Dementia Flashcards
_________ is a MEDICAL EMERGENCY.
Delirium
What are the 3 steps in the Cognitive Continuum?
- Preclinical [Normal Cognitive function]
- Minor neurocognitive disorder [Mild Cognitive Impairment]
- Major neurocognitive disorder [Dementia]
What are Instrumental Activities of Daily Living?
- Cooking
- House cleaning
- Laundry
- Management of medications
- Management of the telephone
- Management of personal accounts
- Shopping
- Use of transportation
What are Activities of Daily Living (ADLs)?
DEATH
- Dressing
- Eating
- Ambulating
- Toileting
- Hygiene (Bathing)
What is the Mini-Cog Exam?
What are the 3 steps?
- Ask patient to remember 3 unrelated words
- Banana, Sunrise, Chair
- Village, Kitchen, Baby
- Leader, Season, Table
- Ask patient to draw the face of a clock. After the numbers are on the clock, ask patient to draw hands to read 10 min after 11:00
- Ask patient to recall the 3 words
How is the Mini-Cog exam scored?
- 3 recalled words
- Negative for cognitive impairment
- 1-2 recalled words + normal clock
- Negative for cognitive impairment
- 1-2 recalled words + abnormal clock
- Positive for cognitive impairment
- 0 recalled words
- Positive for cognitive impairment
What is the laboratory work up for all patients?
- CBC
- Electrolytes
- Creatinine
- Glucose
- TSH
- Vitamin B12
What is the laboratory work up for selected cases?
- HIV serology
- RPR
- Heavy metal screening
- LFTs
- MMA
What is a normal score for the Montreal Cognitive Assessment test? (MOCA)
> 26/30
How are Neurocognitive Disorders defined according to DSM-V?
- Delirium
- Neurocognitive disorders [not delirium]
- Minor
- Major
- Further subdivision based on etiology
What is the Dementia/Major Neurocognitive Disorder Diagnostic Criteria for DSM-5?
- Evidence of significant cognitive decline from a previous level of performance in one or more cognitive domains based on:
- Concern of the individual, knowledgeable informant, or the clinician that there has been a significant decline in cognitive function AND
- A substantial impairment in cognitive performance (documented)
- The cognitive defects interfere w/ independence in everyday activities
- The cognitive defects do not occur exclusively in the context of a delirium
- The cognitive defects are not better explained by another mental disorder
What are the 6 cognitive domains?
- Complex attention
- Executive function
- Learning & memory
- Language
- Perceptual-motor
- Social cognition
What are the 4 components of a dementia diagnosis?
- >2 cognitive domains affected
- Impaired occupational function
- Evidence of progression
- No alternative diagnosis
Mild Cognitive Impairment (MCI)
- Onset
- Domain
- Motor
- Progression
- Imaging
- Onset: Gradual
- Domain: >Memory
- Motor: Rare
- Progression: 12%/yr to Alzheimer’s
- Imaging: Normal or Alzheimer’s pattern
Alzheimer’s Disease
- Onset
- Domain
- Motor
- Progression
- Imaging
- Onset: Gradual
- Domain: Memory, Language, Visuospatial
- Motor: Late
- Progression: Gradual (8-10 yrs)
- Imaging: Atrophy, small hippocampal volume
Vascular Dementia
- Onset
- Domain
- Motor
- Progression
- Imaging
- Onset: Sudden & gradual
- Domain: Depends on location
- Motor: Depends on location
- Progression: Depends on ischemia pattern
- Imaging: Cortical or subcortical MRI changes
Lewy Body Dementia
- Onset
- Domain
- Motor
- Progression
- Imaging
- Onset: Gradual
- Domain: Memory, visuospatial, hallucinations, fluctuating
- Motor: Parkinsonism
- Progression: Gradual & cognitive fluctuations
- Imaging: Atrophy
What is the prevalence of dementia by age?
- 65-75
- >75
- >85
- 65-75
- Outpatient: 2.1%
- Inpatient: 6.4%
- >75
- Outpatient: 11.7%
- Inpatient: 13.0%
- >85
- Outpatient: -
- Inpatient: 31.2%
What are the typical pathologic findings of Alzheimer’s disease?
- Decreased brain weight
- Atrophy of gyri & widening of sulci
-
Senile Plaques (amyloid)
- Diffuse: EC accumulation of Aß protein
- Neuritic: EC accumulation of Aß protein & tau containing neurites
-
Neurofibrillary Tangles
- Intraneuronal accumulation of abnormally phosphorylated tau (normal MT associated protein)
- Not unique to AD, found in other degenerative diseases
What is the typical prognosis of Alzheimer’s disease?
- Estimates of median survival: 5-9 yrs
- 3 yrs (2.7-4 yrs)
Dementia can lead to impairments in…..
“Make safety a priority before it’s a problem!”
- Judgment
- Orientation
- Behavior
- Physical ability
What are some safety issues in dementia?
- Home environment
- Medications
- Firearms
- Wandering & getting lost
- Driving
What is the second most common type of dementia?
What is the second most common type of degenerative dementia?
Vascular dementia
Lewy body dementia
Lewy Body Dementia
- Prevalence
- Sex & Age
- Inheritance
- 10-20% of dementias
- M > W
- Mean age of onset = 75 yrs
- Most cases sporadic
- Autosomal dominant inherited form
- alpha-synuclein gene
What are the clinical features of Lewy Body Dementia?
- Gradual cognitive decline; Dementia often presenting symptom
- Early in course: attention, visuospatial & executive function, poor job performance getting lost
- Later in a course memory is impaired
What are the 3 core clinical features of DLB?
-
Fluctuation in alertness
- Seconds to days
- In btwn episodes functioning may be normal
-
Vivid visual hallucinations
- Simple or complex
- Early sign, often precedes motor symptoms
-
Parkinsonism
- Bradykinesia & rididity
- Tremor is less common than PD
- Motor symptoms develop later in a course of illness or in concordance w/ dementia
- If motor symptoms present >1 yr before dementia, think PD dementia
What are some suggestive features of DLB?
- Repeat falls
- Neuroleptic sensitivity resulting in severe pakinsonism, typical more than atypical, not dose related
- REM sleep disorder - vivid dreams in REM sleep w/o muscle atonia, patients act out their dreams
- Syncope or LOC
- Orthostasis - associated w/ carotid sinus sensitivity
- Autonomic dysfunction - urinary incontinence or retention, constipation, impotence
- Auditory hallucinations & delusions
- Depression - 40% will have MDD
In DLB, what does MRI show?
What does SPECT/PET show?
- MRI - generalized atrophy
- SPECT/PET scan - decreased perfusion in occipital lobes
What is the neuropathology of Lewy Body Dementia?
Lewy bodies
Alpha-synuclein
What are Lewy Bodies?
round, eosinophilic, intracytoplasmic inclusions in the nuclei of neurons

What is alpha-synuclein?
Where is it found?
- Major component of Lewy bodies
- Deep cortical areas throughout the brain
- Anterior, frontal & temporal lobes
- Cingulate gyrus & insula
_________ are often present but NFTs are rare in DLB.
____________ are sparse or absent.
Amyloid plaques
NFTs
Neuronal loss in DLB is greater in __________, ____________, __________ and _____.
- Frontal lobes
- Nucleus basalis of Meynert
- Substantia nigra
- LC
In DLB, there are decreased cortical levels of _____________.
choline acetyl transferase
What is the prognosis of DLB?
What are some non-pharmacologic treatments?
- Prognosis is very poor
- No therapies are known to alter the natural progression of the underlying neurodegeneration or time of death
- Average survival is similar to that of AD, about 8 years
- Non-pharmacologic treatments is emphasized: addressing environmental, medical, psychologic & social factors; caregiver education & support
What is the pharmacological management of DLB?
- Pharmacological treatment is symptomatic, no FDA approved medications
- Acetylcholinesterase inhibitors can offer benefit in realms of apathy, confusion, hallucination & somnolence
- When antipsychotics are needed, atypical agents are preferred (Olanzapaine, Quetiapine) w/ the goal to avoid long-term usage
- Antiparkinsonian medications: Levodopa-carbidopa well tolerated, avoid anticholinergics
- REM sleep behavior disorder: low dose of Clonazepam; Melatonin might be helpful
What does DLB look like on brain imaging?
- MRI - generalized atrophy
- SPECT/PET scan - decreased perfusion in occipital lobes
What does AD look like on brain imaging?
- MRI
- generalized atrophy
- shrinkage of hippocampus
- enlarged ventricles
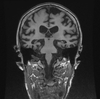
What does FTD look like on brain imaging?
- MRI - frontal & temporal atrophy
- PET scan - decreased metabolism in frontal & occipital lobes

What does vascular dementia look like on brain imaging?
- MRI - white matter lesions

Which 3 are the core features of DLB?
- Visual hallucinations
- Repeated falls
- Parkinsonism
- Cognitive fluctuations
- Visual hallucinations
- Parkinsonism
- Cognitive fluctuations
Which 3 are the supportive features of DLB?
- Neuroleptic sensitivity
- REM sleep disorder
- Delusions
- Non-REM sleep disorder
- Neuroleptic sensitivity
- REM sleep disorder
- Delusions
Alpha-synuclein is a major component of….
- NFTs
- Senile plaques
- Lewy bodies
- Amyloid-beta protein
Lewy bodies
65 YO male has been frustrated as he is forgetting phone numbers & misplaces his keys. Otherwise he is doing well & his daily functioning is not impaired. His father had Alzheimer’s disease. On MMSE he scored 28/30, he lost 2 points on delayed recall. What is the most likely diagnosis?
- Vascular dementia
- Alzheimer’s disease
- Mild cognitive impairment
- Lewy body dementia
Mild cognitive impairment
What is the second most common type of dementia?
- Parkinson’s disease dementia
- Frontotemporal dementia
- Vascular dementia
- Alzheimer’s disease
Vascular dementia
Mr. Smith is a 60 YO male who was brought by his son for evaluation. Son reported that 4 yrs ago his father become social inappropriate, making sexual comments to his female neighbors. Mr. Smith was evicted from his apartment due to poor environmental hygiene & complaints made by his neighbors as he was urinating in a hallway.
On neurophysiology testing Mr. Smith showed executive & visuospatial deficits along w/ deficits in attention & language. The memory is preserved however he is not able to work or live independently.
Labs were w/i normal limites. On physical exam he had no focal signs & didn’t exhibit any signs of movement disorder. What is the most likely diagnosis?
- Alzheimer’s disease
- Lewy body dementia
- Frontotemporal dementia (FTD)
- Vascular dementia
Frontotemporal dementia (FTD)
70 YO male came for evaluation due to memory problems that started a year ago. Physical exam was significant for bradykinesia, rigidity & pill-rolling tremor. You found in his history that he has parkinsonian features for the past 5 yrs & has been taking sinemet. Neurophysiology testing was done & showed deficits in executive function along w/ visuospatial, memory & language impairment. He has no Hx of stroke. What is the most likely diagnosis?
- Frontotemporal dementia
- Lewy body dementia
- Parkinson’s disease dementia (PDD)
- Vascular dementia
Parkinson’s disease dementia (PDD)


