Mod IV: Regional Anesthesia Part 5 Flashcards
Regional Anesthesia - Locating Nerves
How to find what your looking for?
Apply that Anatomy
Knowledge of nerve path, surrounding structures, and surface landmarks is of paramount importance
Regional Anesthesia - Locating Nerves
Techniques used to localize nerves
Landmarks - Paresthesia - Nerve Stimulator
Ultrasound - Fluoroscopy
CT guided
Regional Anesthesia - Locating Nerves
Nerve localization technique that provides both still and live x-ray views:
Fluoroscopy
Used primarily in pain blocks
Expensive
Regional Anesthesia - Locating Nerves
Nerve localization technique that provides still and live Ct images:
Ct guided
Used rarely in pain blocks
Extremely expensive!!!
Regional Anesthesia - Locating Nerves
Techniques for locating nerves that use surface landmarks and knowledge of anatomical relationships:
Landmark Techniques

Regional Anesthesia - Locating Nerves
Using Landmarks alone can help anesthetized which structures?
Ankle
Digits
Cervical plexus

Regional Anesthesia - Locating Nerves
Landmark Techniques can be combined with:
Paresthesia
Nerve Stimulator
Ultrasound
Regional Anesthesia - Locating Nerves
The feeling of tingling, tickling, burning, prickling, or buzzing felt is also known as:
Paresthesia
Regional Anesthesia - Locating Nerves
What’s the goal of Paresthesia technique?
To place the needle in direct contact with the desired nerve to produce a Paresthesia
This tells the practitioner they are very close or in the target nerve, then withdraw slightly until paresthesia stops and inject LA
NEVER inject LA if pt has sharp PAIN or PARESTHESIA!!!
The elicited paresthesia should follow the target nerves distribution
Old technique still used by some practitioners
Regional Anesthesia - Locating Nerves
What are disadvantages of the Paresthesia technique?
Risk of neural injury
Higher block failure rates when compared to newer techniques
Regional Anesthesia - Locating Nerves
Nerve localization technique that uses electricity to produce a response of a target nerve:
Nerve Stimulator Technique
Used in combination with anatomical and surface landmark knowledge
Motor –Target nerve muscles twitch
Sensory – paresthesia over target nerve distribution

Regional Anesthesia - Locating Nerves
Membrane potentials - What’s Resting MP?
– 90 mV

Regional Anesthesia - Locating Nerves - Membrane potentials
What’s Threshold Level? what happens when it’s reached by a stimulus?
– 55mV
Depolarization occurs
Propagation of Action potential
Regional Anesthesia - Locating Nerves
How does Nerve Stimulator work?
Negative Polarity Impulse
Neutralizes positive current outside nerve dropping MP
Black lead attached to needle
Red positive lead is attached to skin

Regional Anesthesia - Locating Nerves
Which nerves have Lowest Threshold of Ext Stim to generate AP? why?
Motor nerves
B/c Highly myelinated nerves

Regional Anesthesia - Locating Nerves
Which nerves have Higher Threshold for External Stim to generate AP? why?
Sensory nerves
B/c Unmyelinated nerves – slower

Regional Anesthesia - Locating Nerve - Generating a Action Potential
Which characteristics of a stimulus determine generation of an Action Potential?
Stimulus Strength and Duration

Regional Anesthesia - Locating Nerves
Generating a Action Potential - Strength of electrical stimulus is also known as:
Current Amplitude

Regional Anesthesia - Locating Nerves
The amount of time a stimulus must be applied to generate an Action Potential is known as:
Current Duration
Regional Anesthesia - Locating Nerves
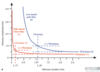
Generating a Action Potential - Impulses of which duration are better discriminator of distance?
Short duration impulses
Regional Anesthesia - Locating Nerves
Motor impulse duration:
0.1 ms

Regional Anesthesia - Locating Nerves
Sensory impulse duration:
0.3 ms
Longer duration needed to reach threshold level

Regional Anesthesia - Locating Nerves
Nerve stimulator - Frequency:
1-2 Hz
Regional Anesthesia - Locating Nerves
Nerve stimulator - Duration:
- 1ms Motor
- 3 ms Sensory
Regional Anesthesia - Locating Nerves
Nerve stimulator - Amplitude - Start stimulator at which mA?
1-1.5 mA
Position needle => twitch
↓ mA, and adjust needle position …
Regional Anesthesia - Locating Nerves
Nerve stimulator - Amplitude - What’s the goal?
Goal is loss of motor response 0.3-0.5mA
Indicates that the tip of the block needle is in correct position
Never inject <0.3mA
(0.2mA by some sources)
Regional Anesthesia - Locating Nerves
Nerve stimulator - Why is Reliability a Problem?
74.5% sensitivity for needle to nerve contact
25% NO muscle twitch
even when needle actually touching nerve!!
Regional Anesthesia - Locating Nerves
Nerve stimulator - Reliability is a Problem. However Twitch present at:
0.2-0.3mA
ALWAYS INTRANURAL!!
Regional Anesthesia - Nerve stimulator
Technique of Locating Nerves with Series of 3 pulses (3Hz frequency), also known as:
Sequential Electrical Nerve Stimulation
(SENSe Mode)

Regional Anesthesia - Nerve stimulator
Sequential Electrical Nerve Stimulation aka SENSe Mode - Technique:
Series of 3 pulses (3Hz frequency)
2 short: 0.1ms
1 longer: duration increases with Amplitude
0.2ms @ 0.3mA
0.42ms @ 1mA
0.84ms @ 2mA
Longer pulse reaches further in tissue
Regional Anesthesia - Nerve stimulator
Use of Sequential Electrical Nerve Stimulation aka SENSe Mode:
Single twitch achieved
Needle optimized until 3 twitches present
Goal: current 0.3 – 0.5mA with 3 twitches

Regional Anesthesia - Locating Nerves
Stimulating Needles:
Insulated
Direct current at the tip for precise nerve location
Blunt Bevel

Regional Anesthesia - Locating Nerves
Technique of locating nerves that provides real time imaging of target nerves, related structures, LA injection
Ultrasound Guidance
1978 1st case report of using US for regional

Regional Anesthesia - Locating Nerves
US guidance has greatly improved as evidenced by:
Block success
Speed of onset
Anesthetic quality of block
Becoming the gold standard in block placement!!!
Regional Anesthesia - Locating Nerves
What are arguments againts US guidance?
Steep learning curve
Adds to much time to blocks
Cost of machine
No need, “…my blocks don’t fail”
Regional Anesthesia - Locating Nerves
How is US image generated?
Piezoelectric Material in Probe
Electricity => material => sound waves
Sound waves => material => electricity
100 – 300 crystals in a Probe
Send out cyclical pulses of US energy and measures reflected energy that travels back to the probe
Reflected energy produces the US image you see
Probe talks (2%) and listens (98%)
The sum of all the crystals creates the US beam

Regional Anesthesia - Locating Nerves
US probe talks (xx%) and listens (yy%)
Talks (2%)
Listens (98%)

Regional Anesthesia - Locating Nerves - Ultrasound Guidance
When US encounters boundaries some energy is reflected back at the probe and the rest transmitted. What you see is called:
Reflection
This is what we see
Regional Anesthesia - Locating Nerves - Ultrasound Guidance
Degradation of US by rough surfaces and heterogeneous material is also known as:
Scatter
Regional Anesthesia - Locating Nerves - Ultrasound Guidance
Conversion of US into heat; This is where majority goes and it is also known as:
Absorption
Regional Anesthesia - Locating Nerves - Ultrasound Guidance
Does Absorption of US waves using modern US machines poses any risk to pts?
There has never been any documented biological risk to Pts
Regional Anesthesia - Locating Nerves - Ultrasound Guidance
Degradation of US wave in tissue is also known as:
Attenuation
Higher frequency US energy degredates more quickly
Regional Anesthesia - Locating Nerves - Ultrasound Guidance
Higher frequency US energy degredates more quickly. What’s the clinical significance of this?
Use Higher frequency probes only for superficial structures
Lower Frequency probe are Better for deep structures
Regional Anesthesia - Locating Nerves - Ultrasound Guidance
The number of sound waves per sec is also known as:
Frequency
2 – 15 MHz commonly used in US
Human ear 20Hz – 20 kHz

Regional Anesthesia - Locating Nerves - Ultrasound Guidance
Distance between wave peaks:
Wavelength
Inversely related to Frequency
Primary determinant of lateral and axial resolution
Temporal resolution is related to frame rate (typically 30 frames/sec)

Regional Anesthesia - Ultrasound Guidance - Probe Selection
Higher Frequency Probes are also known as:
Linear Probes
Better resolution of superficial structures
Up to 6 cm deep
For superficial nerve blocks and Vascular access.
IJ line, ISB, Femoral, etc

Regional Anesthesia - Ultrasound Guidance - Probe Selection
Lower Frequency probes are also known as:
Curvilinear Probes
AKA – Phase Array
Visualize deeper structures
To 14 cm deep
For deeper structure Nerve blocks and Musculoskeletal assessment
Sciatic nerve, TAPs, Neuraxial assessment

Regional Anesthesia - Ultrasound Guidance - US Modes
The US mode that displays the 2D imaging we see today is also known as”
B-Mode
(Brightness)
What you will typically use

Regional Anesthesia - Ultrasound Guidance - US Modes
The US mode that displays Image of Movement over Time is also known as:
M-Mode
Useful in assessment of specific tissues
Heart valves, Lung

Regional Anesthesia - Ultrasound Guidance - US Modes
The change in sound waves resulting from relative motion between source and receiver is also known as:
Doppler Effect

Regional Anesthesia - Ultrasound Guidance - Doppler Mode
Red Color indicates flow moving in which direction?
Flow coming toward probe
Moving Toward Receiver
Higher Pitch
Useful for Vascular identification
Regional Anesthesia - Ultrasound Guidance - Doppler Mode
Blue Color indicates flow moving in which direction?
Flow moving Away from probe
Moving Away from receiver
Lower Pitch
Useful for Vascular identification
Regional Anesthesia - Ultrasound Machine
Knob that allows for optimal depth adjustment important for focusing image
Depth knob
Limited to probe selected
Regional Anesthesia - Ultrasound Machine
Knob on Newer machines that can automaticaly focus
Focus knob
May have to set depth to focus on
Regional Anesthesia - Ultrasound Machine
Knob that allows to adjust Brightness of image on screen
Gain knob
Some machines allow for gain to be adjusted at different depths independently
Regional Anesthesia - Ultrasound Machine
Knob used to aid in detecting vascular structures
Doppler knob
Regional Anesthesia - Ultrasound Guidance
What Nerves Look Like? Nerve shapes:
Round, oval, triangular

Regional Anesthesia - Ultrasound Guidance
Images from US could have which three appearances?
Hyper-echoic
Hypo-echoic
Honeycomb

Regional Anesthesia - Ultrasound Guidance
What are possible US Image Artifacts?
Shadowing
Enhancement
Reverberation
Mirror image
Velocity Error

Regional Anesthesia - Ultrasound Guidance - Image Artifact
A significant reduction of image below solid objects is known as:
Shadowing

Regional Anesthesia - Ultrasound Guidance - Image Artifact
Overly intense echogenicity behind an object (Blood vessel, cyst) is known as:
Enhancement

Regional Anesthesia - Ultrasound Guidance - Image Artifact
Equally spaced bright linear echoes below an object is known as:
Reverberation

Regional Anesthesia - Ultrasound Guidance - Image Artifact
Objects appearing on both sides of a highly reflective interface represents which artifact?
Mirror image

Regional Anesthesia - Ultrasound Guidance - Image Artifact
Visual displacement of interface due to difference in actual US velocity versus celebrated speed (1540 m/sec) is known as:
Velocity Error
Regional Anesthesia - Ultrasound Guidance
What are the two axial options for maping a structure?
Short Axis
Long Axis

Regional Anesthesia - Ultrasound Guidance - Imaging a structure
A Cross sectional or Transverse view represents which axis?
Short Axis view

Regional Anesthesia - Ultrasound Guidance - Imaging a structure
A Longitudinal view represents which axial view?
Long Axis view

Regional Anesthesia - Ultrasound Guidance
Needle Approaches:
In Plane
Out of Plane

Regional Anesthesia - Ultrasound Guidance
Professor’s Practice using US - Nerve Block:
Short axis View
Needle In Plane
Injection of LA under direct visualization
Placement of Catheter directly visualized

Regional Anesthesia - Ultrasound Guidance
Professor’s Practice using US - Vascular Access:
Short Axis
Out of Plane



