Management cards (Slide exam) Flashcards
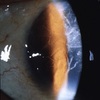
Name, mx (3)

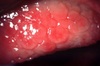
Conjunctival papilloma
Patient reassurance, optional surgery for cosmesis, general ddx (check FAT, feeder blood vessels, surround tissue invasion, biopsy)
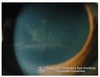
.Name, mx (2)

CIN (conjunctival intraepithelial neoplasia):
Mx: surgery for removal, general ddx
Name, mx (1)

SCN:
Mx: surgery for removal, ddx
How should you manage any unusual/unepected growth on the eye (e.g. the ones in the image) or adnexa? (4)

- Check for fast development/spread (e.g. with FAT)
- Check amount of feeder blood vessels
- Check for surrounding tissue invasion
- Refer for biopsy as needed
.Name, mx (1)

Naevus: Benign ocular pigmented lesion
Mx: refer for biopsy if suspicious
Name, mx (1)

Congenital melanocytosis
Mx: (if malignant) refer for excision + biopsy
Name, When is a biopsy indicated? (2)

Primary Acquired Melanosis (PAM):
Biopsy indicated if: - diffuse lesion found at limbus + corneal involvement; - expansive/overgrowth of diffuse lesion in one eye (which shows its pleomorphic)
Name, Biopsy appearance (1), mx (1)

Melanoma
biopsy: invasive lesion with pleomorphism and anaplasia
Mx: surgical removal
Name, mx (2)

Telangiectasia:
Mx: surgery for cosmesis, tx any assoc. systemic conditions (e.g. sturge-weber, HHT)
Name, mx (7)
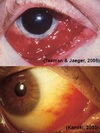
Kaposi’s sarcoma:
Mx: refer for diagnostic workup if AIDS dx unknown, or for therapy (e.g. HAART - highly active anti retroviral therapy) if AIDS present.;
Tx often palliative (i.e. relieve symptoms/pain), surgery, focal radiation, anti-mitotics, AIDS protease inhibitors
Name, mx (4)

Sturge-Weber Syndrome
Mx: consider referral for ax of neurological status; follow up appt. in 3-12 months to check for glaucoma; if choroidal hemangioma present = check for signs of retinal detachment. If choroidal hemangioma grows into central vision, leaks or causes detachment: tx it by laser or radiation
.Name, define, mx (1)

Cavernous sinus fistula:
.- Break in the cavernous sinus- i.e. “fistula” = break in wall of an artery –> causing higher arterial blood to enter venous space—-
Mx: refer for closure of fistula + mx of IOP
.Name, mx (4)

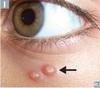
Cyst of Moll/sweat glands
Excision for cosmesis
• Pouching of small hydrocystoma
• Refer for excision
• Lidnocaine as skin anaesthetic before pouching
Name, mx (3)

Cyst of Zeis Gland - Opaque lesion
Mx: pouching incision, curettage, refer for excision
(note: curretage = Removal of tissue with a curette from the wall of a cavity or another surface)
Name, mx (4)

Stye/Hordeolum
Mx: Warm compress, Most resolve 2-3 days, Topical broad spectrum antibiotic (chlorsig) if persistent, Can lead to cellulitis (indicated by fever and V.A) –> that requires antibiotics tx
Name, mx (5)

Chalazion
Mx: spontaneous resolution in few months (when fluid resorbed), Tx = heat compress (qid), lid massage (to help glands open + soften oil), incision w/curettage + steroid injection (long lasting), doxycline if recurrent (40-100mg bid) or tetracycline (500mg bid)
Name, mx (3)

Sebaceous gland carcinoma: malignant tumour of sebaceous gland
Mx: careful examination, review with referral of suspicious cases, 6-12 monthly reviews
Name, mx (1)

Viral Warts (Verruca)
Mx: refer for excision + cautery
Name, Ax (2), Mx (3)
Molluscum contagiosum
Ax: check eyebrows and evert; ensure no lymphadenopathy, check lymph nodes
Mx: counsel about hygeine, spread skin-skin contact; self-limiting, non-scarring; refer for excision + cauterisation
name, ax (1), mx (3)

Keratoacanthoma
Ax: biopsy of keratin core
Mx: refer for excision + biopsy; exclude SCC; spontaneous involuted by one year
Name, mx (4)

Xanthelasma
refer to GP to manage systemic overlay
check /control lipid levels (TGs, cholesterol),
systemic work up (fasting blood lipids)
Consider excision for cosmesis(recurrent) + refer for biopsy (to make sure it’s benign)
Name, Ax (1), Mx (1)

Seborrheic Keratosis (SK):
Ax: referral for excision and biopsy (if suspicious)
Mx: progressive, suspicious or cosmesis excise excluding BCC, SCN
Solar or Actinic Keratosis. How do you manage it? (3)
malignant potential
photos to monitor
refer for biopsy & excision (exclude BCC, SCC)

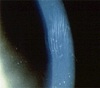
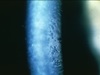
Epithelial Basement Membrane Dystrophy (EBMD): Mx (4)
Lubricants; Mx of any co-existing surface disease if there are any symptoms; mx of any pre-existing erosion;
any co-existing surface disease will increase the risk of recurrent corneal erosions.