Lecture 12: Treatments for Diarrhea, Abdominal Pain, and Constipation Flashcards
What are the 3 Opioid Agonists used to treat diarrhea?
- Loperamide
- Diphenoxylate
- Eluxadoline
What is the MOA of Loperamide as an Anti-diarrheal?
- Interferes w/ peristalsis (slows transit time)
- Direct action on circular and longitudinal ms. of intestinal wall
What is one of the serious side-effects related to Loperamide?
Cardiac toxicities leading to death
Which anti-diarrheal agent is given with a small amount of atropine to discourage abuse/OD’s?
Diphenoxylate (opioid agonist)

MOA of Diphenoxylate?
- Exerts effects locally and centrally on GI smooth muscle cells
- Inhibits GI motility
- Slow excess GI propulsion
What is the MOA of the anti-diarrheal Eluxadoline?
- Agonist at opioid mu and kappareceptors inGI tract –> slows peristalsis/delays digestion
- Antagonist at delta opioid receptors in GI –> ↓ stomach, pancreas and biliary secretion
Eluxadoline (opioid agonist) is indicated for use in which patients?
IBS-D (diarrhea predominant subtype)
What is the the most serious adverse effect associated with Eluxadoline?
Which patients are most at risk?
- Hepatic/pancreatic toxicity
- Pancreatitis = high-risk in pts w/o GB –> DEATHs have occurred

The anti-diarrheal, Eluxadoline, is contraindicated in which 5 conditions?
1) Biliary duct obstruction
2) Sphincter of Oddi dysfunction
3) Alcoholism
4) Hx of Pancreatitis
5) Severe hepatic impairment
Therapy with the anti-diarrheal, Eluxadoline, should be stopped if what develops?
Severe constipation develops and lasts 4+ days
What is the 5-HT3 antagonist used as an anti-diarrheal?
Alosetron
What is the only indication for using the antidiarrheal, Alosetron?
Chronic, severe IBS-D that is NOT responsive to other conventional therapies
What is a major adverse effect related to the anti-diarrheal, Alosetron?
If which side effect develops should therapy be stopped?
- Ischemic colitis (black box warning!)
- Constipation is an adverse effect and if this occurs, STOP THERAPY!
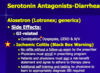
What are the regulations for prescribing the anti-diarrheal, Alosetron due to one of its severe adverse effects?
i.e., what must both the doc and pt do
- No refills w/o a follow up exam!
- Doc must enroll in prescribing program
- Doc and pt must sign a risk-benefit statement and agree to adhere to therapy plans
- Additional self-training and testing by Docs to learn to appropriately Dx IBS required!
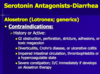
What are the contraindications for the anti-diarrheal, Alestron?
Hx of Active:
- GI obstruction, perforation, stricture, adhesion or toxic megacolon
- Diverticulitis, Chron Dz, or UC
- Impaired intestinal circulation, thrombophlebitis or a hypercoagulable state
What is the Cl- Channel Inhibitor used as an Anti-diarrheal?
Crofelemer
What is the MOA of the anti-diarrheal, Crofelemer?
- Inhibits Cl- secretion by blocking:
- cAMP-stimulated CFTR channels and
- Calcium-activated (CaCC) chloride channels
What is the specific indication for using the anti-diarrheal, Crofelemer?
Non-infectious diarrhea in HIV/AIDS pts. on anti-retroviral tx
Which drug class is used for abdominal pain/spasms associated with IBS?
Anti-muscarinics
What are the 4 antimuscarinics used for abdominal pain/spasms associated w/ IBS?
- Hyoscyamine
- Dicyclomine
- Clindinium/Chlordiazepoxide
What is the guanylate cyclase-c agonist used for constipation and it’s two MOA?
- Linaclotide
- Binds GC-C on luminal surface of intestinal epithelium and increases intra/extracellular [cGMP]
- Stimulates secretion of Cl-/HCO3- into intestinal lumen via activation of CFTR ion channels
What are the indication for use of the anti-constipation agent, Linaclotide?
- Constipation predominant IBS (IBS-C)
- Chronic idiopathic constipation (CIC)
What is the Selective Chloride (C2) Channel Activator used for treatment of constipation?
Lubiprostone
*“Lubi“-prostone –> “Lubes up the GI”
What is the MOA for the anti-constipation drug, Lubiprostone?
- A bicyclic FA, PGE-1 derivative
- Increases intestinal fluid secretion by activating GI specific chloride channels (CIC-2) in luminal cells of intestinal epithelium






