Introductory Veterinary Pathology Flashcards
Describe cellular dysplasia.
Alteration in the size, shape or organization of a tissue
What is aplasia?
Organ does not develop at all and only rudimentary tissue is present
What is agenesis?
Failure of any development due to lack of embryonic primordial tissue
Describe hydropic degeneration.
- Cellular injury
- Reversible
- Often results from hypoxia as reduced ATP levels cause cell to switch to anaerobic metabolism causing depletion of glycogen and accumulation of lactate and inorganic phosophates which inhibits membrane sodium/potassium pump and water moves into the cell
- Characterized by cytoplasmic swelling and extensive vaculolation which does not histopathologically stain for fat (Oil Red O) or glycogen (Periodic Acid-Schiff Stain)
- Can progress to ‘Ballooning Degeneration’
What is oncotic necrosis?
Swelling of cell due to excessive water entry (hydropic degeneration) and subsequent cellular death
Describe coagulative necrosis.
- Cell death typically caused by ischemia or infarction.
- The architecture of dead cells is preserved for at least a couple of days.
Describe caseous necrosis.
- Form of cell death in which the tissue maintains a cheese-like appearance. The dead tissue appears as a soft and white proteinaceous dead cell mass.
- Evidence of chronic lesion
- May develop dystrophic calcification
- On microscopic examination with H&E staining, it is characterized by acellular pink areas of necrosis surrounded by a granulomatous inflammatory process.
Decribe gangrenous necrosis.
- Type of necrosis caused by a critically insufficient blood supply
- Grossly, tissues appear black in colour
What is dystrophic calcification?
- Calcification occurring in degenerated or necrotic tissue
- It occurs in areas of cell necrosis in which activated phosphatases bind calcium ions to phospholipids in the membrane.
What is Karyorrhexis?
The breaking of nuclei into pieces.
What is pyknosis?
The apparent shrinking of the cellular nucleus upon microscopic investigation
Describe lipidosis.
- Intracellular (intracytoplasmic) accumulations of fat. The liver is susceptible because of its central role in lipid metabolism
- Mechanisms
- Excessive free fatty acids from diet or adipose tissue breakdown
- Toxic damage affecting metabolism of fatty acids and triglycerides
What is fatty infiltration?
- Replacement of cells by adipocytes
- Can occurs because of old age or obesity
What is hameosiderin?
Iron storage complex found in red blood cells
What is an empyema?
- the collection of suppurative/ purlent inflammatiory fluid (pus) in a cavity in the body
- Dominated by neutrophils, both dead and alive
- Contains dead host cells
- Often caused by bacteria
- May become walled off by granulation or fibrous tissue causing an abcess
How does fibrinous inflammation occur?
- Forms as a result of increased vascular permeability and fibrinogen escape from the vascular system which polymerizes to fibrin by thrombin
- Acute phenomenon
Describe mucus/catarrhal inflammation.
- Caused by mucus hypersecretion which accompanies inflammation
- Often found in respiratory and gastrointestinal tracts where mucus-secreting cells are prominent
Describe this gross pathology.

Caseous necrosis in the pleura
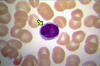
What cell is this?

Eosinophil of a horse
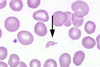
Describe the prominent process occuring

Erythrophagocytosis
Describe the process occuring

Fatty infiltration of the muscle fascicle
Describe the gross pathology

- Fibrinous inflammation
- Acute phenomenon which occurs as a result of increased vascular permeability and fibrinogen escape from the vascular system which polymerizes to fibrin by thrombin
What cell type is pictured here?

Fibroblasts
Describe this process

Fibrosis of the liver
Describe this process

- Gangrenous necrosis of a pig’s ear
- Occurs with infarct
- Follows on some cases of coagulative necrosis
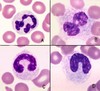
What cell is pictured here?

Giant cell
What cellular process is pictured here? What stain was used?

- Glycogen accumulation in the cells of the proximal tubule
- Periodic acid-Schiff (PAS) was used to detect the glycogen polysaccharide
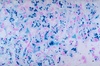
What stain is being used in this slide and what is being depicted?

- Gram stain to visualize bacteria
- Gram negative bateria stain pink
- Gram positive bateria stain purple
What stain is being used in this slide and what is it depicting?

- Jones stain which visualizes basement membranes
- This is a slide of the kidney
What process is being depicted here?

Karryohexis
What process is being depicted here?

Karyolysis
What process is being depicted here/

Lipidosis of the liver
What cell is being depicted here?
Lymphocyte
What cells are being depicted here?

Macrophages
What histological stain is being used and what is it depicting?

- Mason’s trichrome stain of the liver
- Stains connective tisse in green
What cell is being depicted here? Describe some of its characteristics.

- Mast cell
- derived from the myeloid stem cell. It is a part of the immune and neuroimmune systems and contains many granules rich in histamine and heparin
What cells are being depicted here?
- Neutrophils
What stain is being used in this histological slide and what is it depicting?

Oil red O stain highlighting lipid in red
What stain is being used in the following histological slide and what is it depticting?

Periodic acid-Schiff (PAS) stain of the kidney for visualizing glycogen
Describe the appearance of karyolysis histologically. What causes this?
Karyolysis appears histologically as a nucleus which fades into the background. This is caused by the complete dissolution of the chromatin of a dying cell due to the enzymatic degradation by endonucleases.
What stain is being used here and what does this stain highlight?
- Perl’s Prussian Blue reaction stains is being used which stains haemosiderin (blood breakddown product) blue
- This particular slide is depicting hepatocytes
What pathology is being shown here?

Purulent and suppurative exudate of the thorax
What process is depicted here?

Pyknosis: the shriking of the cell nucleus
How can this group of cells be described?

- Pyogranulomaous inflammation: inflammatory process in which there is infiltration of polymorphonuclear cells into a more chronic area of inflammation characterized by mononuclear cells, macrophages, lymphocytes and possibly plasma cells
- This particular side is of an infected lymph node
What stain is being used here and what structure is/are being highlighted?

- Toluidine blue stain is used to visualize acidic structures
- Immune cell graunlocyte granules will appear blue histologically upon staining
What stain is being used in this histological slide and what is it hightlighting?

- Ziel-Neilson stain for mycobacteria mast cell granules
- This particular slide is of a sputum sample
Describe the following lesions

Depressed
Describe the following lesion

Diffuse
Describe the following lesion.

Elevated
Describe the following lesion.

Flat, multifocal
Describe the following lesion.

Focal
Describe the following lesion

Multifocal lesion
Describe the following lesion

Multifocal to coalescing lesion
Describe the following lesion

Pedunculated lesion
Describe the following lesion.

Segmental lesion
Describe the following lesion.

Sessile lesion
How would you describe the borders of this lesion?

Poorly demarcated
How would you describe the borders of this lesion?

Well-demarcated
Describe the following.

- Pathognomonic acute liver fluke
Describe the following.

Pathognomonic Chronic liver fluke
Describe the following.

Pathognomonic congenital renal cysts
Describe the following

Pathognomonic Lungworm infection
What is algor mortis?
- Cooling of the body after death
- Slower in animals with more vicera (ruminants, for example)
What is rigor mortis, why does it occur, and what factors determine its onset/duration?
Rigor mortis occurs 2-4 hours after death. Because ATP is required for actin and myosin to release, after death (when no more ATP is produced) muscle fibres undego sustained contraction causing skeletal muscle rigidity. This is compounded by influx of calcium due to failure of membrane pumps. Metabolic activity is also increased.
- Duration/onset dependent on
- Glycogen content of muscle
- Glycogen fuels ATP production. With less glycogen there will be a faster onset
- Temperature
- A higher temperature causes faster onset
- pH of muscle
- Glycogen content of muscle
- High pH delays or inhibits onset
Describe putrefaction.
- Invasion of dead tissue by anaerobes such as Clostridia
- Causes tissue to turn green/brown due to combination of haemaglobin breakdown and formation of hydrogen sulfide
- Causes emphysema (excess gas) to be liberated
- No use in performing histopathology on a specimen which has been putrefied
What does turbid fluid indicate?
Presence of cells
What is pseudomelanosis?
- Black-blown colour of tissue caused by hydrogen sulfide produced by bacteria causing tissue iron to be catalyzed to iron sulphide
- Not a pathological finding
How is anti-diuretic hormone release regualted and what does this hormone do?
- Hypoosmolar state/Hypervolaemia
- Recognized by osmoreceptors in hypothalamus which suppress secretion of ADH and cause loss of water in kidney
- Baroreceptors in left atrium detect high blood volume and blood pressure which inhibit ADH production
- The resulting greater urine production reduced blood pressure
- Hyperosmolar state
- Thirst is increase driven high plasma osmolarity as detected by the hypothalamus
- Causes stimulation of osmoreceptors in hypothalamus leading to ADH secretion and retention of water by kidneys
- Volume increase must be corrected as a hypovolaemic state is created
- Actions
- cAMP-mediated stimulation of cells of collecting duct to insert performed aquaporin-2 into apical membrane and re-absorb water
- Stimulates insertion of urea channels to allow urea exit to increase hypertonicity of interstitium
Describe the release and action of atrial naturitic peptide.
- Released in response to high blood pressure which causes heart stretching
- powerful vasodilator, and a protein (polypeptide) hormone secreted by heart muscle cells
- Downregulates channels of sodium and sodium-potassium ATPase in Principal cells
- Suppresses sodium re-absorption
- Dilates afferent arteriole and constricts efferent arteriole in the glomerulus
- Increases the GFR- increases sodium filtration
- Triggers loss of water and sodium from kidneys
- Decreases cardiac output and blood pressure
What is hyperaemia?
- Active process of areriolar dilation
- Increases blood flow
- Causes redness
- Fibrin may be apparent
- Examples: blistering, pyrexia, blushing
Describe the different types of haemorrhage sizes.
- Petechiae (petechial)
- 1-2mm diameter
- Purpura
- 3-10mm diameter
- Ecchymoses (Ecchymotic)
- 1-3cm diameter
- Suffusive/rhectic
- Major bleeding
- Involves large contiguous areas
Describe the coagulation cascade.
- Intrinsic
- Factor XII (Hageman factor) is converted to factor XIIa with exposure to thombogenic surfaces
- XIIa Converts factor XI to XIa
- XIa Converts IX to IXa
- IXa converts X to Xa and join the common pathway
- Extrinsic (Triggered by tissue thromboplasin (Factor III))
- Stimulated by tissue injury, Tissue factor (Thromboplasin) converts VII to VIIa
- VIIa converts X to Xa and joins the common pathway
- Common
- X is converted to Xa via agents from either the intrinsic and/or extrinsic pathways
- Xa, catalyzed by V and Ca2+ converts Prothrombin (II) to Thrombin (IIa)
- Thrombin (IIa) converts soluble fibrinogen (I) to insoluble fibrinogen (Ia)
- Catalyzed by XIII, insoluble fibrinogen is converted to X-linked fibrin
What is the importance of Von Willebrand factor for coagulation?
The platelet surface receptor must come into contact with Von Willebrand factor on the subendothelium to help overcome the force of blood flow.
What is the importance of Vitamin K in the clotting cascade?
Factors II, VII, IX, and X of the clotting cascade are Vitamin K-depdendent
What are the ways to evaluate the coagulative haemostasis in an animal?
- Primary haemostasis
- Platelet count
- Measurement of vEf function
- Buccal mucosal bleeding time (BMBT)
- Secondary haemostasis
- Prothombin time (PT)
- Activated partial thromboplastin time (APTT)
- Factors must be decreased to 30% of normal before apTT is prolongued
- Tertiary haemostasis
- D-dimers
- D-dimer (or D dimer) is a fibrin degradation product (or FDP), a small protein fragment present in the blood after a blood clot is degraded by fibrinolysis. It is so named because it contains two crosslinked Dfragments of the fibrin protein.
- fibrinogen levels and Thrombin clot time
- D-dimers
What are the predisposing factors for thrombosis?
- Virchow’s Triad
- Endothelial injury
- Caused by viruses, parasites, Immune-mediated vasculitis, disseminated intravascular coagulation, local extension of infection
- Abnormal (turbulent) blood flow
- Hypercoagulation
- Endothelial injury
Descrube the diorders of tertiary hameostasis.
- Mostly associated with DIC which causes widespread activation of haemostasis (prothrombotic state), which, in turn, uses up all the clotting factors and results in increased tendency to bleed
- Inflammation may result in increased fibronogen levels (acute phase protein)
What causes anaphylactic shock?
- Organism is exposed and sensitized to a particular antigen and shock is associated with subsequent release of histamine
- Causes vasodilation, leaky dilated blood vessels, drop in blood pressure and reduced perfusion
What causes septic shock?
- Most common form of maldistributive shock
- Mediated by vascular and inflammatory mediators in response to bacterial or fungal infection
- Causes vasodilation
- Trigger is LPS (endotoxin) in Gram Negative Bacteria which stimulates Factor XII and causes coagulation at high dose
- At low dose, activates macrophages, endothelial cells, and complement
- At moderate dose, raises TNF and IL-1, causing fever
Describe the progressive stages of shock.
- Compensated
- Increased cardiac output and vasoconstriction to maintain blood pressure and tissue oxygenation via stimulation of the sympathetic nervous system so that vital organs are protected
- Control of water balance by decreasing GFR, through the use of the RAS, and release of ADH
- Progressive
- Compensatory mechanisms cannot cope with prolongued or severe drop in blood volume leading to hypoperfusion and cell injury
- Tissues do not receive enough oxygen so cell metabolism shifts to anaerobic respiration (decrease in ATP production) and production of lactic acid leading to cell damage (from lysosomal enzyme release) and necrosis
- Irreversible
- Mechanisms aimed at vasoconstriction are overwhelmed
- Leads to widespread vasodilation and organ failure
What proportion of the bodyweight is blood volume?
~7%
Discuss the aetiology of Feline Infectious Peritonitis Virus (FIPV)
- Coronavirus
- Causes feline peritonitis
- Virus lives in macrophage
- Pathology is the result of phlebitis (inflammation of the veins)
- Results from deposition of immune complexes and activation of complement
- Macrophages release proinflammatory cytokines with promote leakage of blood vessels
Discuss Myobaterium Bovis.
- Cattle tuberculosis
- Causes disease in cattle and other animals
- Spread by coughing and sneezing
- Bacteria survive in macrophages in a granuloma in the respiratory tract
- Zoonotic
- Pathology
- Grossly: circumscribed, often encapsulated, pale yellow to while focus, often with caseous necrosis or mineralization
- Respiratory tract lymph nodes are affected most often
- Can cause lesions in the lungs
- Can cause systemic disease
- Histologically
- Cental area of caseous necrosis
- Mantle of macrophages and multinucleated giant cells
- Rim of lymphocytes and fibroblasts
- Acid-fast bacteria within the macrophages and giant cells
- Causes subtle lesions in badger lungs
Disucss M.a. Paratuberculosis.
- Johne’s disease
- Affects cattle, sheep, goats and deer
- Animals infected when young and causes diarrhoea and weight loss when older
- Gross lesions
- Thickened and corrugated small intestine
- Terminal ileum is most often affected
- Swollen lymphatics
- Granulomatous inflammation with sheets of macrophages upon histological examination
- Histologically (in sheep) types:
- Mutibacillary
- Macrophages and giant cells apparent
- Intracellular acid-fast bacteria apparent
- Paucibacillary
- Lymphocytes and plasma cells apparent
- Some macrophages apparent
- Very few acid-fast bacteria apparent
- Rare in cattle
- Mutibacillary
What feature of mycobacteria cause granulomatous disease?
Mycobacteria can cause granulomas because their intracellular survival is aided by their specialized cell wall which halts the fusion of the lysosome to the phagosome.
Describe granulomatous inflammation.
Chronic inflammation characterized by an abundance of macrophages
What is desmoplasia?
Growth of fibrous or connective tissue
Describe the cytological features of malignancy.
- Hypercellularity
- Presence of excess cells
- Multinucleated cells
- Large or multiple nucleoli
- Increased nuclear to cytoplasmic ratio
- Anisocytosis (variation in cell size)
- Ansiokaryosis (variation in nuclear size)
- Pleomorphism (variation in cell shape)
- Increased mitotic activity and/or abnormal mitoses
What is Post-mortem blood hypostasis?
If an animal has been lying on one side after death, asymmetric congestion will result
What is tissue autolysis?
- Tissue self-digestion due to release of intracellular enzymes
- Can resemble necrosis
- Histologically loses the definition of cells and supporting tissue
- Tissue tends to be darker and friable
- Occurs at different rates in different tissues
What is anthracosis?
- Lungs may contain fine 1-2mm black foci in subpleural region
- Medulla of regional lymph nodes may be black
How should suspected toxicology (suspected poisoned animal) samples be stored and transported?
Samples to be sent for toxicology should be frozen
How would a sample be prepared to investigate the presence of a pathogen?
Swab into transport medium
What are the clinical features of shock?
- Hypotension
- Weak pulse and tachycardia
- Hyperventilation
- Decreased urine production
- Peripheral vasoconstriction (during compensatory phase)
What is pleomorphism?
Variability in the size, shape and staining of cells and/or their nuclei
What is antiosocytosis?
The presence of red blood cells of different sizes
What is macrocytosis?
Insufficient and unusually large red blood cells
What are some common histological features of a malignant neoplasm?
- Pleomorphism
- variability in the size, shape and staining of cells and/or their nuclei.
- Antisocytosis
- Red blood cells are of different sizes
- Macrocytosis
- Insufficient and unusually large red blood cells
- Hypercellularity
- Abnormal excess of cells
- Disordered alignment (formation of 3D structure, for example)
- Basophilia
- Vacuoles
- Phagocytosis of tumor cells or of other cells by tumour cells
- Ansio/macrokaryosis
- Increased nucleus to cytoplasm ratio
- Mitoses
- Atypical mitosis
- Division in three parts
- Single chromosomes
- Incorrect alignment of chromosomes
- Multinucleation
- Nuclear moulding
- Deformation of nuclei by other nuclei within the same cell or adjacent
- Atypical chromatin pattern
- Cord-like, coarse, clumps, fragments, nuclear wall hyperchromasia, variation in chromatin content
- Abnormal nucleoli
What is poikilocytosis?
Variation in the shape of red blood cells
What is haemoconcentration? What can it indicate?
- Increased red blood cell concentration
- Indicative of: Fitness, dehydration, hypoxia, some tumours, unique genetics (seen in sighthounds which tend to have higher values)
Describe the situations in which there can be a low red blood cell count.
- Regenerative
- Haemolytic
- Haemorrhagic
- Non-regenerative
- Pre-regenerative
- Anaemia of inflammatory disease
- Chronic renal disease
- Iron deficiency anaemia
- Bone marrow disease- lack of erythropoeitin production
What condition is indicated by neutrophilia and lymphocytosis?
Physiological
What is indicated with the white blood cell desmonstrating: neutrophilia, monocytosis, lymphopenia, eosinopenia
Stress
What is the following indicative of: Neutrophilia (+/- left shift), monocytosis, +/- lymphocytosis
Inflammation
What is the following indicative of: Severe neutrophilia
Extreme neutrophilic leukocytosis
How is hypovolaemia corrected in the body?
- Decreased renal perfusion (causing low sodium levels) detected by macula densa cells in the juxtaglomerular apparatus causes renin release
- Renin causes the conversion of angiotensinogen to Angiotensin I in the liver
- Angiotensin I is converted to angiontensin II by angiotensin-converting enzyme (ACE) in the lungs
- Angiotensin II causes the release of aldosterone from the adrenal cortex
- Aldosterone upregulates sodium channels and sodium-potassium ATPase in principle cells in the late distal convoluted tubule causing sodium reabsorption and water
Sodium is recovered from the late distal tubule and the collecting ducts
How is hypervolaemia (hypoosmolar state) detected in the body?
- Recognized by osmoreceptors in hypothalamus which suppress secretion of ADH and cause loss of water in kidney
- Baroreceptors in left atrium detect high blood volume and blood pressure which inhibit ADH production
- The resulting greater urine production reduced blood pressure
What is epistaxis?
Bleeding from the nose
What is haemoptysis?
Coughing up of blood
What is haematochezia?
Haemorrhagic faeces
What three conditions are seen in Feline Eosinophilic Granuloma Complex?
- Feline eosinophilic granuloma
- More common in young cats
- Forms nodular or linear lesions on skin, footpad, musculocutaneous junctions and oral cavity that are raised, pink, and alopecic
- Histologically: eosinophils and macrophages found
- Eosinophilic plaque
- Forms raised, red, alopecic to ulcerated, flat-topped plaques on the skin
- Very pruritic
- Histologically, eosinophils, lymphocytes, and macrophages found
- Indolent ulcer
- Forms ulcerated lesion on upper lip, adjacent to philtrum
- Pain and pruritis are rare
- Can be unilateral or bilateral
- Histologically, eosinophils, neutrophils, mast cells, and macrophages are found
Describe the biological behaviour of a benign tumour.
- Expansile, capsular growth
- Slow growth rate
- Well differentiated
- No metastasis
- Becomes a space-occupying lesion (SOL)
Describe the behaviour of a malignant tumour.
- Invasive with no capsule
- Wide range of growth rates
- Wide range of differentiation
- Can metastasise
- Often causes life-threatening circumstances for the host
What is a papilloma?
Benign surface tumour
What is this? When is it likely to be formed?

Keratin pearl likely to form in squamous cell carcinoma
What is ansiokaryosis?
Variation in nuclear size
What is pictured here?

Blood cells and platelets
What is pictured here?
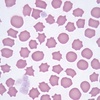
Echidnocytes
What is pictured here? What causes this conditon?

Howell-Jolly body: histopathological findings of basophilic nuclear remnants (clusters of DNA) in circulating erythrocyte
What is pictured here?
Schistocyte


