Lymphadenopathy Flashcards
Challenge to assessing lymph nodes in pedi primary care?
- Common! Challenge is avoiding invasive investigation while making timely diagnosis where necessary
- Younger kids constantly exposed to new antigens
- Young vs older kids: older children and ados have smaller LNs than younger kids
Lymphadenopathy:
Red Flags on History suspicious of malignancy
- Persistent node >6 weeks
- Firm, hard, immobile
- Node >2cm in size
- Rapidly increasing in size
- Family history of malignancy
- If hasn’t responded to antimicrobial therapy in 4 weeks
Lymphadenopathy:
Red Flags on History suspicious of TB
- Night sweats
- Recent travel to region endemic for TB
- Weight loss
Lymphadenopathy:
Red Flags on History suspicious of HIV/hepatitis
- Exposure to HIV or hepatitis
- Nontender nodes in axillary, cervical, and occipital region
- IV drug use or risky sexual behavor
Lymphadenopathy - red flags on exam
- •Hard, rubbery, matted nodes
- •Nodes > 2 cm
- •swelling of node
Necessary components of history taking in the setting of pediatric lymphadenopathy
•S/S of infection and/or systemic disease, exposures to sick contacts or animals/pests, IZ status, medications, travel, high-risk behavior, immune status
Necessary components of PE in the setting of pediatric lymphadenopathy
Depends on area and other symptoms, but always:
- •Location, size, consistency, fixation, tenderness
- •NL: asymmetric, small & discrete (non-matted), soft, mobile, NT
Generalized vs local LAD
generalized is 2+ noncontiguous regions
Evaluation of lymph nodes - possible labs / imaging based on symptoms
- •Labs:
- •CBC, ESR & CRP, lactate dehydrogenase and uric acid, liver enzymes, serology (EBV, HIV, CMV, parvovirus, bartonella, etc), cultures, PPD/Quant Gold, specific atypical mycobacterial Ag
- •Imaging:
- •Radiography (CXR, neck XR), U/S, CT
Excisional/open biopsy vs FNA
- Excisional biopsy
- BEST - preserves Intact specimen, Confirms malignancy, granulomatous tissues of TB or sarcoid
- •Cons: invasive, should be done in a medical center specializing in care of children – removal of wrong node leading to false neg is not uncommon
- Fine needle aspiration
- •Decompress suppurative LN, obtain tissue specimen for histopathology
- •Cons: Invasive, sedation/general anesthesia, éfalse negative rate, potential for sinus tract formation (wound tunneling).
- Not typically recommended.
Reasons for Early biopsy
EARLY if high suspicion for malignancy
- Systemic sx: fever >1 week, night sweats, wt loss >10% body weight
- Lack of infectious Sx in ENT
- Size >2cm, increasing over 2 weeks, no decrease after 4 weeks or no response to 2 weeks of antimicrobial therapy
- Supraclavicular & lower cervical
- Hard, matted, rubbery
- Abnl CXR or CBC
Cervical LNs + Drainage

Congenital vs acquired cmv
cogenital must be Dxed in first 3 weeks of life
S/S of Congenital CMV
- •Most are asymptomatic
- Common:
- •Sensorineural hearing loss*
- •Lethargy*
- •Hypotonia*
- •Petechiae*
- •Jaundice at birth*
- •Hepatosplenomegaly*
- •Small size for gestational age*
- •Microcephaly*
- Other:
- •Polymicrogyria
- •Chorioretinitis
- •Seizures
- •Hemolytic anemia
- •Pneumonia
Diagnostics and Lab findings in congenital CMV
- Diagnosis: CMV detected on viral culture (urine or saliva)
- other options: rapid culture, PCR
- Associated findings
- •Elevated liver transaminases
- •Thrombocytopenia
- •Elevated direct and indirect serum bilirubin
Treatment for CMV
- Asymptomatic infants do not require antiviral treatment
- IV Ganciclovir or PO valganciclovir for symptomatic infections
Clinical manifestations of acquired CMV
- •Most children are asymptomatic
- Common:
- •Fever*
- •Fatigue*
- •Pharyngitis*
- •Mononucleosis-like syndrome*
- •Adenopathy*
- •Hepatitis*
- Other:
- •Headache
- •Abdominal pain
- •Diarrhea
- •Arthralgias
- •Rash
Diagnosis of acquired cmv + associated lab findings
- Diagnostic labs
- •CMV IgG seroconversion with CMV IgM antibody
- Associated findings
- •Lymphocytosis or lymphopenia
- •Thrombocytopenia
- •Abnormal liver function tests
- •Negative monospot test
Treatment of acquired cmv
- •Antiviral treatment is generally not indicated.
- •Supportive care with hydration and fever control
staph aureus or strep pneumonia on culture in setting of acute pharyngitis
may show up on culture but do not cause acute pharyngitis
Common causes of infectious pharyngitis
- Streptococci
- Group A strep
- Respiratory viruses
- Adenovirus, coxsackie, influenza, parainfluenza
- Infectious mononucleosis
- EBV
Diagnosis of infectious pharyngitis
- Clinical manifestations
- Symptoms with pharyngeal erythema, exudate: rapid strep test
- If negative: throat culture
- Back up culture for rapid antigen diagnostic test
Treatment for infectious pharyngitis
- •Bacterial – antibiotics, analgesics, topical therapies
- •Viral – analgesics, topical therapies
What is lymphadenitis?
- enlarged, inflamed, erythematous and tender lymph nodes - infection / inflammation in LNs themselves rather than a marker of infectious elsewhere
- •Usually unilateral
- •2-6cm in size
Common age for lymphadenitis
1-5yo
Most common bacterial pathogens in lympadenitis
staph aureus, strep pyogenes
Diagnostic labs in lymphadenitis
not typically necessary - can use clinical manifestations
Treatment of lymphadenitis: mild / moderate / severe
- Mild: observe 48-72h, warm compresses, tylenol prn
-
Moderate: PO antibiotics, f/u w/in 48-72h
- (possible but unlikely cultures - blood, throat, biopsy)
- Severe: I&D, blood cultures, antibiotics
- Antibiotics: Augmentin or keflex
- •Further workup needed if not regressing after 2 weeks on abx
Nodes concerning for malignancy
Any supraclavicular, infraclavicular, epitrochlear
Abnormal node size
- >1cm w/following exceptions:
- Epitrochlear > 0.5 cm
- Inguinal >1.5 cm
- Cervical >2 cm
Work up for suspected malignancy
- •CBC with differential
- •CXR
- •Referral for lymph node biopsy
- Subsequent referral to specialist (hematology/oncology or ENT)
Considerations in performing biopsy (which you’ll be referring out for, but.)
- outpatient setting under local anesthesia - place that specializes in pedi care
- •The most abnormal node is selected if multiple node groups are involved
- •If no single node predominates, the preference goes as such: supraclavicular > neck > axilla > groin (supraclavicular being most specific for malignancy and inguinal being least). Infection risk is also high in groin and axilla.
- •Open biopsy is preferred to FNA because of false negative rate with FNA> FNA is preferred in searching for cancer recurrence.
Inguinal lymph nodes: considerations in age and size
- Nl
- More common in >2yo, less common
- Usually no specific etiology unless >3cm
Causes of inguinal lymphadenopathy
•Common: UTI, LE suppurative infection, genital herpes, syphilis, gonococcal infection, lymphoma
•Less common: Yersinia pestis, chancroid, lymphogranuloma venereum
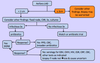
MGMT algorithm for localized LAD

Axillary LNs
- Humeral (lateral), Central, apical, subscapular (posterior), pectoral (anterior)
- Drains: arm, breast, thorax, neck
- Nl
causes of axillary LAD
- Common:* cat scratch (B. henselae), pyogenic infections of upper arm, brucellosis, reactive response to disruption in skin integrity
- Less common:* Brucellosis, Yersinia pestis, rat-bite fever, toxoplasmosis, rheumatologic disease of hand or wrist
MGMT algorithm for localized axillary LAD
Cat scratch disease / Bartonella henselae
cause and seasonal distribution
•Cause: cat scratch, cat bite, flea bite. Most associated w/kittens w/fleas
•Seasonal distribution: peaks fall & early winter

Clinical manifestations of cat scratch disease
•Common presentation:
•skin lesion: 3-10 days after inoculation
•Lymphadenopathy:
- hallmark of CSD. ~2 weeks after inoculation. 1-5cm
- Common sites: axillary, epitrochlear, cervical, supraclavicular, submandibular
- Usually tender, erythematous overlying skin, occasionally suppurative
- Usually resolves in 1-4 months (up to 3 years)
- Hepatomegaly or splenomegaly.
- FUO
•Uncommon presentations:
•Ocular manifestations, Neurological involvement, musculoskeletal involvement

Diagnosis of CSD
- clinical manifestations + probable exposure to cats/fleas.
- Positive serology for B. henselae supports Dx
- Atypical findings:
- Positive serology
- ?tissue biopsy for histopathologic changes, pcr, & culture. Culture is definitive, but difficult to isolate. and invasive!
MGMT of typical CSD
- Usually resolves on its own
- But - recommend antibiotic therapy: 5-day course Azithromycin.
- >45.5kg: 500mg day 1, then 250mg x 4 days
•Ocular, Neurological, musculoskeletal involvement: consider referral
Generalized LAD: definition and general approach
- •Enlarged (>1cm) nodes in two or more noncontiguous regions
- •Most often self-limited and does not require laboratory diagnosis
Generalized LAD
general causes
- •MIAMI
- •Malignancy
- •Infection
- •Autoimmune
- •Miscelanious
- •Iatrogenic
medications associated w/LAD
Phenytoin, phenobarbital, carbamazepine, isoniazid, aspirin, barbiturates, penicillin, tetracycline, iodides, sulfonamides, allopurinol, and phenylbutazone
Presentation of HIV in terms of LAD
- may be a mononucleosis type of syndrome with many nonspecific symptoms
- generalized LAD, persists longer than 3 months
- possible IV drug use, sexual history and protection
- Early HIV infection may be asymptomatic
- •Or may present with minor c/o fever, lymphadenopathy, sore throat, rash, myalgia, arthalgia, GI distress, fatigue, fungal infections, seborrhoeic dermatitis, neurological issues like strange behavior or memory loss
Mono / EBV: S/S
- •Caused by Epstein Barr Virus (EBV) spread by saliva
- •Mono Triad: fever, pharyngitis, lymphadenopathy
- •S/s:
- •Prolonged fever, fatigue/malaise, Pharyngitis – usually exudative but not always, Palatal petechiae, URI, Painless generalized lymphadenopathy, Possible splenomegaly
•Illness lasts 3-4 weeks, fatigue for further 6-12 months
Important history questions with mono / EBV
- Trouble breathing or swallowing? – ABCs and hydration status
- Headaches, weakness, confusion – possible CNS complications
Diagnostic tests for EBV/mono
•Nonspecific serologic test for heterophil antibody aka monospot test for EBV
•Gold standard
- Often negative in children under 4 yo but identifies 85% of cases in older children and adolescents
- First 7 days of illness, test may be negative. Re-test in 1-2 weeks
- Possible
CBC with differential
- To determine increased WBCs (infection) and to discover any other complications such as pernicious anemia
- Blood smear
- Atypical lymphocytes is diagnostic of acute infection and r/o toxoplasmosis and hepatitis
- Rapid Strep test to r/o strep, LFT to r/o hepatitis if exposed, HIV test if risk
Treatment for EBV/mono
- •Bed rest, possible to give corticosteroids if tonsils severely enlarged, no contact sports due to risk of splenic rupture
- •F/u every 1-2 weeks until s/s completely resolve
- Can return to contact sports when feeling 100% better and no sign of spleen enlargement
algorithm for generalized LAD

Suggested approach to unexplained localized (non-supraclavicular) LAD

- At your clinic you see a two day-old infant with sensorineural hearing loss. You immediately think of symptomatic congenital CMV as a differential diagnosis. If this were the case, what else might you expect to see?
a. Large for gestational age, hypoglycemia
b. Hepatosplenomegaly, jaundice
c. Hypertonia, lymphadenopathy in single node
d. Drooling, listless pulses
B
- An 18 year old female presents with fatigue, fever, sore throat, and lymphadenopathy x4 days. Her CBC reveals atypical lymphocytosis, but her Monospot test is negative. Which of the following statements is TRUE?
a. The Monospot test is not a highly sensitive test for this age range.
b. Her symptoms may be due to primary infection by cytomegalovirus (CMV).
c. There is no role for EBV-specific antibodies in making the diagnosis.
d. A corticosteroid could be prescribed to reduce the size of the lymph nodes.
B


