Lecture 10.1: Myelodysplasias and Myeloproliferative Syndromes Flashcards
Myelodysplastic syndromes are associated with what enviornmental exposures?
Radiation and benzene

What are the most common offenders associated with therapy-realted Myelodysplastic syndromes?
- Alkylating agents: cyclophosphamide, ifosfamide, cisplatin, busulfan, nitrosourea, or procarbazine
- Anthracycline antibiotics: adriamycin, daunorubicin, epirubicin

Some myelodysplastic syndromes in adults have which recognizable germline mutation?
germline GATA2, RUNX1 or telomere repair gene mutations
Myelodysplastic syndromes are disorders of which cells and are characterized by what?
- Disorders of the pluripotent stem cell
- Characterized by ineffective hematopoiesis –> pancytopenia w/ HYPERplastic marrow

Describe the major cytogenetic abnormalities associated with myelodysplastic syndromes?
- Partial or total loss of long arm of chromosomes 5 or 7 and 20
- Inversion of chromosome 16
- Trisomy 8

Which gene mutation is strongly associatd with sideroblastic anemia?
Mutations in genes of RNA splicing machinery, especially SF3B1
What is the clinical presentation like for myelodysplastic syndromes?
- Half are asymptomatic
- Sx’s may include: fatigue, pallor, bleeding and infection due to pancytopenia

What are 2 lab abnormalities which may be seen in association with myelodysplastic syndromes?
- Elevated serum LDH
- Evidence (in some) of iron overload: ↑ ferritin w/ serum iron and TIBC often normal

What are 3 differential diagnoses that should be offered up in any patient with pancytopenia?
- Hypersplenism
- Aplastic anemia
- Myelodysplasia

Which myelodysplastic syndrome is associated with the lowest risk of conversion to AML (10-15%)?
Refractory anemia with ringed sideroblasts (RARS)

What test and potential therapy should be done on any patient with anemia and ringed sideroblasts present?
- Check B6 level (pyridoxine)
- Replace B6 for at least 6 months if deficientm then repeat marrow - if no improvement, pt. has pyridoxine resistant sideroblastic anemia (RARS)

What are 5 adverse prognostic features associated with Myelodysplatic Syndromes (blasts, platelets, Hgb, neutrophils, and age)?
- Marrow blasts >5%
- Platelets <100,000/uL
- Hemoglobin <10 g/dL
- Neutrophils <2500/uL
- Age >60 years

List 3 cytogenetic related abnormalities associated with poor prognosis in myelodysplastic syndromes?
- Monosomy 7
- HYPOdiploidy
- Multiple abnormalities

Myelodysplastic syndromes associated with what cytogenetic abnormality is associated with a favorable prognosis?
5q- syndrome; which leads to heterozygous loss of a ribosomal protein gene (ribosomal protein gene mutations cause Diamond-Blackfin anemia)
What is considered supportive care for myelodysplastic syndromes, when are PRBCs and platelets given?
- Avoid meds that damage marrow
- Aggressive tx of infections w/ Abx
- Transfuse PRBCs when symptomatic
- Transfuse platelets ONLY for bleeding or in prep for surgery
- Watch for iron-overload; give desferrioxamine or deferasirox if present
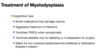
What is the benefit of giving EPO to pt with myelodysplastic syndromes and what level of EPO predicts poor prognosis?
- May decrease or ameliorate transfusion requirement in some; but is expensive
- Serum EPO level >500 predicts poor response

Which chemotherapy drug is given for 5q- syndrome (MDS) only; what is its main MOA, and what are toxicities associated with it?
- Lenalidomide, an angiogenesis inhibitor; particularly effective in reversing anemia
- Toxicities = myelosuppression + ↑ risk of DVT’s and PE’s

Which 2 chemotherapeutic agents are frequently used in high-risk MDS patients who are not candidates for stem cell transplant, and may also be effective in lower risk patients?
Hypomethylating agents –> Decitabine and Azacitidine

What is the MOA of Azacitidine and Decitabine used in some pt’s with MDS; what are the major AE’s?
- Cause hypomethylation (demethylation) of DNA and direct cytotoxicity on abnormal bone marrow hematopoietic cells
- Major toxicity = myelosuppression, leading to worsening blood counts

What is the only treatment which offers a cure for MDS and whom should it be considered for?
- Hematopoietic stem cell transplantation
- Should be considered for pt’s with MDS who are <60 and have an HLA-matching sibling donor

ATG, cyclosporine, and the anti-CD52 monoclonal antibody alemtuzumab are especially effective in which pt’s with MDS?
Younger pt’s (<60) with more favorable IPSS scores and who bear HLA-DR15
What are common presenting signs/sx’s of Primary Myelofibrosis?
- Anemia
- May have fever + night sweats + anorexia and weight loss
- Splenomegaly may be massive (due to ↑ extramedulary hematopoiesis)
What is the triad of Myelofibrosis?
- Leukoerythroblastic anemia
- Pokilocytosis = varying shapes i.e., tear-drop cells
- Splenomegaly

How is the diagnosis of primary myelofibrosis made and what is seen?
- Bone marrow biopsy
- Shows ↑ collagen and reticulin fibrosis + ↑ numbers dysplastic-appearing megakaryocytes + osteosclerosis

What are 2 conditions that cause 2’ bone marrow fibrosis which need to be excluded before making dx of primary myelofibrosis?
Miliary tuberculosis and metastatic cancer
What are 3 driver mutations which may be present and assist in the dx of primary myelofibrosis; which may have better prognosis?
- JAK2 V617F mutations in about 50% of cases
- Calreticulin (CALR) mutations: may have better prognosis
- MPL mutations

What are the leukocyte and platelet counts seen with Primary Myelofibrosis?
Normal or increased
What are some of the complications which may arise with exuberant extramedullary hematopoiesis seen in Primary Myelofibrosis?
- Portal, pulmonary, or intracranial HTN
- Intestinal or ureteral obstruction
- Pericardial tamponade
- Spinal cord compression
- Skin nodules
- Massive splenomegaly —> splenic infarction
How should the anemia be managed in patient with primary myelofibrosis?
- Manage with transfusion
- EPO administration if serum EPO <500
- Transfuse platelets ONLY if bleed occurs

What is the most common cause of death in pt’s with Myelofibrosis and how does this impact your treatment plan?
Overwhelming infection, so treat infections aggressively
How should asymptomatic pt with primary myelofibrosis be managed?
Observation
What are the tx options for the splenomegaly seen with primary myelofibrosis; what are the risks?
- Hydroxyurea is variably effective - may be overly myelosuppressive
- Splenic irradiation-but assoc. w/ significant risk ofneutropenia, infection, and operative hemorrhage if splenectomy is attempted
- Splenectomy in severe cases but is dangerous

Which drug has proved effective in reducing the splenomegaly and alleviating constitutional sx’s in cases of intermediate and high-risk myelofibrosis?
JAK2 inhibitor, Ruxolitinib

What is the only curative treatment for myelofibrosis and who is it reserved for?
Allogenic BM transplantation; used in younger pt’s and older pt’s with high-risk disease

What are some of the common and unique presenting sx’s of Polycythemia Vera?
- Facial rubor = red facies
- Pruritus with a hot shower or bath
- HA + dizziness + blurred vision
- Heaviness in the arms or legs
- Erythromelalgia

What are the laboratory findings indicative of polycythemia vera?
- Increased RBC numbers (Hgb/Hct): may seen nucleated RBCs on smear
- ↑ leukocyte alkaline phosphatase (LAP)
- ↑ WBC and/or platelet counts

Virtually all cases of polycythemia vera are associated with what mutation?JAK
JAK2 mutation

What are some of the complications which may arise with polycythemia vera?
- Increased risk of thromboembolic and hemorrhagic disorder, including stroke and MI
- Associated with Budd-Chiari Syndrome

What are some of the secondary causes of elevated RBC counts which need to be excluded before making dx of polycythemia vera?
- Hemoconcentration due to dehydration; check BUN/Cr levels
- Pulmonary disease: COPD (smokers polycythemia)
- EPO producing tumors (RCC and neuroendocrine tumors)
- Hemoglobinopathy w/ high affinity Hgb
- Living at high altitudes: hypoxia from decreased FiO2

What should to work-up for suspected polycythemia vera include?
- Full hx and physical exam
- Routine CBC and biochemical profile
- Exclusion of hemoconcentration: is pt dehydrated? BUN/Cr normal?
- Check serum EPO level: should be decreased or normal in PCV
- U/S of kidneys optional; but should be done if RCC suspected
- Exclude abnormal lung function: pulse oximetry w/ ABG
- PFT w/ DLCO: tests lung function and performance

What is the mainstay of treatment for polycythemia vera?
- Phlebotomy of 250-500cc whole blood every 1-2 weeks as long as Hct >50%
- Schedule phlebotomy chronically for pt’s as needed (usually every 6-12 weeks)

Pt’s with polycythemia vera who are >60 y/o or who have had prior thromboembolic events remain at high risk for mobiditiy despite phlebotomy and should receive what treatment?
Hydroxyurea



