Breast Pathology Pre-Study Flashcards
Most breast cancers arise where?
In the terminal duct lobular unit (TDLU) consisting of the terminal ducts, the lobules, and the surrounding stroma

What are the most common palpable lesions of the breast?
cysts, fibroadenomas, and invasive carcinomas
These are the histopathologic findings in a series of women seeking evaluation of breast ‘lumps’

Approximately 50% of carcinomas are located in what part of the breast?
the upper outer quadrant
NOTE: Only 10% of breast masses in women younger than age 40 are malignant as compared with 60% of masses in women older than age 50 (this number drops off around 80 yo)
the majority of cancers that have the capacity to metastasize will have done so by the time they reach a size that can be palpated—generally around 2 to 3 cm.
What are the major symptoms of breast disease (in order)?
lumpiness or palpable mass
pain
nipply discharge
What are the common common causes for nipple pain?
fibrocystic changes that are cyclic with the menstrual period or
due to obstruction or inflammation (especially in breastfeeding women)
NOTE: Only about 10% of breast cancers are painful
Bloody nipple discharge suggest what?
large duct papiloma
Why would it make sense to group fibrocystic breast changes into non-proliferative vs. proliferative changes?
Non-proliferative changes have a very small chance of transforming into cancer
What are fibrocystic changes?
These are the most common breast abnormality in pre-menopausal women and are most likely to be a consequence of the cyclic breast changes that occur normally during the menstrual cycle and result in either some form of fibrosis or cyst formation
Does estrogen therapy increase the risk of fibrocystic change? What about oral contraceptives?
No to either, and oral contraceptives may actually decrease the risk
Describe the morphology of non-proliferative fibrocytic changes in the breast

A single, large cyst may form within one breast, but changes are usually multifocal that appear as ill-defined, diffusely increased densities and nodules on mammography.
Unopened cysts are brown to blue in color (blue dome cysts) and are filled with fluid and secretions that may calcify to produce microcalcifications on mammaograms
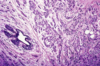
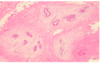
What is this showing?

There is a very pink epithelium characteristic of a nonproliferative cyst. Frequently, the lining cells are large and polygonal with eosinophilic cytoplasm, a process called apocrine metaplasia which is virtually always benign

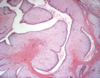
What is this showing?

Apocrine metaplasia, which is almost always benign
Normal ducts and lobules of the breast are lined by what?
two layers of cells- a layer of luminal cells overlying a second layer of myoepithelial cells
NOTE: In order to diagnose an invasive carcinoma, these layers must be destroyed.

What is a common sign of proliferative change?
epithelial hyperplasia, or the presence of more than two layers of cells lining to ducts and lobules of the breast (increas
What are the types of epithelial hyperplasia?
usual duct hyperplasia (below- note that slitlike fenestrations in the duct lumen) and atypical duct hyperplasia
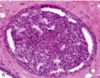
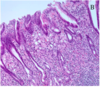
What is this showing?

Atypical ductal hyperplasia- is recognized by its histologic resemblance to ductal carcinoma in situ (DCIS). It consists of a relatively monomorphic proliferation of regularly spaced cells (with no overlap), sometimes with cribriform spaces.
Most surgeons will remove cells with atypical ductal hyperplasia
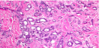
What is this?

Atypical lobular hyperplasia- consists of cells identical to those of lobular carcinoma in situ, but the cells do not fill or distend more than 50% of the acini within a lobule.
Surgeons typically do not surgically excise these cells
What is sclerosing adenosis (aka too many glands)?
A type of fibrocystic change that is less common than cysts and hyperplasia but is significant because it mimics carcinoma closely.
The involved terminal duct lobular unit is enlarged, and the acini are compressed and distorted by dense stroma.
Calcifications are present within some of the lumens.
Unlike carcinomas, the acini are arranged in a swirling pattern, and the outer border is well circumscribed.
The acini at the edge of a focus of sclerosing adenosis appear round and smoothly contoured. They possess a two-layered epithelium composed of both luminal and myoepithelial cells, and a basement membrane encloses each acinus.


The radiograph shows an irregular central mass with long radiodense projections.
Grossly the mass appears solid and has irregular borders, but it is not as firm as an invasive carcinoma.
The mass consists of a central nidus of small tubules entrapped in a densely fibrotic stroma and numerous projections containing epithelium with varying degrees of cyst formation and hyperplasia.
What types of fibrocystic changes have minimal or no increased risk of breast carcinoma?
fibrosis, cystic changes, apocrine metaplasia, and mild hyperplasia
What types of fibrocystic changes have slightly increased (1.5-2x) risk of breast carcinoma?
moderate to florid hyperplasia (without atypia), ductal papillomatosis, sclerosing adenosis
What types of fibrocystic changes have significantly increased risk of breast carcinoma?
atypical hyperplasia, whether ductal or lobular, DCIS, and LCIS
How do inflammatory processes of the breast typically present?
They are uncommon and are usually associated with pain and tenderness in the affected areas
What are some causes of inflammation in the breast?
Acute mastitis
Fat encrosis
Mammary duct ectasia
Lymphocytic mastitis
Granulomatous mastitis
What is the most common cause of acute mastitis?
It typically develops when bacteria, usually Staph aureus, gain access to breast tissue through the ducts, typically during breastfeeding and typically presents as single or mutiple abscesses. Usually found in the lateral breast

What causes fat necrosis in the breast?
It is an uncommon lesion that produces a mass, typically as the result of trauma that presents as a central focus of necrotic fat surrounded by neutrophils that later becomes enclosed by firous tissue and is eventually replaced by scar tissue or a cyst.
Calcifications may also develop in either the scar or cyst wall

What causes mammary duct ectasia?
a nonbacterial chronic inflammation associated with nipple obstruction most commonly. Ductal dilation and eventual rupture leads to reactive changes in the surrounding tissue that may present as a poorly defined periareolar mass with nipple retraction (mimics some cancer).
What are some known associations with lymphocytic mastitis?
Diabetes and possibly autoimmune
What are the common tumors of the breast?
¤Fibroadenoma (FA)
¤Phyllodes Tumor
¤Intraductal papilloma
¤Carcinoma
¤Gynecomastia
What are fibroadenomas?
The most common neoplasm of the female breast (especially common in women in their 30s), it is a biphasic tumor composed of fibroblastic stroma and epithelium-lined glands (but only the stromal cells are clonal are truly neoplastic)
Describe the gross appearance of fibroadenomas. How are they diagnosed?
They are usually discrete, firm, and mobile (feels rubbery and compressable) and on cut-section take on a uniform tan-white color, with softer yellow-pink specks representing the glandular areas.
Diagnosis is made by needle-core biopsy or excision

What causes fibroadenomas?
They are thought to be controlled by estrogen and characteristically can enlarge late in the menstrual cycle and during pregnancy and may regress and calcify after menopause
How do fibroadenomas appear histologically?
They are characterized by a loss fibroblastic stroma containing ductlike, epithelium-lined spaces

What are phyllodes tumors?
These are also biphasic, being composed of neoplastic cells and epithelium-lined glands. However, they can be distinguished from fibroadenomas because they are more cellular and form epithelium-lined leaflife projections
These arise de novo and are usually benign
Phyllodes tumors can be malignant. What are some indicators of a malignant prognosis?
increased stromal cellularity, rapid size increase, 10+ mitotic figures, and infiltrative margins.
NOTE: Even malignant tumors tend to remain localized (85%)
Be suspicious about a ‘fibroadenoma’ if it is large (> 35mm) and from an older woman (> 35 yrs)The surgeon may alert you to a history of recent growth

Benign Borderline Malignant
Pushing boundary Yes Usually Not usually
Stromal/epithelial balance Even Even Uneven
Stromal cellularity High High High
Variab. of stromal cellularity: Yes Yes Yes ++
Stromal mitoses /10 hpf < 5 5 - 10 >10
Phyloddes prognosis
What are Intraductal papillomas?
Benign neoplastic papillary growth most often seen in premenopausal women, and commonly found within the principal lactiferous ducts or sinuses.
How do intraductal papillomas tend to present?
- serous or blood nipple discharge
- the presence of a small subareolar tumor a few millimeters in diameter
- nipple retraction in rare cases