Lecture 9: Drugs Used for Heart Failure Flashcards
Left-sided systolic heart failure is due to failure of what?
Failure of the pump function of the heart (EF <45%) due to dysf. or destruction of cardiac myocytes or their molecular components

Left-sided diastolic heart failure occurs due to what?
Ventricular capacitance is diminished and/or when ventricle becomes “stiff” and cannot fully relax during diastole

What are 2 common causes of left-sided diastolic heart failure?
- Ventricular hypertrophy due to chronic HTN
- CT disease such as amyloidosis
What occurs to both afterload and preload in systolic heart failure?
- Increased afterload
- Increased preload

What is the LVEF like in systolic HF and there is usually progressive what?
- LVEF <50% = HFrEF
- Usually progressive chamber dilation w/ eccentric remodeling
Diastolic heart failure is now especially common in whom?
Elderly women
What occurs to the ejection fraction in diastolic heart failure?
Usually normal = HFpEF
What occurs to preload in diastolic heart failure?
Decreased preload

Diastolic heart failure has a poor tolerance of what 2 things and is worsened by an increase in what?
- DHF –> poor tolerance of atrial fibrillation
- DHF –> poor tolerance of tachycardia
- DHF is worsened by ↑ MAP
Worsening of diastolic HF by ischemia raises left atrial pressure which can lead to which life threatening condition?
“Flash” pulmonary edema
With a drop in cardiac output, what are the adpative mechanisms (i.e., what gets increased) contributing to HF?
- ↑ renin + ↑ aldosterone + ↑ natriuretic peptides
- ↑ sympathetic discharge
- ↑ preload and afterload
- ↑ remodeling of heart

ACE-I and ARB’s lead to less angiotensin II which has what 3 positive effects in pt’s with HF?
- Less vasoconstriction (↓ afterload)
- Less aldosterone and less Na+/H2O retention (↓ preload)
- ↓ cell proliferation and remodeling
Define the terms inotropic agent and chronotropic agent.
- Ionotropic agents alter the force/strength of muscle contractions
- Chronotropic agents may change the heart rate and rhythm
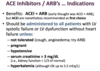
ACE-I (-prils) are used clinically for what heart conditions?
- Heart failure w/ reduced EF (HFrEF) = systolic HF
- LV dysfunction following MI
What are 2 major AE’s associated with ACE-I’s?
- Cough
- Angioedema
Which 2 ACE-I are now widely used due their longer half-life permitting 1x/day dosing?
- Benazepril
- Lisonopril
Which drugs can be used for HF if patient is intolerant to ACE-I’s?
ARBs (-sartans)
Which ARB is noteworthy in that it is not a prodrug requiring activation?
Valsartan
Which ARB is noteworthy in that it displays relatively irreversible binding?
Candesartan
What is the MOA of sacubitril and what is it co-crystalized with as a combo drug for HF?
- Prodrug that inhibits neprilysin (neutral endopeptidase [NEP])
- Co-crystalized with the ARB, Valsartan
- Valsartan/sacubitril
What does the neutral endopeptidase blockade by sacubitril lead to?
Increased levels of natriuretic peptides

What are3 common AE’s of valsartan/sacubitril?
- HYPOtension
- HYPERkalemia
- ↑ serum creatinine
What is the effect of ↑ ANP on GFR, renin/aldosterone secretion, Na+/H2O reabsorption, and ADH secretion?
- ↑ GFR
- ↓ renin + ↓ aldosterone secretion
- ↓ Na+/H2O reabsorption
- ↓ ADH secretion and ADH effects in collecting duct

ACE-I’s/ARBs should be administered to all pt’s with LV systolic failure or LV dysfunction w/o HF except in what 5 situations?
- Not tolerated (cough, angioedema; try ARB)
- Pregnant
- HYPOtensive
- Serum creatinine >3 mg/dL
- HYPERkalemia
Which beta-blocker has been shown to work best in HF?
Carvedilol
Which other beta-blocker is a non-selective alpha/beta blocker, used primarily for severe HTN and tx of hypertensive emergencies?
Labetalol
What condition should patient be in for use of carvedilol in HF and what are it’s recommended uses?
- IF clinically stable
- Recent or remote hx of MI or ACS and ↓ EF (rEF; <40%)
- rEF to prevent SYMPTOMATIC HF (even if no hx of MI)
Carvedilol is used to prevent what in the heart as a result of excessive sympathetic stimulation during HF?
Prevent down-regulation of the β1-receptors
List 5 benefits of carvedilol in HF by preventing the down-regulation of β1-receptors?
- Keeps heart responsive to sympathetic drive
- Protects against dysrhythmias
- ↓ renin secretion
- ↓ myocardial O2 consumption
- Limits heart muscle remodeling
Carvedilol should only be administered to which patients?
Clinically stable
Which type of HF’s is carvedilol useful in and should be given along with ACE-I to which pt’s?
- Pts with diastolic HF will benefit from a lower HR
- Should be given to all pt’s w/ symptomatic CHF and LVEF <40% unless contraindications exist
- Given along w/ ACE-I to all pt’s w/ LV systolic dysfunction caused by MI to reduce mortality

What is the MOA of ivabradine and effects on heart?
- Selective and specific inhibition of the HCN channels (f-channels) within SA node
- Disrupts If (“funny” current) to prolong diastole and slow HR
What is the clinical application of ivabradine; specifically in which pt’s?
- Tx of resting HR ≥70 bpm in pt’s w/ stable, symptomatic chronic HF w/ LVEF ≤35% who are in sinus rhythm with:
- Maximally tolerated doses of β-blockers
OR
- Contraindications to β-blocker use
What is the MOA of spironolactone and its effects on ion and volume levels?
- Competitive antagonist of aldosterone receptors
- K+-sparing diuretic due to ↓ ability of aldosterone to promote Na+-K+ exchange in collecting ducts
- ↓ plasma Na+ and volume
Which K+-sparing diuretic is a more selective aldosterone antagonist, approved for use in post-MI heart failure or in combo for tx of HTN?
Eplerenone
What are the pharmacokinetics of spironolactone like and why is a single dose effective for 2-3 days?
Steroid effects are slow on and slow off
What are some possible AE’s associated with Spironolactone?
- HYPERkalemia (duh.)
- Amenorrhea, hirsutism, gynecomastia, and impotence
- Tumorigen in chronic animal toxicity studies (boxed warning)
What are 3 beneficial effects of spironolactone on the heart?
- ↓ myocardial fibrosis
- Reduces early morning rise in HR
- Reduces mortality and morbidity in pt’s with severe HF
Explain the purpose of aldosterone inhibition when treating post-myocardial infarction heart failure?
- Damaged heart vasculature synthesizes aldosterone after MI
- Locally produced aldosterone contributes to cardiac fibrosis