L15: Physio Management Flashcards
What are 4 roles of manual examination?
- Ensures a thorough examination
- From the patient’s perspective
- Helps ascertain if it is mechanical LBP (versus CS, non-mechanical pain)
- Allows assessment of relative segmental mobility (eg. PAIVMs)
- Indicates reactive/nociceptive level for diagnosis
- Can confirm the diagnosis (eg. pain coming from L2-3 segment)
- If manual therapy is used – allows assessment prior to manual therapy
What is the manual therapy effects of the mechanical mechanism?
Transient biomechanical changes in position and posture, but no lasting change.
No treatment technique is specific to a single structure, only biased

What is the manual therapy effect of the spinal mechanisms?
Neuromuscular response which leads to altered neurone activity, afferent discharge and muscle activity
Eg. descending inhibition

What are the 4 manual therapy effect of the supraspinal mechanism?
- Endogenous opioid
- Sympathetic responses
- Affective responses (placebo, fear, kinesophobia)
- Decreasing perceived threat
What does manual therapy do?
“a mechanical force from MT initiates a cascade of neurophysiological responses from the peripheral and central nervous systems which are then responsible for clinical outcomes”.
Changes in the nervous system and psychological state (eg. confidence)
What do you say to the patient about reasons for using manual therapy?
Trying to reduce the acute/strong pain just to get your back moving
- Help with the pain
- Get them moving
What are 4 things that manual therapy does not do?
- Reposition or realign joints
- Lengthen muscles, tendons or ligaments
- Reduce muscle tone for a significant period
- Break down scar tissue or adhesions Only temporary and are neurophysiological
What are 3 factors that determine what technique to choose in the treatment?
- Position tolerated by the patient
- Eg. prone, supine, side lye –> start with this
- The patient’s comfort is SO much more important than the manual therapy
- Severity and irritability of symptoms
- Findings on the physical examination
- ROM Restriction into any specific movement?
- Manual examination
- Movement restriction

In the lumbar spine, the selection of manual therapy technique based on _______ of movement restriction or ______.
direction; symptoms
What are 2 situations where the central postero anterior (P-A)glide is used?
- Sagittal movement loss or pain
- Where prone is tolerated

How can you progress the central A-P glide?
End range problem?
- Done in a bit of extension
- On elbows

How can you regress the central A-P glide?
- Done in flexion
- Pillow under legs

What are 2 situations where the unilateral postero-anterior (P-A) glide is used?
- Movement loss in any plane.
- May assist with pain modulation of unilateral pain

When do you use thumb and when do you use pisiform for the unilateral P-A glide?
Only use thumbs if patient is very small and short time but pisiform is better
When do you use the segmental “reverse” lateral flexion?
Radiculopathy symptoms – lower grade

How do you do the segmental “reverse” lateral flexion?
Painful side on top
- Acute LBP
- Radiculopathy
- Not mechanical –> often chemical inflammation
Go into side flexion –> stretching area
Very hard to do grade _____ and ______ in the segmental “reverse” lateral flexion position
4; high velocity thrust
What are 4 situations where the segmental rotation mobilisation is used?
- Loss of rotation, side flexion and/or radiculopathy symptoms
- Acute pain where patient most comfortable in side lying
- Is a stronger end range technique
- Can be progressed to a manipulation

What are 4 situations where the segmental rotation mobilisation is used over segmental “reverse” lateral flexion?
- No radiculopathy symptoms
- Milder symptoms (still can be acute lower back pain)
- More tolerable
- Goes from Gr1-5 Grade 5 is high velocity thrust
What are 6 treatment techniques for SIJ symptoms?
- PA on sacrum
- Unilateral PA on Sacrum
- AP of an innominate
- Longitudinal ceph or caud on sacrum
- Either arthrokinematic glide (posterior or anterior rotation)
What 2 situations would manual therapy technique choice may depend on pain level?
- posterior rotation (activities associated with hip flexion, lumbar flexion)
- anterior rotation (activities associated with hip extension, lumbar extension)
Manual therapy is based on _____ (aggravating/easing) factors but still have to take into consideration which _____ is tolerable
aggravating; position
What are 2 situations where the posterior pelvic rotation mobilisation for SIJ is used?
- To aid posterior rotation ROM
- Improve symptoms associated with posterior rotation movements or positions

What are 2 situations where the anterior pelvic rotation mobilisation for SIJ is used?
- To aid posterior rotation ROM
- Improve symptoms associated with posterior rotation movements or positions

The selection of technique is based on the nature of _____.
pain
What are 3 characteristics of treatment techniques in severe pain?
- Technique should be short of pain production
- Lower grade (e.g. II, III)
- Position in range (physiological position of ease, e.g. if extension is the position of provocation, the patient may be positioned in flexion)
What are 2 characteristics of treatment techniques in progressing if pain improving or if pain is low?
- Technique should cause minor symptoms only (or no pain)
- Higher grade (IV or V) and position further into range or restriction
What are 4 ways to progression treatment techniques?
- increase time of application
- increase grade of technique
- combined technique or MWM
- change position in range for application
What is the first thing to do if they are able to tolerate techniques?
combined technique or MWM
If able to tolerate –> always start with high level the patient can do (MWM) Unlike exercise which progresses
What are 4 ways to perform MWMs?
- In standing (into flexion)
- In sitting (into flexion)
- In 4 point kneeling to sit to heels
- In prone to aid extension

What is the advantage of an active movement (MWM)?
Patient is actively involved –> more confident to move, showing them that they can move
What is the purpose of the belt in an MWM?
Belt is used to counterbalance the patient not used for mobilisation
- If push them –> they wont fall
What is the starting position for a MWM?
- Patient in sitting.
- Pelvis stabilised via a belt being placed around the patients ASIS’s and around the therapist’s ischeal tuberosity.
- Therapist to palpate between adjacent spinous processes.
What is the method for a MWM?
- The therapist maintains the tension on the belt throughout movement.
- The segmental level is palpated and when the patient actively moves into flexion, a sustained PA force is applied throughout the whole movement of flexion to the spinous process.
- N.B * The therapist should have bent knees and be able to lean onto the belt to increase the tension of the belt.
Manual therapy/mobilisation is more used to treat ____ (acute/chronic) LBP. Can you still use it in the other condition?
Acute
In chronic conditions –> while it can be used, do not prioritise it
What is the role of exercise in lumbar radiculopathy?
- A limited course of structured exercise is an option for patients with mild to moderate symptoms from radiculopathy
- Improving tolerance to moving –> not for improving strengthen, endurance
What is the role of spinal manipulation in lumbar radiculopathy?
Spinal manipulation is an option for symptomatic relief in patients with radiculopathy.
Do you use high velocity thrusts (grade 5) in radiculopathy?
Not a contra-indication but high velocity thrust is better for acute lower back pain rather than radiculopathy
What is the role of epidural steroid injections (ESI) in lumbar radiculopathy?
- Transforaminal ESI is recommended to provide short-term (2–4 weeks) pain relief in some patients.
- Interlaminar ESI may be considered.
- There is insufficient evidence to make a recommendation for long term efficacy of ESI.

Why is surgery for radiculopathy so common?
- They do not respond to conservative management
- Usually so disabled that they see the surgeon first rather than physio –> goes to surgery once have MRI
_______ (Different/Similar) outcomes of surgery and conservative management in long term (usually all recovered in 12 months)
Similar
Similar outcomes of surgery and conservative management in long term (usually all recovered in 12 months), why is surgery used?
Better short term relief with surgery for severe pain (not as beneficial for mild symptoms)
It depends on if they can tolerate/how bad are their symptoms, how long they can tolerate
- Whether surgery or conservative management is better
There was a general tendency for patients with more severe symptoms to choose _____ and benefit from it, even when randomized to the no-surgery group.
surgery
Both options (surgery and conservative management) eventually lead to _____ results for the majority of radiculopathy patients.
satisfactory
What can be concluded is that _____ treatment is a reasonable option for the patient with radiculopathy. 90% will resolve their symptoms without substantial medical intervention. Therefore, patient ______ and active participation in decision-making is vital
non-surgical; education
What is the optimal timing for surgical intervention for patients with radiculopathy?
- Surgical intervention prior to six months is suggested in patients whose symptoms are severe enough to warrant surgery.
- Earlier surgery (within six months–one year) is associated with faster recovery and improved long-term outcomes.
- There is insufficient evidence to make a recommendation for or against urgent surgery for patients with motor deficits.

What might mechanosensitivity mean for treatment in advice and education?
- Aimed at reducing threat value
- Messages; the nervous system is well designed to move, appreciating the mechanical continuity of the nervous system
- Understanding the behaviour of peripheral neuropathic pain can reduce the threat value and alter any unhelpful beliefs
What might mechanosensitivity mean for treatment in self management?
Modification to aggravating tasks for example
What might mechanosensitivity mean for treatment in addressing other impairments (exercise and manual therapy)?
Impairments found in muscle and articular systems and movement behaviours
What might mechanosensitivity mean for treatment in Neural tissue mobilization techniques?
Focus on restoring the ability of the nervous system to tolerate normal forces.
Failure to improve with conservative treatment doesn’t necessarily mean that s patient is a suitable candidate for ______.
surgery
What are 2 factors to thing of when determining if a referral is required or not in radiculopathy?
- what are the indications for a referral?
- They are getting frustrated/psychosocial factors OR good reasons (neurological symptoms are not getting better)
- what is the aim/expectation for outcomes of this referral? Guidelines
What do the guidelines suggest when referring a patient with radiculopathy?
- If neurological symptoms deteriorate or if there is no improvement after 2 to 3 weeks, then imaging and specialist review is appropriate.
- Refer for MRI and/or consult with and refer to the patient’s GP for a possible specialist referral – Ortho or Neuro
- Patient should be referred for imaging and specialist review if there is no improvement in leg pain (with radicular pain) after 4-8 weeks
What are the five factors that are commonly used in surgical decision-making and referrals that summarise this information have ‘enhanced specificity’?
- Dominant location of pain
- Radicular pain is the dominant symptom
- Severity of symptoms.
- Severity of radicular symptoms most relevant.
- Neurological findings.
- Neurological exam and neurodynamic (SLR)
- Duration of symptoms.
- Symptoms continuing despite 6 weeks conservative management
- Previous treatment and investigations.
- Appropriate conservative management, work and home modifications.
- Include MRI findings if already referred.
- Exercise, self-management..etc not TENS
Usually patients with radiculopathy who have not been seen by a physio will be sent away to see one before surgeon will see them as usually. Why?
most people respond to conservative management
Surgery is unneccessary if conservative treatment works
What is the role of orthopaedic physiotherapy screening clinics?
Evidence suggests the service reduces time of waiting lists, increases patient satisfaction and allows orthopaedic consultants to see a higher ratio of patients who are most appropriate for surgery.
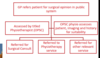
What are 9 management processes to follow for acute radiculopathy?
- Education and reassurance of favourable outcomes for majority
- Education the condition and that it can take time to settle.
- Education – regarding sensitivity of nervous system and continuity of nervous system to explain distal symptoms
- Same principles as managing a patient with acute NSLBP however the patient with Radiculopathy often:
- Will not tolerate as much activity in the acute stage
- May require more modification of activity and
- May require more rest initially for symptoms to settle (relative rest may be appropriate for a few days)
- Encourage GP visit/involvement for appropriate pain medication
- Minimise physical assessments if severe or irritable
- Manage lateral shift – self generated
- Gentle tolerated exercise and progress as symptoms settle – directional preference
- Prescribe exercise and self-management strategies as for acute LBP Focus on gradual return to function, work and other activities
When is it okay to explain anatomical pathological diagnosis to a patient?
It is okay to explain to patient for specific pain but not for non-specific
Still need to give reassurance
What is important to tell the patient when they have radiculopathy compared to non-specific LBP?
Radiculopathy are more severe
Need to be more gradual than non specific LBP Still want to encourage them though
What are 4 characteristics that must be included in the manual therapy of radiculopathy?
- Treat in a position of ease
- Techniques should try not to compromise neural interface
- Indirect neurodynamic techniques
- Pain relief positioning and advice
The presence of ____ symptoms should not deter progressing function, activity or therapy approaches
radicular
In radiculopathy, consistent monitoring of function and symptoms should inform ______.
management
_____ of symptoms get better quite significantly in radiculopathy while it take 14.5 months in the study.
Majority
What is the a priority in ongoing management of radiculopathy?
monitor Neurological signs and symptoms
The international consensus is that first 6-8 weeks, _____ treatment is indicated. Why?
conservative as most patients will rapidly improve and recover
What are 3 strategies in conservative management of radiculopath?
- Progress functional ability (rather than focussing just on pain reduction)
- Consider motor control retraining approaches if appropriate
- Manage secondary impairments – ROM, loss of strength, disability, work restrictions and difficulties
What are the 6 principles in the management of SIJ pain?
- Patient education
- Give them info about their pain, give advice and what they can do
- Postural or activity modification
- What aggravates symptoms and they try to modify? –> get prolonged standing
- Joint mobilization (neurophysiological effect)
- Joint manipulation (neurophysiological effect)
- Muscle stretching
- Strengthening – based on physical assessment findings – enhancing weight bearing capacity, including posterior chain, possibly aimed also at enhancing motor control. Joint mobilisation and strengthening
SIMILAR PRINCIPLES TO LBP (unless inflammatory condition)
The principles for the management of SIJ is ____ (similar/different) to LBP management. When is the exception?
similar
inflammatory condition
Should you tell them in the session that they might need surgery if conservative treatment is not effective in improving the radiculopathy?
Need to give all the information about management to patient
- Course of action if they do not get significantly better
- Might need to refer for a scan and surgery if not better
- Can take a few weeks to settle down
What are 8 skills in the management of radiculopathy?
- Monitoring neurological symptoms through neuro assessment
- Priority in day 1
- Directional preference assessment and exercises
- Acute ROM exercises
- Motor control assessment and exercises
- Advice and education – self management, postural strategies
- Reverse lateral flexion technique
- Segmental rotation technique
- Nerve mobilisation techniques
- Try to reduce the sensitivity of the nerves
What is the Priority in day 1 for the management of radiculopathy?
Monitoring neurological symptoms through neuro assessment


