Dizziness Flashcards
What is your first step in evaluating a patient who presents with dizziness?
- Differentiate vertigo from presyncope from unsteadiness
- True vertigo should have an aspect of movement (spinning of self or room)
What are some other things that people report as dizziness? (7)
- Presyncope
- Unsteadiness of gait (peripheral neuropathy)
- Blurry or double vision
- Cloudy mentation - disorientation
- Migraine aura
- Seizure aura
- Anxiety
If the patient has vertigo, what other questions should you be asking?
-
Are there associated symptoms?
- Cranial nerves
- Hearing
- Ataxia
- Cardiovascular
- Onset, timing, duration, stimulating activities
- Peripheral vs. Central vertigo
What is the difference between peripheral & central vertigo?
-
Peripheral vertigo
- Delay for stimulation (1-2 sec)
- Exhibits fatigue
-
Central vertigo
- No delay
- Much more profound & prolonged
- Little fatigue
What is the definition of vertigo?
- Imbalance to input from either inner ears, vestibular nuclei or vestibular tracts
- Sensation of movement w/o any
- Misperception of movements one is making
What are the peripheral causes of vertigo?
- BPPV
- Meniere’s
- Vestibular Neuronitis
- Labyrinthitis
- Direct trauma
What are the central causes of vertigo?
- Stroke - lateral medullary, cerebellum
- Brainstem or cerebellar mass
- Medications
- Migraine
- MS
- Anxiety
What parts of the ear detect linear acceleration?
- Maculae in the utricle & saccule
- Linear movement = both ears perceive in the same way

What parts of the ear detect angular motion?
- Semicircular canals detect angular motion, each in its own plane
- X, Y, Z plane
- No otoliths but have gel –> gel moves against the semicircular canal

Identify the labeled structures:

- Lateral Semicircular Canal
- Vestibule
- Internal Auditory Canal
Identify the labeled structures:

- Posterior Semicircular Canal
- Mastoids
What are the 4 vestibular nuclei?
-
Caudal Pons
- Superior vestibular nucleus
- Lateral vestibular nucleus
-
Rostral Medulla
- Medial vestibular nucleus
- Inferior vestibular nucleus

_______, _______, & ________ are places where you get lesions that cause vertigo.
These often disturb the _____________ tracts.
cerebellum, pons, medulla
vestibulospinal

Mrs. Jones is a 67-year-old woman w/ a PMH of smoking & HTN. She takes lisinopril 10 mg daily. She presents to her primary physician complaining of dizziness.
She describes 2 days of having a severe sensation of spinning when she sits up or rolls over, lies down or even when she turns to the left. She has to sit down or hold on & close her eyes to keep from falling or throwing up. It goes away after ~30 sec. She does not have any hearing changes or other neurologic symptoms.
Vitals, mental status, cranial nerves, motor, sensory, all normal. Hearing is normal.
What does Mrs. Jones have?
Benign Paroxysmal Positional Vertigo
What causes BPPV?
How does it usually present?
How is it treated?
- Secondary to a free-floating canalith usually within 1 of the semicircular canals. The canalith creates turbulent flow within the endolymph resulting in the sensation of motion (vertigo).
- Patients with all 4 of the following criteria usually have BPPV
- Recurrent vertigo
- Duration of attack < 1 minute
- Symptoms invariably provoked by changing head position
- Lying down or turning over in bed OR
- 2 of the following: Reclining the head, rising from supine, or bending forward
- Not attributable to another disorder
- Treatment: Epley maneuver
What are the components of a complete exam on a patient with dizziness?
What are the possible findings and what do they indicate?
-
Look for nystagmus
- If there is no nystagmus, not ear related
- Vertical nystagmus is central
- Direction changing is central
-
Look for associated symptoms
- Ataxia, particularly one-sided = cerebellar lesion
- Dysphagia, diplopia, facial sensation loss, Horner’s syndrome, skew deviation = brainstem stroke
- Weakness, numbness, other neurologic findings = consider a large stroke, tumor or a multifocal process such as MS
What is a skew deviation?
How is it tested for?
-
Eyes are not focused on the same point
- Up & down or side-to-side
-
Cover to cover test
- Have patient look at your nose w/ both eyes
- Cover each eye individually
- If eyes are aligned, nothing will happen
- If eyes not not aligned, they will align as they remove their hand to look at your nose
What is the Dix-Hallpike maneuver?
What do you expect to see?
- Drop the patient backwards & then turn the head sideways & down towards the floor
- Ask the patient to look toward the floor & watch for nystagmus
- In peripheral nystagmus you will see it develop after a few seconds & last for under a minute
- Patients can get sick so be careful
- Also may need assistance to do it safely

Fill in the blanks:


In BPPV, where are the otoconia after they are displaced from the utricle?
Posterior canal

What would your patient have if they get dizzy when they stand up?
How is this tested for?
Orthostatic hypotension
- Usually more lightheaded than vertiginous
- Medication
- Hyponatremia/dehydration
- Autonomic failure
- Important to test orthostatics WELL
- Start supine, then sitting, then standing w/ >3 min in each position prior to testing
- >20 mmHg drop in SBP or >10 mmHg drop in DBP after 3 min is diagnostic
- Tilt table testing for autonomic insufficiency

What would you patient have if they get dizzy (true vertigo) with standing for a long period of time?
Vertebrobasilar insufficiency
- Stenosed or occluded vertebral arteries BILATERALLY
- Stenosed or occluded basilar artery
- “Locked-in syndrome”
- Ischemia of vestibular nuclei in the pons & medulla can present w/ vertigo
- Often w/ other associated symptoms such as weakness, diplopia, dysarthria
What is the best type of imaging for Vertebrobasilar insufficiency?
How is it treated?
Vascular imaging
- MRI won’t tell you anything
- Take her off anti-hypertensives
- Possible stenosing (but not that effective)
- Don’t lower BP (orthostatis is disastrous)

Mr. Smith is a 32-year-old man w/ a PMH of migraine. He presents w/ complaints of dizziness to the ED.
He describes the sensation of falling to the left which particularly occurs when he is walking. He often bumps into things when he walks. He feels like he is walking on a boat sometimes & feels himself swaying when he stands still. He has been dropping things in his left hand as well. He denies hearing changes & is not aware of any other neurologic symptoms.
Exam normal except for slow rapid alternating movements, mild ataxia of the L arm, & some slow difficulty w/ tandem gait. Decreased tone on L arm & leg.
What does Mr. Smith have?
Cerebellar lesion/stroke/hemorrhage/tumor/trauma
What is this?
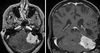
Benign meningioma of the left cerebellum
- Dural tails characteristic of meningioma
- Cause problems by mass effect
- Surgical resection or radiation to shrink
What are the 7 common signs of cerebellar disease?
- Scanning speech
- Nystagmus
- Abnormal finger to nose test
- Abnormal rapid alternating movements
- Abnormal heel to shin test
- Wide based & staggering gait, often falling to the side of the lesion
What tumors of the brainstem & cerebellum are more common in children?
- Medulloblastoma
- PNET
- Pineal tumors
- Ependymoma
- Astrocytomas of BS & cerebellum (25%)
- Gliomas (almost exclusively children/young adults)
Tumors in the cerebellum & brainstem
__________ are more common in adults.
________________ from meningioma, acoustic neuroma.
Metastases (lung, breast, testicular, renal)
Extra-axial cerebellar compression
What is this? (younger patient)

Pilocytic astrocytoma
- Motor tracts not affected
- Problems w/ sensation, balance, vertigo, eye movements
What is Lateral Medullary (Wallenberg) Syndrome?
How does it present?
How is it treated?
- Often from vertebral artery dissection (PICA)
- Rare, but more common in young people
- Some or all of:
- Dysphagia
- Horner’s syndrome
- Ataxia
- Sensory loss
- Nystagmus
- Vertigo
- Pain up neck for days after trauma
- Anticoagulation: heals on its own
- Good prognosis

What is this?

Vertebral artery dissection (PICA)
What is this?

Multiple Sclerosis
Multiple plaques perpenticular to ventricles
How does a migraine/vestibular migraine typically present?
- 4-72 hours
- Diplopia/dysphagia but rare
- Episodic nature, happened more than once
- Sensitivity to light & sound during event
- Phonophobia, nausea
How does anxiety-induced dizziness present?
What is another cause of dizziness?
- Vertigo & dizziness
- Lightheaded, non-specific
- Precipitating event
- Room full of people
- “feeling of doom”
- Palpitations
- Medication side effects can also cause dizziness
What types of medications cause lightheadedness/presyncope/vague dizziness?
- BP meds
- Psych meds
- Neuro meds
What types of medications cause true vertigo via cerebellar degeneration?
- Phenytoin
- Decades to do this
- Used for short-term only (status epilepticus)
- Ethanol
- Also B12 deficiency, sniffing glue
What types of medications cause true vertigo via vestibulotoxicity?
- Aminoglycosides
- Gentamicin
- Tobramycin
- Chemotherapy
- Cisplatin
- Vincristine


