Lower Respiratory Tract Infections in Children Flashcards
LRTI is infection distal to the _______
larynx
Principles of management:
- Make a diagnosis (____)
- Assess the patient (____) - Oxygenation, hydration, nutrition
- To treat or not to treat (____)
easy
easy
grey - Biggest dilemma is to weather to treat or not
Putting LRTI into context - how common are they?
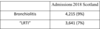
More than a third of all admissions of all hospitals, of all children to all hospitals in Scotland in 2018 were explained by upper and lower respiratory tract infection
what is Tracheitis?
- Uncommon
- “croup which does not get better”
- Fever, sick child
- Staph or Strep invasive infection
- Augmentin

what is Bronchitis and what are the symptoms?
- Common ++++
- Endobronchial infection
- Loose rattly cough with URTI
- Post-tussive vomit - “glut” (sputum)
- Chest free of wheeze/creps
- Haemophilus/Pneumococcus
- Mostly self-limiting
- Child VERY well, parent worried
what is the mechanism of Bacterial bronchitis?
•Disturbed mucociliary clearance
- Minor airway malacia
- RSV/adenovirus
- Lack of social inhibition!
- Bacterial infection/overgrowth is secondary
Virus switches of mucociliary clearance
Bronchitis:
So what happens in winter is……
Common for child to have 4 or 5 cycles of this in winter

how long may a cough last?

what is the natural history of Bacterial bronchitis?
- Following URTI
- Lasts 4 weeks
- 60-80% respond (antibiotics)
- First winter bad
- Second winter better
- Third winter fine
- Pneumococcus/H flu

Persistent bacterial bronchitis: what is the management?
- Make the diagnosis
- Reassure
- Do not treat
Bronchiolitis – a clinical diagnosis
what is it?
(Different form bronchitis (infection of large airways). As this is infection of small airways)
- LRTI of infants
- Affects 30-40% of all infants
- Usually RSV, others include paraflu III, HMPV
- Nasal stuffiness, tachypnoea, poor feeding
- Crackles +/- wheeze
Not many conditions that are as predictable as bronchiolitis - what does the progression of it look like?
If you see them at day 3 and they are bad then admit to hospital as you know they will get worse but if you see them at day 5 and their oxygenation and hydration are fine then you know tomorrow they wont be any worse

what is the duration of bronchiolitis?

when about does bronchitis occur?
Comes at Christmas

Bronchiolitis:
- <12 months old
- One off (___ recurrent)
- Typical _______….
12 (Condition of infancy)
NOT
history
what is the Management of bronchiolitis?
- Maximal observation
- Minimal intervention
what investigation can be done for bronchiolitis?
a clinical diagnosis
- NPA (nursing in same ward) (identify what the virus is)
- Oxygen saturations (severity)
- No routine need for - CXR, Bloods, Bacterial cultures
what Medications proven to work in bronchiolitis?
none
Lower respiratory tract infection - what are the typical features?
- 48 hrs (history of), fever (>38.5oC), SOB, cough, grunting
- Wheeze makes bacterial cause unlikely
- Reduced or bronchial breath sounds
- “Infective agents” - Virus+commensal bacteria/bacterium
if a patient presents, Is it pneumonia or not?
- Totally academic! (does the child care??)
- Word causes great anxiety
- You might call it pneumonia if:
- Signs are focal, ie in one area (LLZ – left lower zone)
- Creps
- High fever
•Otherwise call it LRTI (or chest infection)
should you x-ray in pneumonia?
Regardless of these x-rays, the management is exactly the same
This is the chest X-ray of a child with a 48 hour history of fever, cough, shortness of breath, and is treated with amoxicillin
BTS guidelines – community acquired pneumonia
what are the guidlines?
- Investigations - CXR and inflammatory makers (e.g. CRP, BC) NOT “routine”
- Management:
- Nothing if symptoms are mild (oxygen and hydration normal)
- (always offer to review if things get worse!)
- Oral Amoxycillin first line
- Oral Macrolide second choice (if allergic to amoxycillin)
- Only for iv if vomiting
iv versus oral antibiotics:
When:
- antibiotics are indicated (48 hours, etc, etc)
- in non-severe LRTI
- when child is not vomiting
If child fills 3 criteria, then they get away with oral antibiotics - why is oral better than IV?
Oral antibiotics “win” 2:1
√ Shorter hospital stay
√ Cheaper
X Fever for a few more hours
What is the difference between LRTI and bronchiolitis?
Both technically the same thing
bronchiolitis has a 12 month age limit




