Male Pathology Flashcards
The most common malformations of the oenis include abnormalities in the location of the distal urethral orifice, termed hypospadias (more common) where the urethra is on the ventral aspect and epispadias, where teh urethral orifice is on the dorsal side

What are the associations of hypospadias?
the urethral orifice can be obstructed, resulting in urinary tract obstruction and an increased risk of UTIs
inguinal hernias and undescended testes
What are the associations of epispadias?
anterior abdominal wall defects including extrophy of the bladder
What is Phimosis?
represents a condition in which the prepuce cannot be retracted easily over the glans penis that can lead to the accumulation of smegma and possible infection. This is a small risk of squamous cell carcinoma of the penis in these pts.
This can occur congenitally, but most cases are acquired from scarring to the prepuce to previous episodes of balanosposthitis
What are balanitis and balanosposthitis?
These refer to local inflammation of the glans penis and over the overlying prepuce, respectively.
What are some common causes of balanitis and balanosposthitis?
Candida albicans, anaerobs, Gardnerella, ad pyogenic bacteria. Most cases occur due to poor hygiene in uncircumscribed males
What is Peyronies Disease?
benign local growth of fibrous plaque located inside the tunica albuginea of the penis that causes an upward (usually) curvature. Mostly cosmetic, but up to half can experience pain with erection

More than 95% of penile neoplasms arise where?
on squamous epithelium, aka squamous cell carcinomas of the penis (although these are rare in developed countries). Most cases occur in uncircumscribed males over 40
What are the risk factors for squamous cell carcinoma of the penis?
poor hygiene with smegma
smoking
HPV infection, particularly 16/18
What is Penile intraepithelial neoplasia?
is a rare pre-cancerous disease of the outer skin layer (epidermis) of the penis. This ‘group’ includes:
Bowenoid papulosis
Erythroplasia of Queyrat
What is Bowen disease (aka Erythroplasia of Querat)?
squamous cell carcinoma in situ of the penis associated with HPV. Typically occurs in older uncircumcised males and appears grossly as a solitary plaque on the penis shaft


What is Bowenoid papulosis?
a cutaneous pre-cancerous condition that presents as single or multiple small, red, brown or flesh-coloured spots or patches on the genitals of males and females. They are associated with human papillomavirus, the causative agent of genital warts. The lesions have a typical dysplastic histology and are generally considered benign, although a small percentage will develop malignant characteristics.
The presence of keratin swirls helps define it as a squamous cell carcinoma

What is cryptorchidism?
a failure of testicular descent into the scrotum, Normally, the testes descend from teh abdominal cavity into the pelvis by the 3rd month, and then trhough the inguinal canals into the scrotum during the last 2 months of gestation.
When can the diagnosis of cryptorchidism be made?
Only after age 1, because often times thr process is not complete at birth. It has an incidence of 1% of live male births, particularly in premature infants. Most cases are idiopathic
What risks are associated with cyrptorchidism?
In addition to infertility, failure of descent is associated with a 3- to 5-fold increased risk of testicular cancer. Orchiopexy reduces the risk of sterility and cancer.
Inflammatory lesions of the testes are more common where?
in the epididymis rather than the testis proper
What are the main causes of testicular inflammation?
-STIs
- Other causes of testicular inflammation include nonspecific epididymitis and orchitis, mumps, and tuberculosis.
- Nonspecific epididymitis and orchitis usually begins as a primary urinary tract infection that then spreads to the testis through the vas deferens or the lymphatics of the spermatic cord - predominantly neutrophilic infiltrate.
- Orchitis complicates mumps infection in roughly 20% adult males but rarely occurs in children - lymphoplasmacytic inflammatory infiltrate
- Tuberculosis = granulomatous inflammation and caseous necrosis
What is torsion?
twisting of the spermatic cord, which typically results in obstruction of testicular venous drainage while leaving the arteries patent so that venous infarction occurs unless it is relieved.
What are the types of torsion?
neonatal and adult
How is adult torsion different from neonatal?
Adult torsion manifests with sudden onset of testicular pain and results from a bilateral anatomic defect whereby the testis has increased mobility, giving rise to the so-called bell clapper abnormality. it often occurs without injury
This is a surgical emergency and needs to be fixed within 6 hrs

How common are testicular neoplasms?
Incidence of about 0.006%, but are the most common tumors of men in the 15-34 age group. These are solid on ultrasound and typically present as a painless mass
Where do testicular neoplasms msot commonly arise from?
Almost 95% in postpubertal males arise from germ cells and all of these are malignant, whereas neoplasms arising from Sertoli/Leydig cells (sex cord-stromal tumors) are usually benign.
All testicular cancers are more common in white men than black
Again, ______ raises the risk for testicular cancer 3-5x
cryptorchidism (raises the risk in BOTH testes)
Other risk factors: Fam Hx, contralateral neoplasm, i(12p) mutations in germ cell mutations
testicular germ cell tumors are subclassified into what?
seminoma and nonseminoma germ cell tumors
Describe seminomas
These have a good prognosis, dont met until late (through lymph to abdomen- nonseminomatous germ cell tumors tend to spread via blood to lung).
How do seminomas appear histo wise?
These have a fried-egg appearance on histo exam and are characterized in approximately 15% of cases by syncytiotrophoblasts (these minimally elevate serum hCG concentrations- so these men might have a positive pregnancy test!!)

What are some nonseminoma germ cell tumors of the testes?
- embryonal carcinoma
- yolk sac tumor
- choriocarcinoma
Describe embryonal carcinomas
These are masses that contain foci of hemorrhage and necrosis. The primary lesions may be small, even in pts. with mets at the time of discovery. Histologically, the tumor cells are large and have very basophilic cytoplasm and prominent nucleoli

Describe yolk sac tumors
These are the most common primary testicular neoplasm is children younger than 3. These are somewhat aggresive but have a good prognosis
What is this?

Histo of a yolk sac tumor- these often have eosinophilic hyaline globules in which α 1 -antitrypsin and alpha fetoprotein (AFP) can be demonstrated.
Describe what is being shown in this yolk sac tumor

•Areas of loosely textured, microcystic tissue and papillary structures resembling a developing glomerulus (Schiller-Duval bodies).
What is this?

Choriocarcinomas- these are fairly aggressive and are marked by large amounts of hemorrhage and necrosis.
Both cytotrophoblastic cells with central nuclei ( arrowhead, upper right ) and syncytiotrophoblastic cells with multiple dark nuclei embedded in eosinophilic cytoplasm ( arrow, middle ) are present.
____ serum markers will be elevated in a choriocarcinoma
hCG
What is a teratoma?
tumor composed of mature cells from endodermal, mesodermal, and ectodermal lines
What is the pt. population for testicular teratomas?
Pure forms of teratoma are fairly common in infants and children, second in frequency only to yolk sac tumors.
In adults, pure teratomas are rare, constituting 2% to 3% of germ cell tumors, and as with embryonal carcinomas, most are seen in combination with other histologic types.
Are testicular teratomas mostly benign or malignant?
Elements may be mature (resembling various tissues within the adult) or immature (sharing histologic features with fetal or embryonal tissues – more aggressive)
Any age (prepubertal males -typically benign, postpubertal males are malignant)


Most hyperplastic lesions arise in the inner transition zone, while most carcinomas arise in the peripheral zones

The normal prostate contains glands with two cell layers, a flat basal cell layer and an overlying columnar secretory cell layer. Surroundng prostatic stroma contains a mixture of smooth msucle and fibrous tissue.
What are the categories of prostatitis?
1) acute bacterial (2-5% of cases)
2) chronic bacterial
3) chronic nonbacterial prostatitis, or chronic pelvic pain syndrome (90-95% of cases)
4) asymptomatic inflammatory prostatitis
T or F. The prostate is usually not biopsed in men with prostatitis
T.
How does prostatitis present?
commonly with fever, chills, and dysuria, and can be complicated by sepsis. The prostate is often tender on rectal exam
Chronic bacterial prostatitis is often associated with recurrent UTIs
Common causes of bacterial prostatitis
In younger people, sexually transmitted infections are suspected while E.coli is a common cause in older men

What is BPH?
Proliferation of both stromal and epithelial elements of the prostate with resultant glandular enlargement primarily related to excessive or un-regulated action of DHT
- BPH nodules can compress the prostatic urethra.
- Clinical symptoms include hesitancy, urgency, nocturia, and poor urinary stream.
- Chronic obstruction predisposes to recurrent urinary tract infections.
Where does BPH typically occur?

transitional zone
Epidemiology of Prostate adenocarcinoma
These are the most common cancer in men, second most common cause of death, less than that for cancers of the lung and equal to that for colorectal cancer.
Note that the progressin of prostatic cancers is VERY variable, with some being agressive and others being indolent
Describe the pathogenesis of prostate cancer
Androgens are of central importance and are required for development of a prostatic tumor (but note that some can acquire mutations that make it hormonally independent)
- Fam Hx (highest in blacks)- associated with MYC mutations in blacks
- Environment and diet
What acquired mutations may lead to increased risk of a prostatic adenocarcinoma?
TMPRSS2-ETS fusion proteins or inactivating mutations in PTEN (which normally downregulates P13K/AKT pathways)

Notes about prostatic adenocarcinoma
This picture is of a low-grade lesion. These tumors like to wrap are neural tissue, and metastasize to bone to produce blastic/sclerotic lesions

Usually Grade 3 isnt that bad

prostatic adenocarcinoma where the carcinoma cells on the left are the dark purple ones


Prostatic adenocarcinoma- pts suspected will get a core biopsy

Prostatic cancers arise in what part of the prostate?
peripheral zone (and hence may be palpable as irregular hard nodules on rectal exam). However, most prostate cancers are small, nonpalpable, asymptomatic lesions discovered on needle biopsy performed to investigate an elevated PSA
Clinical features of prostate carcinoma
Because of its peripheral location, these are less likely than BPH to cause urethral obstruction in its initial stages
Describe PSA
The PSA assay is the most important test used in prostatic cancer diagnosis (but is limited in many ways!). PSA is a product of prostatic epithelium and is normally secreted in semen.
In most labs, the cutoff between normal and abnormal is 4 ng/mL (although some use 2.5)
What are the limitations of PSA screening?
- some prostatic cancers are not worth treating (but no way to know!)
- while it is organ specific, it is not cancer-specific (BPH, prostatitis, and ejaculation all raise PSA levels). AND not all confirmed prostatic cancers even have elevated PSAs!
What is a way that PSA measurement can be improved for prostatic cancer diagnosis?
Instead of just elevated levels, it is more accurate to use the RATE of increase, which is better correlated with prostatic cancer AND
the percentage of free PSA is lower in men with prostate cancer than in men with benign prostatic diseases
How is Prostatic cancer tx?
the most common tx for localized cancer is radical prstatectomy and radiotherapy. In some sub-groups (older men, younger men with lower PSA), because some prostatic cancer can be indolent, a watch-and-wait approach is more appropriate
Advanced metastatic carcinoma is tx by androgen deprivation usually with GnRH analogs (these tend to produce clones that result in death and thus is not curative)
Describe the tissue of the ureter, bladder, ad urethra
They are lined with urothelium. Beneath the mucosa are the lamina propria and the muscularis propria

Urothelium is composed of: five to six layers of cells with oval nuclei, often with linear nuclear grooves, and a surface layer consisting of large, flattened “umbrella cells” with abundant cytoplasm.

What are some common things that can obstruct the ureters
- ureteropelvic junction obstruction can result in hydronephrosis (common in childhood)
- urothelial carcinomas
- retroperitoneal fibrosis (common in middle age)- associated with elevated IgG4 (below)




What most commonly causes bladder diverticuli?
These are blind pouchlike evaginations of bladder wall that can be congential but are more commonly the result of acquired lesions arising from persistent urethral obstruction (i.e. due to BPH). Some can lead to infection

What is Exstrophy of the bladder?
A developmental failure in the anterior wall of the abdomen and the bladder, so that the bladder either communicates directly through a large defect with the surface of the body or lies as an opened sac

What is Malakoplakia?
This most commonly occurs in the bladder and results from defects in phagocytic functions of macrophages, such that phagosomes become overloaded with undigested bacterial products as well as Michaelis-Gutmann bodies, which are laminated mineralized concretions resulting from deposition of calcium (below)

Epidemiology of bladder cancer
Bladder cancer accounts for approx. 3% of all cancer deaths. Almost 90% are urothelial carcinomas. These cancers are more common in men, in industralized countries, and in urban settings.
The vast majority of pts are between 50-80
What are some other types of bladder cancer?
squamous cell carcinoma and adenocarcinomas
What are the risk factors for bladder cancer?
- Not typically familial
- cigs, occupational carcinogens, and
Schistosoma haematobium infections where it is endemic (Egypt)

Two distinct precursor lesions to invasive urothelial carcinoma, namely:
noninvasive papillary tumor (most common)
carcinoma in situ
NOTE: In 50% of invasive bladder cancers, no precursor lesions is found
Noninvasive papillary urothelial neoplasms demonstrate a range of atypic and are graded to reflect therir biologic behavior. The most common grading system classifies tumors as follows:
1) papilloma
2) papillary urothelial neoplasm of low malignant potential (PUMLMP)
3) low grade papillary urothelial carcinoma
4) high grade papillary urothelial carcinoma

Remember that in CIS of the bladder, tumor cells lack co-adhesivenss, and thus tend to be shed into the urine where they can detected by cytology
CIS commonly is multifocal and without tx mostly progress to muscle-invasive cancer

Low grade papillary lesion

High grade papillary lesion

With invasive urothelial cancer, the extent of invasion and spread (staging) at the time of initial diagnosis is the most importnat prognostic factor
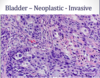


What is this?

A urethral caruncle- An inflammatory lesion that presents as a small, red, painful mass about the external urethral meatus, typically in older females.

It consists of inflamed granulation tissue covered by an intact but extremely friable mucosa, which may ulcerate and bleed with the slightest trauma.
How are urethral caruncles treated?
Surgical excision affords prompt relief and cure.


