Joint Pain Flashcards
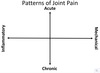
How would you frame the DDx of joint pain?
Acute vs. chronic
Inflammatory vs. mechanical
Polyarthritis vs. oligoarthritis vs. monoarthritis
What are the patterns of joint pain?

A 14 YO girl has had pain in her fingers & wrists & this has made her clarinet performances more difficult over the last couple months. She has also had tactile fevers, fatigue, mouth sores & erythema of her cheeks for the last month. She thinks her hair is thinning & she has lost 5 lb in 2 wks. She has missed the last week of school.
She is tired appearing. Her eyes seem puffy. There is trace pitting edema of her ankles.
What is your top differential?
Systemic Lupus Erythematosus (SLE)
Depression/Chronic Pain Syndrome
How does this present?
What questions should you ask?
- Fatigue, weight loss, missing school, diffuse pain
- Recent stressors? Disinterest in usual activities? Difficulty sleeping?
EBV Infection
How does this present?
What questions should you ask?
- Fatigue, diffuse pain
- Sick contacts? Swollen LN? Sore throat?
Rheumatoid Arthritis
How does this present?
What questions should you ask?
- Multiple joint pain, fatigue
- Persistent swelling/stiffness of joints?
Psoriatic Arthritis
How does this present?
What questions should you ask?
- Multiple joint pain
- Persistent swelling/stiffness of joints?
- Rash?
- Nail abnormalities?
- FHx of psoriasis?
Inflammatory Bowel Disease
How does this present?
What questions should you ask?
- Multiple joint pain, mouth sores, weight loss, fatigue, hair loss
- Abdominal pain? Diarrhea? Bloody stools?
Systemic Lupus Erythematosus
How does this present?
What questions should you ask?
- Multiple joint pain, mouth sores, facial rash, fatigue, weight loss, hair loss, missing school
- Has facial rash been persistent?
- Photosensitive rashes?
- Leg swelling?
Common Variable Immune Deficiency
How does this present?
What questions should you ask?
- Multiple joint pain, fatigue, weight loss
- History of sinopulmonary infections?
What laboratory tests would you do for these?
- SLE
- EBV
- Hypothyroidism
- Rheumatoid arthritis
- IBD
- CVID
- SLE
- CBC, Cr, UA, ANA, anti-dsDNA, anti-Smith Ab
- EBV
- Monospot, EBV titers
- Hypothyroidism - TSH
- Rheumatoid arthritis
- RF, CCP, hand X-rays
- IBD
- CBC, ESR, CRP, stool guiaic
- CVID
- Immunoglobulin panel, vaccine titers
What are the two main categories of symptoms in Systemic Lupus Erythematosus?
- Mucocutaneous manifestations
- “-itis”
What are the mucocutaneous manifestations in SLE?
- Oral ulcers - hard palate
- Malar rash - crosses nasal bridge, spares nasolabial folds
- Rashes often photosensitive
What are the “-itis”-es of SLE?
- CNS inflammation
- Cerebritis (seizures, psychosis)
- Transverse myelitis
- Nephritis
- Arthritis
- Small joints
- Hands & wrists
- Serositis
- Pericarditis
- Pleuritis
What are the laboratory abnormalities seen in SLE?
-
Auto Ab
- ANA (sensitive but not specific)
- anti-dsDNA, anti-Smith (specific but not sensitive)
- Coombs
-
Cytopenia
- Leukopenia, lymphopenia
- AIHA, ITP
- Low complement
If our patient with SLE had normal urine but platelets consistently <20K, what would you treat her with?
- Steroids
- IVIG
- Rituximab
- Belimumab - not typically used for thrombocytopenia, but a related B-cell therapy
What is the pathophysiology of SLE nephritis?
How is this manifested in the lab abnormalities?
Type III Hypersensitivity
- (Auto)Ab + (Auto)Ag = immune complex (IC)
- IC deposit in tissues
- Deposited IC elicits inflammation including PMN infiltration
- Inflammation results in tissue damage
- Labs
- Immunofluorescence for IgG stains dermal-epidermal junction
- Lupus Band
A 14 YO girl has had pain in her fingers & wrists and this has made her clarinet performances more difficult over the last couple months. She has also had fatigue & mouth sores. On exam you see scaling on the extensor surfaces & nail pitting.
What is the most likely diagnosis?
Psoriatic Arthritis
What are the patterns of joint involvement in Psoriatic Arthritis?
- DIP predominant arthritis
- Oligoarticular (typically large joints)
- Polyarticular
- Axial involvement (uncommon)
What are some other presenting characteristics of Psoriatic Arthritis?
What is the genetic association?
- Enthesitis
- Dactylitis (“sausage digits”)
- Can be associated w/ HLA-B27
- Arthritis can precede onset of psoriasis
How does Psoriatic Arthritis present on the skin?
What is the Auspitz sign? Koebner phenomenon?
How does this correlate with arthritis severity?
- Lesions
- Well-demarcated erythematous lesions w/ silvery scale
- Auspitz sign - bleeding w/ peeling of scale
- Koebner phenomenon - rash at sites of trauma
- Most common distribution w/ plaque psoriasis - extensor surfaces of elbows & knees
- Severity does not correlated with arthritis severity
- Nail pitting increases the risk of arthritis
How is Psoriatic Arthritis treated?
- NSAIDs (arthritis only)
- Methotrexate
- Anti-TNF medications (etanercept, adalimumab, infliximab)
- Costimulation blockade (CTLA-4 Ig, abatacept)
- Anti-IL17 (secukinamab)
- Anti-IL12/23 (ustekinumab)
- JAK/STAT inhibitors (tofacitinib)
- PDE-4 inhibitors (apremilast)
14 YO female presents w/ a 2 wk history of very painful joints, initially her R knee, then her L wrist, and now her L ankle. She has had hives, and is fatigued. She has had mild dsypnea w/ ambulation. She is tachycardic & has a II/VI holosystolic murmur at the apex radiating to the axilla. Her joint exam is normal except for severe pain w/ ROM of the L ankle w/ mild swelling. She has an urticarial-like rash on her trunk. She had a sore throat about a month ago.
What is the Problem List?
What is the Leading DDx?
- Problem List
- Migratory polyarthritis
- Urticarial rash
- Murmur radiating to axilla (mitral valve)
- History of sore throat
- Leading DDx: acute rheumatic fever
14 YO female presents w/ a 2 wk history of swelling & stiffness intitially her L knee then progressed to also involve her L wrist, then both wrists w/ stiffness of her fingers. She has had fever, rash & is fatigued. She has swelling, warmth, erythema, tenderness & severe pain w/ ROM of her R knee, L wrist & L ankle. She has small pustules on her hands. She had a sore throat about 1 mo ago.
What is the Problem List?
What is the Leading DDx?
- Problem List
- Additive polyarthritis (very painful & erythematous)
- Fever
- Pustular rash
- History of sore throat
- Sexually active
- Leading DDx: gonococcal arthritis









