Microvascular Complications of Diabetes - Retinopathy Flashcards
diabetic retinopathy
damage to the retina and iris caused by diabetes which can lead to blindness
is associated with several complications (cataract, glaucoma, acute hyperglycaemia)
cataracts
the denuration of protein and other components of the lens of the eye render it opaque
develops early in people with diabetes, and can be reversed with return to normoglycaemia

glaucoma
the increase in fluid pressure in the eye lead to optic nerve damage
2x more likely in DM
acute hyperglycaemia
visual blurring
- acute short sightedness is a possible acute presentation of DM
- reversible once normoglycaemia established
symptoms of diabetic retinopathy
tend to be mild initally (eg visual burring or dark spots/floaters)
however, can be more serious (eg sudden onset of blindness)
what are the stages defined by
pathology, rather than symptoms/clinical presentation
diabetes without retinopathy
underlying hyperglycaemia causes damages to pericytes in the retina that are important in regulating blood flow. damage to them is caused by an inability to properly metabolise glucose - osmotic damage

what are the signs of diabetes without retinopathy
likely present in most individuals who have had diabetes for a few years, not detectable on eye exam
no signs of retinopathy, but underlying damage
non proliferative retinopathy
damage to retinal pericytes causes weakening of capillary wall and increased blood flow - formation of microaneurysms
- these appear as red dots and are typically the first clinical sign
damage to pericytes also increases vascular permeability (leaky capillaries), this means proteins and lipids can leak out into retinal tissue and are trapped - form hard exudates (yellow/white flecks on retina)

at what stage does non-proliferative retinopathy usually occur
25 years after DM diagnosis
is non proliferative retinopathy symptomatic
may or may not be
proliferative retinopathy
characterised by vascular proliferation within the retina - this is the retina trying to compensate for ischaemia due to retinal damage. produces a groth factor (VEGF) which produces new blood vessels
however, these are abnormal and do not compensate for ischaemia

symptoms of proliferative retinopathy
uncommonly asymptomatic
usually patients at least have blurry vision and floaters
prognosis
once diabetic retinopathy is proliferative, prognosis is poor and unpredictable
can result in vision threatening complications
maculopathy
damage to the macula
suspected when acuity (clarity of vision) is decreased
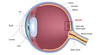
macula
surrounds the fovea - portion of retina with highest density of cones (colour and high resolution image)
when would one refer maculopathy
lesions (specified below) are within a radius of <1 disc diameter of the centre of the fovea
- blot haemorrhages
- hard exudates
diabetic retinopathy treatment
laser
vitrectomy (remocal of vitreous gel from middle of eye)
anti-VEGF (growth factor) injections

laser burns on retina
background retinopathy criteria
- at least 1 dot haemorrhage or microaneurysms with/out hard exudate
- cotton wool spot
- <4 blot haemorrhages
- review in one year

moderate diabetic retinopathy criteria
- ≥4 haemorrhages
- rescreen in 6 months



