral collateral ligament: Lateral femoral epicondyle –> Fibula - varus stability
Anterior cruciate ligament: Anterior intercondylar area of tibia –> Lateral femoral condyle in intercondylar notch - prevents tibia sliding anteriorly
Posterior cruciate ligament: Posterior intercondylar area of tibia –> Medial femoral condyle in intercondylar notch - prevents tibia sliding posteriorly
Patellar ligament: Central band of the tendon of quadriceps femoris, extends from patella to tibial tuberosity
Knee joint
The knee joint is a synovial joint, the largest and most complicated. It consists of two condylar joints between the femur and tibia and a sellar joint between the patella and the femur. The tibiofemoral articular surfaces are incongruent, however, this is improved by the presence of the menisci. The degree of congruence is related to the anatomical position of the knee joint and is greatest in full extension.
Knee joint compartments
- Tibiofemoral: Comprised of the patella/femur joint, lateral and medial compartments (between femur condyles and tibia). Synovial membrane and cruciate ligaments partially separate the medial and lateral compartments
- Patellofemoral: Ligamentum patellae. Actions: provides joint stability in full extension
Fibrous capsule
The capsule of the knee joint is a complex, composite structure with contributions from adjacent tendons.
Anterior fibresThe capsule does not pass proximal to the patella. It blends with the tendinous expansions of vastus medialis and lateralis
Posterior fibresThese fibres are vertical and run from the posterior surface of the femoral condyles to the posterior aspect of the tibial condyle
Medial fibresAttach to the femoral and tibial condyles beyond their articular margins, blending with the tibial collateral ligament
Lateral fibresAttach to the femur superior to popliteus, pass over its tendon to head of fibula and tibial condyle
Bursae
- Anterior: Subcutaneous prepatellar bursa; between patella and skin, Deep infrapatellar bursa; between tibia and patellar ligament, Subcutaneous infrapatellar bursa; between distal tibial tuberosity and skin
- Laterally: Bursa between lateral head of gastrocnemius and joint capsule, Bursa between fibular collateral ligament and tendon of biceps femoris, Bursa between fibular collateral ligament and tendon of popliteus
- Medially: Bursa between medial head of gastrocnemius and the fibrous capsule, Bursa between tibial collateral ligament and tendons of sartorius, gracilis and semitendinosus, Bursa between the tendon of semimembranosus and medial tibial condyle and medial head of gastrocnemius
- Posterior: Highly variable and inconsistent
Menisci
Medial and lateral menisci compensate for the incongruence of the femoral and tibial condyles.
Composed of fibrous tissue.
Medial meniscus is attached to the tibial collateral ligament.
Lateral meniscus is attached to the loose fibres at the lateral edge of the joint and is separate from the fibular collateral ligament. The lateral meniscus is crossed by the popliteus tendon.
Nerve supply
The knee joint is supplied by the femoral, tibial and common peroneal divisions of the sciatic and by a branch from the obturator nerve. Hip pathology pain may be referred to the knee.
Blood supply
Genicular branches of the femoral artery, popliteal and anterior tibial arteries all supply the knee joint.
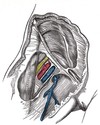
What nerves are at risk when performing an excision of the submandibular gland?
Where would you site an incision for a sub mandibular gland excision and why?
Mandibular branch of the facial nerve
Hypoglossal nerve
Lingual nerve
I would site the incision two to three finger breadths below the mandible to avoid injury to the marginal mandibular branch of the facial nerve
Submandibular gland
Relations of the submandibular gland
Superficial: Platysma, deep fascia and mandible, Submandibular lymph nodes, Facial vein (facial artery near mandible), Marginal mandibular nerve, Cervical branch of the facial nerve
Deep: Facial artery (inferior to the mandible), Mylohyoid muscle
Sub mandibular duct, Hyoglossus muscle, Lingual nerve, Submandibular ganglion, Hypoglossal nerve
Submandibular duct (Wharton’s duct): Opens lateral to the lingual frenulum on the anterior floor of mouth. , 5 cm length. Lingual nerve wraps around Wharton’s duct. As the duct passes forwards it crosses medial to the nerve to lie above it and then crosses back, lateral to it, to reach a position below the nerve.
Innervation
Sympathetic innervation- Derived from superior cervical ganglion
Parasympathetic innervation- Submandibular ganglion via lingual nerve
Arterial supply: Branch of the facial artery. The facial artery passes through the gland to groove its deep surface. It then emerges onto the face by passing between the gland and the mandible.
Venous drainage: Anterior facial vein (lies deep to the Marginal Mandibular nerve)
Lymphatic drainage: Deep cervical and jugular chains of nodes
What are the effects of injury to the hypoglossal nerve and lingual nerves?
What are the effects of injury to the marginal mandibular branch of the facial nerve?
Injury to the lingual nerve will result in ipsilateral loss of somatic sensation to the anterior two thirds of the tongue. Injury to the hypoglossal nerve will result in atrophy the muscles of the tongue on the ipsilateral side. This can be clinically demonstrated by asking the patient to protrude their tongue, when this is done it will deviate to the side of the lesion.
This branch supplies risorius and the muscles of the lower lip. Therefore, injury to it will potentially result in an ipsilateral weakness of the lip.
All at risk during submandibular gland excision
Submandibular gland:
Relations of the submandibular gland
Superficial: Platysma, deep fascia and mandible, Submandibular lymph nodes, Facial vein (facial artery near mandible), Marginal mandibular nerve, Cervical branch of the facial nerve
Deep: Facial artery (inferior to the mandible), Mylohyoid muscle
Sub mandibular duct, Hyoglossus muscle, Lingual nerve, Submandibular ganglion, Hypoglossal nerve
Submandibular duct (Wharton’s duct): Opens lateral to the lingual frenulum on the anterior floor of mouth. , 5 cm length. Lingual nerve wraps around Wharton’s duct. As the duct passes forwards it crosses medial to the nerve to lie above it and then crosses back, lateral to it, to reach a position below the nerve.
Innervation
Sympathetic innervation- Derived from superior cervical ganglion
Parasympathetic innervation- Submandibular ganglion via lingual nerve
Arterial supply: Branch of the facial artery. The facial artery passes through the gland to groove its deep surface. It then emerges onto the face by passing between the gland and the mandible.
Venous drainage: Anterior facial vein (lies deep to the Marginal Mandibular nerve)
Lymphatic drainage: Deep cervical and jugular chains of nodes
What cartilaginous structures constitute the larynx?
The larynx is a fibrocartilagenous structure that is comprised of 6 different cartilages.
Epiglottis- This broad structure is attached to the posterior aspect of the thyroid cartilage inferiorly. Superiorly, it projects posterior to the hyoid and tongue.
Thyroid- This shield shaped segment consist of two laminae that unite in the midline with the thyroid notch superiorly. Inferiorly, the horns articulate with the cricoid.
Cricoid- This forms a complete ring and is the only complete ring within the larynx. It articulates with both the thyroid and arytenoid cartilages.
Arytenoid- There are two arytenoids, the have a pyramidal shape and sit on the cricoid. Together, they are responsible for tension within the vocal cords.
Corniculate and cuneiform- There are two of each of these cartilaginous structures. Together, the sit in the aryepiglottic fold.
Larynx
The larynx lies in the anterior part of the neck at the levels of C3 to C6 vertebral bodies. The laryngeal skeleton consists of a number of cartilagenous segments. Three of these are paired; arytenoid, corniculate and cuneiform. Three are single; thyroid, cricoid and epiglottic. The cricoid cartilage forms a complete ring (the only one to do so).
The laryngeal cavity extends from the laryngeal inlet to the level of the inferior border of the cricoid cartilage.
Divisions of the laryngeal cavity
Laryngeal vestibule: Superior to the vestibular folds
Laryngeal ventricle: Lies between vestibular folds and superior to the vocal cords
Infraglottic cavity: Extends from vocal cords to inferior border of the cricoid cartilage
The vocal folds (true vocal cords) control sound production. The apex of each fold projects medially into the laryngeal cavity. Each vocal fold includes:
- Vocal ligament
- Vocalis muscle (most medial part of thyroarytenoid muscle)
The glottis is composed of the vocal folds, processes and rima glottidis. The rima glottidis is the narrowest potential site within the larynx, as the vocal cords may be completely opposed, forming a complete barrier.
Muscle/Origin/Insertion/Innervation/Action
Posterior cricoarytenoid: Posterior aspect of lamina of cricoid–> Muscular process of arytenoid. Recurrent Laryngeal - Abducts vocal fold
Lateral cricoarytenoid: Arch of cricoid–> Muscular process of arytenoid. Recurrent laryngeal - Adducts vocal fold
Thyroarytenoid: Posterior aspect of thyroid cartilage –> Muscular process of arytenoid. Recurrent laryngeal - Relaxes vocal fold
Transverse and oblique arytenoids: Arytenoid cartilage –> Contralateral arytenoid. Recurrent laryngeal - Closure of intercartilagenous part of the rima glottidis
Vocalis: Depression between lamina of thyroid cartilage –> Vocal ligament and vocal process of arytenoid cartilage. Recurrent laryngeal - Relaxes posterior vocal ligament, tenses anterior part
Cricothyroid: Anterolateral part of cricoid –> Inferior margin and horn of thyroid cartilage. External laryngeal - Tenses vocal fold
Blood supply
Arterial supply is via the laryngeal arteries, branches of the superior and inferior thyroid arteries. The superior laryngeal artery is closely related to the internal laryngeal nerve. The inferior laryngeal artery is related to the inferior laryngeal nerve. Venous drainage is via superior and inferior laryngeal veins, the former draining into the superior thyroid vein and the latter draining into the middle thyroid vein, or thyroid venous plexus.
Lymphatic drainage
The vocal cords have no lymphatic drainage and this site acts as a lymphatic watershed.
Supraglottic part: Upper deep cervical nodes
Subglottic part: Prelaryngeal and pretracheal nodes and inferior deep cervical nodes
The aryepiglottic fold and vestibular folds have a dense plexus of lymphatics associated with them and malignancies at these sites have a greater propensity for nodal metastasis.
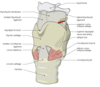
Please name the intrinsic muscles of the larynx.
The function of the intrinsic muscles is to alter the tension of the vocal cords during speech. They open the cords during inspiration and close them during swallowing. They comprise:
Posterior cricoarytenoid- Abducts the cords and externally rotates the arytenoids
Lateral cricoarytenoid- Adducts the cords and internally rotates the arytenoid
Interarytenoid- Adducts the cords and closes the glottis. It is unpaired.
Thyroarytenoid- Shortens the vocal cords by drawing arytenoids forward
Vocalis- Arises from the thyroarytenoid and alters vocal cord tension
Cricothyroid- Lifts the cricoid anteriorly towards the thyroid cartilage. It lengthens the vocal cords
Larynx
The larynx lies in the anterior part of the neck at the levels of C3 to C6 vertebral bodies. The laryngeal skeleton consists of a number of cartilagenous segments. Three of these are paired; arytenoid, corniculate and cuneiform. Three are single; thyroid, cricoid and epiglottic. The cricoid cartilage forms a complete ring (the only one to do so).
The laryngeal cavity extends from the laryngeal inlet to the level of the inferior border of the cricoid cartilage.
Divisions of the laryngeal cavity
Laryngeal vestibule: Superior to the vestibular folds
Laryngeal ventricle: Lies between vestibular folds and superior to the vocal cords
Infraglottic cavity: Extends from vocal cords to inferior border of the cricoid cartilage
The vocal folds (true vocal cords) control sound production. The apex of each fold projects medially into the laryngeal cavity. Each vocal fold includes:
- Vocal ligament
- Vocalis muscle (most medial part of thyroarytenoid muscle)
The glottis is composed of the vocal folds, processes and rima glottidis. The rima glottidis is the narrowest potential site within the larynx, as the vocal cords may be completely opposed, forming a complete barrier.
Muscle/Origin/Insertion/Innervation/Action
Posterior cricoarytenoid: Posterior aspect of lamina of cricoid–> Muscular process of arytenoid. Recurrent Laryngeal - Abducts vocal fold
Lateral cricoarytenoid: Arch of cricoid–> Muscular process of arytenoid. Recurrent laryngeal - Adducts vocal fold
Thyroarytenoid: Posterior aspect of thyroid cartilage –> Muscular process of arytenoid. Recurrent laryngeal - Relaxes vocal fold
Transverse and oblique arytenoids: Arytenoid cartilage –> Contralateral arytenoid. Recurrent laryngeal - Closure of intercartilagenous part of the rima glottidis
Vocalis: Depression between lamina of thyroid cartilage –> Vocal ligament and vocal process of arytenoid cartilage. Recurrent laryngeal - Relaxes posterior vocal ligament, tenses anterior part
Cricothyroid: Anterolateral part of cricoid –> Inferior margin and horn of thyroid cartilage. External laryngeal - Tenses vocal fold
Blood supply
Arterial supply is via the laryngeal arteries, branches of the superior and inferior thyroid arteries. The superior laryngeal artery is closely related to the internal laryngeal nerve. The inferior laryngeal artery is related to the inferior laryngeal nerve. Venous drainage is via superior and inferior laryngeal veins, the former draining into the superior thyroid vein and the latter draining into the middle thyroid vein, or thyroid venous plexus.
Lymphatic drainage
The vocal cords have no lymphatic drainage and this site acts as a lymphatic watershed.
Supraglottic part: Upper deep cervical nodes
Subglottic part: Prelaryngeal and pretracheal nodes and inferior deep cervical nodes
The aryepiglottic fold and vestibular folds have a dense plexus of lymphatics associated with them and malignancies at these sites have a greater propensity for nodal metastasis.

Please name the extrinsic muscles of the larynx.
These attach the larynx to adjacent structures and serve to elevate or depress it. They comprise:
Sternothyroid, thyrohyoid and the inferior constrictor.
Larynx
The larynx lies in the anterior part of the neck at the levels of C3 to C6 vertebral bodies. The laryngeal skeleton consists of a number of cartilagenous segments. Three of these are paired; arytenoid, corniculate and cuneiform. Three are single; thyroid, cricoid and epiglottic. The cricoid cartilage forms a complete ring (the only one to do so).
The laryngeal cavity extends from the laryngeal inlet to the level of the inferior border of the cricoid cartilage.
Divisions of the laryngeal cavity
Laryngeal vestibule: Superior to the vestibular folds
Laryngeal ventricle: Lies between vestibular folds and superior to the vocal cords
Infraglottic cavity: Extends from vocal cords to inferior border of the cricoid cartilage
The vocal folds (true vocal cords) control sound production. The apex of each fold projects medially into the laryngeal cavity. Each vocal fold includes:
- Vocal ligament
- Vocalis muscle (most medial part of thyroarytenoid muscle)
The glottis is composed of the vocal folds, processes and rima glottidis. The rima glottidis is the narrowest potential site within the larynx, as the vocal cords may be completely opposed, forming a complete barrier.
Muscle/Origin/Insertion/Innervation/Action
Posterior cricoarytenoid: Posterior aspect of lamina of cricoid–> Muscular process of arytenoid. Recurrent Laryngeal - Abducts vocal fold
Lateral cricoarytenoid: Arch of cricoid–> Muscular process of arytenoid. Recurrent laryngeal - Adducts vocal fold
Thyroarytenoid: Posterior aspect of thyroid cartilage –> Muscular process of arytenoid. Recurrent laryngeal - Relaxes vocal fold
Transverse and oblique arytenoids: Arytenoid cartilage –> Contralateral arytenoid. Recurrent laryngeal - Closure of intercartilagenous part of the rima glottidis
Vocalis: Depression between lamina of thyroid cartilage –> Vocal ligament and vocal process of arytenoid cartilage. Recurrent laryngeal - Relaxes posterior vocal ligament, tenses anterior part
Cricothyroid: Anterolateral part of cricoid –> Inferior margin and horn of thyroid cartilage. External laryngeal - Tenses vocal fold
Blood supply
Arterial supply is via the laryngeal arteries, branches of the superior and inferior thyroid arteries. The superior laryngeal artery is closely related to the internal laryngeal nerve. The inferior laryngeal artery is related to the inferior laryngeal nerve. Venous drainage is via superior and inferior laryngeal veins, the former draining into the superior thyroid vein and the latter draining into the middle thyroid vein, or thyroid venous plexus.
Lymphatic drainage
The vocal cords have no lymphatic drainage and this site acts as a lymphatic watershed.
Supraglottic part: Upper deep cervical nodes
Subglottic part: Prelaryngeal and pretracheal nodes and inferior deep cervical nodes
The aryepiglottic fold and vestibular folds have a dense plexus of lymphatics associated with them and malignancies at these sites have a greater propensity for nodal metastasis.