ID CM Flashcards
definition of epidemiology
study of distribution of disease and the distribution of determinants (RF, exposures) of disease (or health related states) in disease specific populations
what are the 3 goals of epidemiology?
describe patterns
identify causes of disease
provide data for the management, evaluation and planning of services
what are the 5 goals of surveillance?
detect outbreaks
quantify magnitude of the problem
evaluate prevention measures
detect changes in the health care practice
facilitate planning
what are the 5 categories of reportable conditions?
STDs
gastrointestinal (cholera)
biologic threat agents
Vector Borne
zoonotic
what are there reportable disease
category 1
category 2
Category 1: immediate notification
Category 2: Notification within 48 hours
how long can it take for H1N1 to become a pandemic?
48 hours
she wrote this down
what are the 4 goals of influenza surveillance?
what is this accomplished by?
identify circulating strains
assist in controlling outbreaks
provide information to policy makers
build rapid response
accomplished by syndromic surveillance
who is exempt from HIPPA privacy rule?
public health investigators
they have the right to acess the information on reportable disease
if someone has a reportable condition…what is provided to the public health official?
(4)
condition diagnosed or suspected
unusual or sudden increase
Name, date, phone number
who are specifically vulnerable to disease?
elderly living alone
those with chronic diseases
what number in the country are we for elderly living at home?
why do we care?
3rd!
especially living at home is an issue if there is a flu outbreak or also a heat wave!! think about this!!
what number are we in the country of peope living outside of an urban area?
2nd for % living outside of urban area!
need to consider this if there was epidemic or anything because they would be more vulnerable and have less access to care!
does the federal authority have the right to quarentine or isolate someone?
who is responsible for public health?
yes, federal authority has the right to quarentine someone TO PROTECT THE PUBLICAND IF EMERENCY HEALTH RISK
**states are responsible for public health within their own borders**
what are 4 RECENT conditions that the federal authority can DETAIN somoene for having?
XDR-TB: air traffic
Bushmeat: possible ebola
measles: europe
H1N1 pandemic (young people)
who did H1N1 pandemic effect?
young healthy people
what are 7 isolateable diseases?
cholera
diphtheria
plague
TB
smallpox
yellow fever
hemorrhagic fever
what is it always important to do in a patient presenting with a illness
ask about travel hx!!
what is important to remeber when doffing PPE?
important to remove most contaminated PPE first to prevent self-contamination
have they started vaccination trials for ebola?
YES!
explain the source of peoples confusion surrounding vaccine and autism?
MEASLES MUMPS REBULA VACCINE IN LANCET PUBLISHED IT CAUSED AUTISM,
12 YEARS LATER IN 2010 THE ARTICLE AS REMOVED AND REATRACTED. THE ONLY TIME THAT THE JOURNAL MOVED ARTICLE BECAUSE ITS A PRETIGIOUS JOURNAL
THE RESERACHER FALSIFIED DATA AND LOST OFF OF HIS FUNDING, MULTIPLE STUDIES SINCE SHOWING NO RELATIONSHIP!!!
how many americans get ill with food borne illness?
1 in 4 Americans ill
what are 3 long term sequelae of food born illness and what are they caused by?
1. Hemolytic uremic syndrome (HUS)
E. coli
long term kidney dysfunction in 33%
2. Guillain Barre Syndrome (GBS)
campylobacter jejuni
40% ventilated
85% with residual deficits
3. Reactive arthropathy
salmonella, campylobacter, yersinia, enterocolitia, shigella
what is the 1 foodborne illness that has increased in influnence for infection?
vibrio
how much has ecoli food born illness decreased over the last 4 years?
25%
what are the 7 most influential food born illnesses?
- listeria
- E. coli
- toxoplasmosis
- salmonella
- campylobacter
- norovirus
- vibro (increasing in prevalance)
vibrio
2 things that cause this?
what does it come from?
what is the control strategy?
v. parahaemolyticus, v. vulnificus
underling liver disease, immunocomprimised
WARM WATERS, RAW SHELLFISH
Control strategy: educate the consumer
focal outbreak
what is this characterized by?
who detects it?
what happens?
likely cause?
is there a fix?
- large number of cases in one jurisdiction
- detected by the infected group themselves
- local investigation
- local food handling error
- local solution
dispersed outbreak
where does this occur?
who detects it?
who investigates?
likely cause?
implications?
- small number in many jurisdictions
- detected by lab-based subtype surveillance
- multi-state investigation
- industrial contamination event
- broad implications
why do we see more dispersed outbreaks?
- better surveillance
- centralized production of foods means when there is a problem it occurs everywhere
- more imported foods/ingredients
4.
when you think of ground beef
what bacteria should you think of? (2)
shigella producing E. coli
MDR salmonella
sprouts
why are these bad?
what is it difficult to prevent?
what are two intitiates put in place?
REALLY BAD DIRTY THING!!
grow in warm moist environment that harbors bacteria
Why difficult to prevent:
- difficult to detect the bacteria once in the plant
- rarely cooked by consumer
- scarification, bacteria enters the seed so hard to find
Prevention:
- NACMCF spout guidance white paper!
- sprout guidance by the FDA
what are the two common pathogens that infect sprouts?
E.coli
salmonella
what are the steps to following an outbreak?
(4)
determine whether there is an outbreak
describe the outbreak
measure the outbreak
stop further outbreaks
case definition
what is this?
in epidemiology it is:
what is is required to be included in the outbreak and be considered positive
what is descriptive epidemiology?
the summary of health-related characteristics according to the person place and time, tells you “who, what, when, where, why”
used to determine the cause of the outbreak
yellow fever vaccine
where geographic locations do you need this?
can it be required?
living/dead?
central/south america and Africa
*1 of 2 required vaccines for travel*
required every 10 years to travel to infect areas with endemic levels
attenuated live vaccine
1 vaccine last 10 years
what are the two vaccines that are the only two LEGALLY required for international travel?
- yellow fever
- cholera
is there polio in the americas?
NOPE! americas are polio free now!
cholera vaccine
are travelers at high risk?
helpful vaccine?
how many shots?
booster?
what is there no vaccine to?
most travelers low risk
vaccine of limited use now
no vaccine to vibrio cholera 0139 strain
full 3 shot series
booster in 6 months might be needed
what should you know about the parentral cholera vaccine?
poorly protective in 50% for only a few months
uncomfortable and rarely reccomended
what are some vaccines that may be indicated depending where you are traveling to?
(8 of them)
- typhoid
- plaque
- measles
- polio
- rabies
- Hep A
- Hep B
- Tetnus
measles vaccine
MMR
live/dead?
of doses?
LIVE
two doses
polio vaccine
options for admin?
what 3 geographic locations?
single booster needed for india, pakistan, afghanistan
inactivated: parentral (18+ never vaccinated)
attenuated live oral
where is the only known transmission for polio?
pakistan and afghanistan
rabies vaccine
who gets it?
of doses?
people who are staying in a endemic region or remote area with close animal contact
4 vaccine doses
Hep A vaccine
who should get this?
who are there new reccomendations for?
when should first dose be given?
when do they get booster?
nearly all international travelers
new pediatric recommendations
first dose >4 weeks prior
booster: 6-12/18 months
hepatitis B vaccine
who should get this?
how many series?
endemic in South America, Africa, SE Asia, South Pacific
close contact with locals
extended stay
0, 1, 6 month series
Tetnus
who should get this?
when is the booster indicated?
what is the nickname for this?
what age group qualifies?
EVERYONE SHOULD HAVE A PRIMARY SERIES
TETNUS-DIPHTHERIA TOXOID BOOSTER IS INDICATED every 10 years
greater than 5 years old
“Tdap”
when are the time frames for influenza in the different hemispheres?
November to March northern hemisphere
april to september in southern hemisphere
what are four unavaliable or uncommon vaccines?
if uncommon, where are they used?
small pox: ex: millitary
typhus-off the market
anthrax-CDC
BCG-_overseas_ use
what are 4 important hygiene considerations when traveling abroad?
(what to avoid as well)
1. water acquisition…bottled!
2. other beverages
3. food precautions
a. only well cooked meat
b. AVOID
- salad/raw veggies
- unpasteurized dairy products
- street vendors
- ice
4. restaurant evaluation
travels diareahh
what does this come from?
who is it common in?
what is the 4 most common causes?
what is the most common?
what are 3 symptoms?
what are 4 tx considerations?
fecally contaminated water and food
more common in younger people
MOST COMON BACTERIA, then parasites
MOST COMMON: E.coli, shigella/salmonella, campylobacter, viral
symptoms:
- abrupt onset of loose stools
- abdominal cramping
- rectal urgency
tx:
- typically self limited
- REHYDRATION
-
fluoroquinolones, short 3 day course
- rifaximin
- azithromycin - immodium
is prophylaxsis reccomended for travelers diarreah?
nope it is not…
but you can consider prophylaxsis in special situations with
fluorquinolones/refaxamin
what are 5 preventative measures you can take to prevent travelers diarreah?
- avoid street vendors
- buffets
- raw or undercooked meats/seafoods
- avoid raw fruits, vegetables
- avoid tap water, ice and dairy products
what type of mosquitos bite humans?
explain the life cycle?
what do they need for their life cycle?
what do you find larvae?
only the female take blood meals
eggs to larvae to pupae to adult
mosquitos need to be in WATER for most of their lifecycle
mosquito larvae are found in stanidng water
what are some ways you can prevent arboviral illnesses?
5 ways
- repellants like DEET, oil of lemon
- protective premetherin treated clothing
- limit outdoor activity in high-risk area
- screens on windowns and doors
- use bed nets
what are the two arboviruses that maine is most concerned with?
eastern equine encephalitis
west nile virus
explain how they test for rabies on the specimen you bring in?
euthanasia and decapitation
cold (not frozen shipment)
harvest braine and prepare slides
cerebellum, hippocampus, and brain step
fluorescent antibody staining
monoclonal typing of positive specimens
what are the 4 conditions transmitted by the ixodes scapularis (deer tick)?
- borrelia burdoferi: aka LYME DISEASE
2. babesia microti: HUMAN BABESIOSIS
3. anaplasma phagocytophilia: human granulocytic anaplasmosis
4. powassan virus
lyme disease is caused by
borrelia burdoferi
human babesiosis is caused by
babesia microti
human granulocytic anaplasmosis aka human anaplasmosis is caused by
anaplasma phagocytophilia
what is the scientific name for deer tick?
ioxodes scapularis
what are the most common sxs seen with tickborne disease?
(3)
- fever/chills
- myalgias/pains
- rash
what is the stage of ioxodes scapularis tick that bites humans to cause lyme?
THE NYMPH!!!!!!
not the adult!!…these prefer white tailed deer!!!
what is STARI? what is it transmitted by?
southern tick associated rash illness (STARI)
cause unknown
rash appeares like lyme disease
transmitted by lone star tick
what are relapsing fevers characterized by?
group of acute infections caused by arthropod born spirochetes of the genus BORRELIA
characterized by reccurent cycles of febrile episodes, separated by asymptomatic intervals of apparent recovery
what are the 3 types of body lice?
1. head lice: pediculous humanus capitus
2. body lice: pediculus humanus humanus
3. pubic lice: phthirus pubis
of the 3 types of body lice, which does spread disease and which ones do not?
body lice: SPREAD BACTERIAL DISEASE
head and public lice do NOT spread disease
borrelia reccurentis
what does this cause?
what causes this in africa?
what is this characterized by?
how often can it occur?
3 tx options?
louse born relapsing fever
Borrelia croicudare causes replapsing fever in africa
***portal of entry when infected lice are crushed into abraded skin***
gets into the skin from lice being crushed into abraded skin
CLEARING OF CICULATING STRAIN BORRELIA IN 3-5 days then NEW ANTIGENIC VARIANTS APPEARE
*** up to 3-5 relapses may occur***
TX:
penicillin
tetracycline
erythromycin
how do people get bitten by a tick?
ticks don’t fly or jump!!!
they grab onto persons clothes as they walk by and crawl to a feeding spot on the person’s skin
where are some specific places you should look for hiding ticks on your body?
8 places
- head
- hairline
- nape of the neck
- armpits
- waist
- between legs
- thighs
- behind knees
***basically everywhere**
what is the best way to remove a tick?
- promptly
- with tweezers
- pull gently and slowly till tick lets go
- apply antiseptic to bite
Do not be alarmed if the tick’s mouthparts remain in the skin. Once the mouthparts are removed from the rest of the tick, it can no longer transmit the Lyme disease bacteria.
potentially a Dr. Sears mythbuster!
what are the requirements for HIV test in maine?
(3)
- A patient must be informed that an HIV test will be performed
- Information must include an explanation of what an HIV infection involves
- If a test is positive, post-test counseling must be provided
what are the two reccomendations for pregnant women with regards to HIV?
2
- testing included in routine panel of prenatal screening in ALL pregnant women
- repeat screen in 3rd trimester in areas with elevated HIV among pregnant women
who is screen reccomended in for HIV/AIDS? (3)
what is not required?
what must be obtained to test?
- routine screening in all health care settings for all patients 13-64
(annual tests for at risk populations)
- tests all pts with signs and sxs or with opportunist infection associated with AIDS
- prevention cousleing and written consent forms are not required
- testing must be voluntary with verbal consent informaed
what is the risk of HIV with needle stick?
what about risk after expsure from eye, nose, mouth to HIV infected blood?
.3% with needle stick
.09% from eye, nose, mouth to HIV infected blood
why is there resistance to HIV drugs?
(3)
- High replication rate
- High mutation rate
- Selective pressure of drugs favors mutant strains over wild type
what can be a down side of using antivirals to tx HIV?
when does this ocurr?
how long does it last?
sxs?
reconstitution syndromes
Inflammatory reactions that occur after initiation of effective antiretroviral therapy
Usually occur few weeks to several months after initiation of therapy
Usually self-limited, but manifestations may be severe
is a condition seen in some cases of AIDS orimmunosuppression, in which the immune system begins to recover, but then responds to a previously acquired opportunistic infection with an overwhelming inflammatoryresponse that paradoxically makes the symptoms of infection worse.[2]
what must you continue to monitor for when txing a patient with HIV?
(4)
- new STDs annually
- new onset Hep C annually
- TB
- metabolic disorders
what vaccines are particullary important to make sure HIV pt has?
(5)
Annual influenza
pneumococcal
tetanus
hepatitis A and B
what is the structure of influenza? what family? what types?
- single stranded RNA
- orthomyxovirdae family
- A, B, C types
what is the composition of influenza A? of these two, how many are there in humans?
hemagglutinin (HA)
neuramidase (NA)
3 HA types in humans
2 NA types in humans
what does drift and shift mean in terms of influenza?
shift: pandemics, have NEW HA or NA
drift: epidemics, development of new strains, but not whole new component

what are 3 challenges of containment of influenza?
- short incubation time (1-7 days)
- ability for person with asymptomatic infection to transmit virus (can be contagious 1 day before symptoms)
- early symptoms of illness are likely to be non-specific, delaying recognition (need to get antivirals on board within 48 hours of onset)
Avian flu (H5N1)
who does this infect? how was this introduced into N. america? why are we so scared of this?
- usually only infects birds
- effects younger patients
- longer duration of infection
- introduced to N. america by bird migration, infected people migrating, transportation of infcted poultry
***hasn’t transferred from person to person but if it does, we will basically all die because no one has immunity and 1918 will happen all over again, working on vaccines now but super scary, race agains time***
influenza
what are the three types and which one is most pathogenic? what is the season for this disease, how is it spread and how long can it survive on a surface? how long does it incubate? how long do symptoms last? when is a person contagious? when is peak shedding and what does it correlate with? what is the definition? what is the best choice for diagnosis?
3 types; A (most pathogenic), B, C; neuramidase and hemmaglutinin make up the subtypes
Fall/winter outbreaks (october-november)
spread through aerosolized droplets, can live on surfaces 2-8 hours
- incubates 1-7 days, avg 3
- symptoms last 3-7 days, but up to 14
3. contagious 1 day before symptoms, 5-7 days after
4. peak shedding 3 days of illness, correlates with fever
fever >100 or 37.8C AND cough or sore throat in absence of know cause, ABRUPT onset, can have myalgia in legs and lumbosacral area. Emergency if CNS symptoms.
PCR is best choice for diagnosis, can do rapid from throat or nose, but not as good
what is the best way to prevent influenza?
what are the two mechanisms of this? which age groups should be considereded for these two methods? what form is the virus in? which patients should you NOT use this in???
IMMUNIZATION!!
- inactive intradermal vaccine: innactive, trivalent, quadrivalent, recombinant, higher antigen, contains 3-4 viruses, 70-90% effective everyone older than 6 months
2. intranasal: live attentuated, 2-49 year old, caution in >50 or pregnant
***don’t use if allergic to eggs or gelatin***
what are the treatment options for influenza?
how are they used?
when do they need to be started?
who don’t you use these in?
neuriamidase inhibitors
- oseltamivir
- zanamirvir
used for treatment and prophylaxis
need to be started within 48 hours
don’t use in
what do you worry about when a child has influenza and are given asprin? what is the fatality rate?
REYE SYNDROME
(fatty liver and encephalopathy)
happens when pt has viral infection and given asprin, occurs 2-3 weeks after with a 30% fatality rate
what do you worry about as a complication in elderly and chronically ill who have influenza? (2 things)
- necrosis of the respiratory epithelium that leads to secondary bacterial infection by staph, strep, or haemoph
- pneumonia development, significantly contributes to fatality
How many people are infected with TB? how many of those go on to develope the disease?
2 billion people are infected
9 million people develop the disease
Infected does not mean you will develop the disease!! Two completely different things!!!
what bacteria cause the most TB in the US? what are 4 other bacteria that can cause it?
mycobacterium tuberculosis
mycobacterium bovis
mycobacterium africanum
mycobacterium microti
mycobacterium canetti
what are the two populations of people that TB can be divided by?
hight risk for becoming INFECTED with TB
high risk for DEVELOPING TB DISEASE
what are 7 things that can put someone at high risk for TB INFECTION (not disease)
- close contact
- foreign born
- low income and homeless
- health care workers in high risk groups
- racial and ethnic minorities
- infants, children and adolescents
- IV drug users
name five areas of the world where TB is common?
- asia
- africa
- russia
- eastern europe
- latin america
what groups of people are at risk for developing TB disease!? (7)
- people with HIV (thats why prevalence increased in the 80s)
- infection of TB within last two years (5% risk, and 10% lifetime)
- infants and children
4. prolonged therapy with corticosteroids
- IV drug use
- diabetes
- silicosis
what is the greatest risk factor for devloping TB?
HIV!!! 7-10% risk for devloping TB disease each year when infected with both TB and HIV
are people with LTBI infectious? what percent of these people will go on to develope the disease?
no they aren’t infectious!!
10% will go on to develope disease!
Explain the pathogenisis steps for TB (5 steps)
- tubercle bacilli are inhaled and travel to alveoli
- multiple in alveoli, infection begins
- small number of tubercle bacilli enter bloodstream and spread throughout body
- within 2-4 weeks macrophages survive bacilli, form a barrier shell that keeps the bacilli contained and under control know as LBTI
- if the immune system can’t keep tubercle bacilli under control, they multiple rapidly and cause TB DISEASE *it can occur in other places in the body too*
In TB, explain the differences between LTBI and TB disease in these characteristic:
- active/inactive bacilli
- chest xray findings
- sputum smears
- symptoms
- infectivity
- a case of TB or not

Is LTBI treated with medication?
YES IT IS
you want to prevent these patients from getting it in the future!!!
who is high priority treatment for LTBI with a TST >5 mm or postitive IGRA? (5 things)
- close contacts of those with infectious TB disease
- HIV
- chest xrays indicating previous TB
- organ donor transplants
- immunocomprimised patients
who is high priority for LTBI treatment >10 mm or positive IGRA test? (5 things)
- people who came to US within last 5 years where TB is common
- IV drug users
- live or work in high risk facilities
- micro labatories
- children
what are the two ways HIV can influence the path of TB?
- person with LTBI becomes infected with HIV and then developes TB disease as the immune system is weakened
- a person with HIV becomes infected with TB and rapidly developes the disease
what is primary resistance?
cause by person to person transmission of drug resistant organisms
secondary resistance
develops during TB treatment
- patients were not given appropriate treatment regimen
- patients didn’t follow the medication as it was prescribed
multi-drug resistant TB is resistant to which drugs?
isoniazid and rifampin (2 first line drugs avaliable)
extensively drug resistant (XDR-TB), what drugs are they resistant to?
isoniazid and rifampin, PLUS fluoroquinolones and at least 1 of the 3 second line drugs
**this is a major issue around the world**
how long should a patient be treated for TB?
what if this person has pos sputum after 2 months of treatment?
at least 6 months
if cavities on chest xray and postitive sputum cultures at 2 motnhs then treatment should be extended for 9 months
what are the three phases of TB infection treatment?
1.initial phase: first 8 weeks of treatment, four drugs are used
isoniazid, rifampin, pyrazinamide, ethambutol
2. continuation phase: after first 8 weeks of treatment, bacilli remaining after initial phase are treated with at least two drugs
3. relapse phase: occurs when treatment is not continued for long enough, surviving bacilli may cause TB disease at a later time
in order to prevent drug resistance, TB disease must be treated with at least how many drugs?
2 ones the organism is suseptible to
Tuberculosis
what are the classic symptoms assosicated with TB (clinical and xray)?
clinical symptoms:
coughing >3 weeks
pleuritic chest pain
hemoptysis
positive rales
infiltrates (collection of fluid and cells in lung tissues)
cavities (hollow spaces within lung usually in the upper lobe)
caseating granuloms on biopsy (necrotizing granulomas)
what tests do you use to diagnose TB?
- tuberculin skin test (TST)
2. interferon gamma assays (IGRAS)-measures immune response to m. tuberculosis, less likely to be incorrect compared to TST
3. culture with AFB staining
-need 3 specimens, 8-24 hour collection intervals, can induce with inhaling saline mist spray
4. chest x-ray (infiltrates and cavities)
5. nucleic acid amplification test
6. bronchoscopy or gastric wash if having hard time getting sample
explain the tuberculin skin test? what can’t this test do? what are positive test results for the three groups of people?
in lastent infection positive 2-4 weeks after infection
-injected with inactive tubercle bacilli, read within 48-72 hours
**this test can’t differentiate between latent and active TB, just that a person has been infected at some point**
Positive test results:
15 mm in normal patients
10 mm in immigrants, children
5 mm in HIV, immunsuppressed, positive chest xray, primary TB exposure
explain the difference on chest xray between primary and reactivated TB?
primary: homogeous infiltrates, hilar/paratracheal lymph node englargement, middle/lower lobe consolidation
reactivation: fibrocavity apical disease, nodules, infiltrates **TB reactivation presents at the top of the lungs instead of wher eit happened originally**
what should you connect Ghon complexes and Ranke complexes? what are they?
TB
ghon complexes: calcified primary focus
ranke complexes: calcified primary focus and hilar lymph nodes
**these represent healed primary infection**

what does milliary TB look like?
millet seed like nodule lesions (2-4 mm)
what is the gold standard for TB testing?
acid fast bacilli tests
3 negative tests are considered negative!!
how long should a person be isolated and on treatment before being allowed in public when they have TB?
need to be isolated for a minimum of 2 weeks
what are the four drugs you use during the initial treatment phase for TB? what are their side effects? how do you treat someone if they have been exposed to someone with active TB? what is the treatment regiment for LBTI?
“RIPE acronym
- rifampin (hepatitis, flu, orange body secretions)
- isoniazid (hepatitis, periphreal neuropathy, give B6 to prevent risk)
- Pyrazinamide
- ethambutol (optic neuritis)
**for LBTI: treat with isoniazid and pyrazinamide for 9 months, or 12 months if HIV pos or granulomas present on CXR**
**if someone is exposed to patient with active TB, then treat them emipircally for 12 weeks until negative TB can be obtained**
what are the three main classifications of candidal infections based on location?
- cutaneous (diaper dermatitis and candidal intertrigo)
2. mucosal candida of the mouth and pharynx
3. vulvovaginal
what is the most common species of candida?
candida albicans
Cutaneous candidal infection
- candidal intertrigo
- diaper dermatitis
what is the characterists of these? where are the places you would find these? what are the two TX options?

patches and pustules on a ERYTHEM MATOUS BASE beefy red the erode and confluent with “SATELITE LESIONS“ painful with puritis
Candidal intertrigo: axillae, groin, intergluteal, cleft
diaper dermatitis: irrritabiltiy with urination, defication, changing diapers, genital region, inner aspect of thights and butt
TX: keep dry, antifungals nystatin, imidazole powder
oropharyngeal candidiasis
what does this look like and what in what population can this look completely different? what is the key characteristic of this? what are the 2 treatment options?

thrush, white curd like plaques that can be scraped off
what to find the percipitating cause and treat that, then treat with oral antifungals
*****KEEP IN MIND, PEOPLE IN DENTURES CAN APPEARE BIRGHT RED INSTEAD OF WHITE CURD LIKE****
Tx: nystatin oral fluconazole or itraconazole suspension, swish and spit or swallow
vulvovaginal candidiasis
what percent of females can get this and what can it come from? what are 5 RF for this? what does it look like and what is an important symptoms? what are two treatment options?
75% of females get this at least once, >20% are colonized with C.albicans normally, so this is a overgrowth of normal biota
RF: age extremes, pregnancy, DM, corticosteroids, HIV
white cottage cheese like discharge/plaques, burning while peeing, and puritis
TX: topical/intravaginal azoles or oral fluconazole
what can vulvovaginal candidiasis be closely related to?
some women just get it right befor their period because of the pH change that allows microbiota to grow better
balanitis candidiasis
who is this common in? who must you treat? treatment?
common in uncircumsized men
erosions with white plaques under foreskin
treat sexual partner
TX: topical nystatin, warm soaks to alievate itching/burning
what are 6 RF for candidiasis?
- diabetes
- pregancy
- obesity
- HIV/AIDS
- moisture
- IUD
what do you use to diagnose candidiasis? what do you see?
KOH
***see pseudohyphae and budding yeast***
varicella-zoster virus

explain the differences seen between the primary and secondary eroptios of this virus? how are they descirbed? what sign do you watch out for? what is the order of the lesion developement? where does it begin and where does it spread to?
VARICELLA-ZOSTER virus
varicella (chicken pox): 1st exsposure vesicles on a erythematous base “DEW DROPS ON A ROSE PETAL” describe the different stages
macules->papules->vesicles “dew drops on a rose petal”->pustules->crusts **appeare in crops!**
BEGIN ON FACE AND TRUNK AND SPREADS TO EXTREMITIES
Herpes zoster (shingles): VZV reactivation along a Dermatone in THORACIC OR LUMBAR REGIONS, reactivation from ganglionic satelite cells!
-Hutchinson’s sign:lesions on the nose mean lesions in the eye sincetrigeminal nerve involvement CN #5

what are the two complications you worry about with herpes zoster virus reactivation (shingles)?

- eye involement herpes zoster opthalmicus: look for hutchinson’s sign which is lesions at the end of the nose, if seen here likely it is already in the eye since it follows along the trigeminal nerve or CN 5
- ear involvement herpes zoster oticus: look for ramsay hunt syndrome if lesions are seen on the ear, likely in the canal since it follows facial nerve or CN 7

how long can the post herpetic neuraligia with shingles last? what is a thing you worry about if eldery?
>3 months…so give these people some pain meds
occurence likelyhood is greater if over 60!
what is the treatment options for varicella zoster virus? (4)
- acyclovir, valacyclovir
- pain management for post therapeutic neuralgia
- tricyclate antidepressants
- corticosteroids
what can you do to prevent varicella-zoster virus? (2 options)
VACCINATION!!
child: vaccinated 1-2 years old for varicella
adult: Zostavax single dose >60yrs…basically literally a booster of varicella, becuase it is the same virus, just marketed differently to apeal to elder adults!
**can’t give if allergic to gellatin, neomycin, pregnant, or immunocomprimised!**
acute rheumatic fever/RHEUMATIC VALVITIS
what fraction occur in developign countries? what organism is this caused by? what does this attack and cause? what is the main tx? (what about for other two symptoms?)
2/3 of all cases in developing countries
group A streptococcus that cause oropharyngreal infection, the antigens to this attack the heart
PERICARDITIS INVOLVING THE VALVES, CAUSING FIBROUS THICKENING/STENOSIS AND REGURG
Dx:
Jones criteria two major, 1 minor
plus evidence of B-hemolytic streptococci
Tx: penicillin 10 day course
salicyclates for arthritis in involvement
glucocorticoids if severe carditis
what are the complications of AFR?
(3)
- CHF
- rheumatic pneumonitis
- rheumatic heart disease ***most common and causes valvular disease***
who is and who isn’t reccomended to get prophyllactic abx before invasive procedures to prevent endocarditis?
prophylaxsis no longer reccomended in patients with hx of RHD
EXCEPTIONS!!!
- PROSTETIC CARDIAC VALVE
- PREVIOUS ENDOCARDITIS
- CONGENITAL HEART DISEASE
what are the four main characteristis you should consider when dxing someone with strep that could lead to AFR?
- tonsillar exudates
- absence of a cough
- tender anterior lymphadenopathy
- hx of fever
only need 3/4 for dx
brucella
where does this localized?
what do we worry about with this condition?
how do you dx it? (2)
can you treat it?
gram -
highly contagious zoonosis
localizes to bone marrow and liver
can be a bioterrorism agent
DX:
- PCR
2. elisa
TX:
treatable but serious
***must treat patient and those exposed***
what are the 5 ways you can prevent the spread of brucella?
- vaccination domesticated herds
- serologic testing of animals
- slaughter infected animals
- protection of slaughter house workers
- pasteurize milk
crytococcous
what organism causes this?
what does this most commonly cause?
what does it grow?
where do you find this bacteria?
how is it transmitted?
what are the sxs? (3)
what CD4 count do you worry about
crytococcus neoformans
***most common cause of fungal meningitis***
grows mucoid colonies
budding yeast that is found in SOIL CONTAMINED WITH DREID PIGEON dung
transmission: inhalalation
SXS:
fever, cough, dyspnea
CNS in lose with less with CD4 less than 50
- headache
- meningeal sights
- RARE CRYTOCOMA with intracerebral mass that can cause obstructive hydrocephalus
crytococcus
what are the 3 things you use to DX this?
what are the tx regiments between those with HIV and those without HIV?
CXR:
nodules
pneumonitis
CSF:
india ink stain with latex agglutination
crytococcal antigen assay
tx:
HIV patient:
- oral fluconazole 10 weeks
- severe: amphotericin B 2weeks then fluconazole
non-HIV pt:
amphotericin
what people do you specifically worry about getting crytococcus?
(4)
immunodeficiency
HIV
cancer,
corticosteroids
histoplasmosis
what fungus causes this?
what does it come from?
who do you worry about it in?
transmission?
what are the 3 classifications?
1
2 things to rememeber
3 who is it commom in, what do you see?
histoplasma capsulatum
dimorphic fungus foung in soild infected with bird and bat droppings
transmission: inhalation
especially risking in late stage HIV CD4 <100
*** can see pancytopenia and anemia***
- acute
febrile, few pulmonary complaints
-
progressive disseminated
a. fatal within 6 weeks
b. ulvers in the mouth, pharynx, liver, spleen, and adrenals
- chronic progressive pulmonary histoplasmosis
**older patients esp with COPD**
a. cavitary lung disease
b. progressive pulmonary dx with calcified nodules
c. pericarditis
histoplasmosis
3 tests?
1 tx?
- CXR: milliary infiltrates
- urine antigen assay
- increased alkaline phosphatase lactatate dehydrogenase (LDH)
tx:
itracnazole for weeks to months
what is the most common opportunistic infection see in HIV/AIDS patients?
pneumocysistis
pneumocystis
what fungus causes this?
what should you know about this!***
how is it transmitted?
what are the SXS and 1 uncommon one?
what are the two dx tests? findings?
what do you treat with?
pneumocystic jiroveci pneumonia
most commmon opportunistic infeciton in HIV/AIDS
transmission: airborne, lies latent in the lung
HIV concern: CD4 count less than 200 in HIV/AIDS
SXS:
fever, fatigue, weight loss, SOB
uncommon: pneumothorax
DX:
1. CXR with interstital infiltrates
- heterogenous
- miliary
- patchy
2. blood gas
- hypoxia
- hypocapnia
Tx:
tx empirically
TMP-SMX
do you prophylax HIV patients against pneumocystis has been treated?
um…yeah! its the most common opportunistic infection in HIV/AIDS pts
give TMP-SMX if CD4 count below 200 ater suscessful treatment
botulism
what organism causes this?
where dos it come from?
what is it generalized transmitted through? (3)
what is the differences between inital presentation (2)and late progression (4)?
clostridium botulium

spore forming bacillius found in soil, produces toxin
canned food, vaccum packed, smoked food allows the toxin to be produced until it is ingested!!
SXS:
1. initial-12-36 hours after ingestion
- diplopia
- loss of accomodation
2. later
- ptosis
2. impaired extraoccular movements
3. fixed dilated pupils
4.flaccid paralysis
**needs ventilation and lead to death**
what does the botulism toxin inhibit?
inhibits the release of acetylcholine at the neuromuscular junction
botulism
how do you dx?
tx?
2 things pt will likely need
Dx:
check for toxin using mouse inoculation with serum
TX:
antitoxin available through CDC
***will need ventilation when respiratory failutre occures and IV nuitritional support during progression***
why don’t you give a baby honey? what can it cause?
dont’ give them honey for fear of botulism, can cause “floppy baby syndrome”
cholera
what is the bacterial that causes this?
what does it cause in the body?
what does the pt present with?
transmission?
what are the 2 tx options?
vibrio cholera
toxin activates adenylyl cylase in the intestinal epithelial cells in the small intesting causes hyper secretion of water and chloride ions with massive diarreah
“rice water stool” grey turbid diarreah and causes hypovolemia
transmission: fecal-oral
Dx:
- stool culture for vibrio cholerae
TX:
`1. replace fluids and electrolytes sugar/salt water, severe use IV replacement
- abx in severe cases
what are the 3 things you can do to prevent cholera?
- clean water and food
- proper waste disposal
- vaccine but protection is temporary and booster is needed every 6 months
yellow fever

what spreads this (2)?
what type of virus is this?
where does it effect?
what are the sxs? (4)
Dx?
tx?
spread by
aedes aeypti mosquito or infected monkey
flavavirus infects endothelium and liver
SXS:
- fever, heaaches, muscular aches
- liver failure
- prostration and shock
- hemmorahgia into the intestine showing melena
- renal damage/tubular necrosis
DX:
CLINICAL with IgM after 1 week
tx: no treatment!!!!
how to do prevent yellow fever?
live attenuated 17D yellow fever vaccine to anyone who has been exposed
lasts 10 years
required to travel to endemic areas
E. coli structure?
what are 3 virulence factors?
2 antigens?
gram?
gram -
somatic or O antigen LPS
flagellar or H antigen
serotype O:H
virluence factors:
- hemolysin
- intimin
- shigatoxin
whare are the 4 ways E.coli is transmitted?
- Food: cattle products, food contaminated with cattle or human feces
- water: contaminated drinking water
- animal contact: contact with farm animals ie petting zoo, farm
- person: feces or infected people
what is the most common E.coli for what we think of as e. coli?
shigella toxin-producing (STEC) also called “enterohemmorrhagic”
E. COLI0157 is the one that we usually think of when taking about e.coli outbreak!!
what is the reservoir for e.coli?
ruminant bovine

so common with GROUND BEEF INGESTION!!!
what is the seasonal peak and trough for e. coli infection?
summer peak
winter nadir
what is the most common cause of travelers diarreah?
3 sxs? and duration?
tx?
e.coli
diarreah is:
- purlulent
- bloody
- assocaited with abdominal cramping
- 5-10 duration
tx:
supportive unless severe
diptheria

what is the bacteria that causes this?
where does it LIKE TO BE?
transmission?
what are the 3 types? which is most common and what is characterized by?
cornebacterium diptheriae
likes mucous membranes esp respiratory tract and spread by respiratory secretion, particullarily in children
- TYPES
1. laryngeal
a. upper airway/bronchial obstructions
2. pharyngeal
a. MOST COMMON FORM!!
b. GRAY MEMBRANE “pseudo membrane” COVERS TONSILS AND PHARYNX
c. BULL NECK from swelling of cervical nodes
3. myocarditis/neuropathy
this occurs when the bacterial gets into the blood and settles other places creating that membrane and preventing the organs from working
diptheria
dx?
tx?
DX:
culture!!
Tx:
- horse serum antitoxin must be given in ALL cases and must be obtained from CDC
- penicillin/erythromycin
*****tx the contacts of infected with erythromycin to eradicate carrier state****
what must you do for someone who has diptheria?
isolate the patient until 3 negative samples can be obtained
how do you prevent diptheria?
diptheria-tetnus-pertussive
DTaP vaccine!!
vaccination to toxins!!
salmonellosis
what is the main bacteria that causes this?
what is it most common in?
what does it break out across states?
what are the 3 types?
salmonella typhimurium MC
POULTRY MC!!! can also include leafy greens, beef, dairy, nuts
****MULTISTATE OUTBREAKS COMMON since found in animal flocks and herds***
- enteric fever, TYPHOID FEVER
- gastroenteritis
- bacteremia
enteric fever salmonellosis
“enteric fever/typhoid fever”
where are the 3 places this replicates?
is there a prodrome?
what happens as fever develops? (5)
DX (what to keep in mind)?
Tx: 2 abx and for how long?
replicate in peyer patches, mesenteric lymph nodes, spleen
prodrome: malaise, headache, cough, sore throat
as fever developes: (peaks 7-10 days)
1. abdominal pain/distension
2. pea soup poop
3. splenomegaly
4. bradycardia
5. rash pink papules primarily on trunk during 2nd week
DX:
1. blood sample
+ during first week
- after first week
TX:
- ceftriazone
- fluoroquinolines
TWO WEEKS!!!!
salmonellosis
“gastroenteritis”
what is the incubration?
what are the 5 sxs and msot important?
DX?
tx?
most common form of salmonella infection!!
incubation 8-48 hours after ingestion of infected food or water
SXS:
fever
nausea
vomiting
bloody diarreah 3-5 days!!!!
DX:
STOOL CULTURE
Tx:
selflimited
symptomatic
salmonellosis
“bacteremia”
who is this common in?
what is this?
2 tx
prologned or recurrent fevers with bacteremia and local infection of bone, joints, pleura, pericardia, lungs
***most common in immunosuppresion person***
Tx:
- ceftriaxone
- fluoroquinolones
- tx for 2 weeks and drain absecess
shigellosis
what does this cause?
what are 5 sxs associated with this?
what are the 2 ways to dx this and what do you see?
what are 2 tx options?
dysentery
SXS:
- starts abruptly with diarrhea
- lower abdominal cramps
- tenesmus with fever chills
- loose stools with mixed blood and mucous
- tender abdomen
DX:
- stool
- sigmoidoscopy with punctate lesions, ulcers and inflammed mucose
TX:
- FLUIDS!!!!!!!
- TMP-SMX
what can HLA-B27 peopel get from shigellosis?
reactive arthritis
tetanus
what bacteria causes this?
where is it?
what does it produce that causes this?
what does it cause?
what types of wounds are most susceptible?
what are 5 symptoms?
clostridium tetani
*****present in all soiil*****
they germinate in the wounds and produce a neruotoxin tetanospasm that interferes with neurotransmission at spinal synpases
uncontrolled spasm and exaggerated reflexes
***puncture wounds most susceptible***
sxs:
- pain and tingling of stab site
- JAW TRISMUS/lockjaw
- hyperreflexes and muscle spasms
- tonic convulsions with muscle ridigity in descending fashion
- spasm of glottis and dysphagia
what is the 3 tx for tetnus?
- tetanus immune globulin IM
- penicillin
- bedrest, sedation, and ventilation often needed
what are the ways to prevent tetanus?
- active immunization in childhood
- 3-4 initial doses followed by a booster every 10 years
relapsing fever
what two bacteria cause this?
what ist this characterized by and how does it accomplush this?
3 tx options?
borrelia recurrentis-louse
borrelia croicuidare-africa
characterized by recurrent cycles of febrile episodes, separated by asymptomatic intervals of apparent recovery
***ALTERS MEMBRANE SURFACE PROTEIN TO CAUSE RELAPSING FEVER!!!***
patients clear borrellia in 3-5 days, THEN NEW ANTIGENIC VARIANTS APPEARE
**this creates the relapsing fevers**
TX:
penicillin
teracylcine
erythromycin
atypical mycobacterial disease

“nontuberculous mycobacteria”
WHAT ARE THE TWO MOST COMMON BACTERIA?
WHAT CD4 LEVELS DO YOU WORRY ABOUT?
WHAT ARE 3 DIFFERENT PRESETNATIONS?
- CAUSE, AGE, MOST COMMON, DX
- MOST COMMON,DX REQUIREMENT
- HX OF___, 3 BACTERIA, WHAT IS THE UNIQUE SYMPTOM ASSOCIATED WITH THE FIRST?
mycobacteria avium complex (40%)
mycobacteria gordgonae (25%)
effects immunocomprised esp HIV WITH CD4 LESS THAN 50
**doesn’t spread person to person…found in water, soil, animals***
- lymphadenopathy type
<5 years old
unilateral, submandibular most common
MAC MOST COMMON!!!
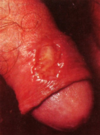
do need aspiration (seen in pic)
- chronic pulmonary disease
MAC MOST COMMON!!!
cough weight loss sputum production
must isolate 2+ sputum or bx site
- skin/soft tissue disease
hx of trauma or superficial laceration
- mycobacterium marnium
WATER, FISH
LAKE POOL AQUARIUM
1-2 MONTH IP TO GRANULMATOUS NODULAR TO ULCERATIVE LESIONS ON HANDS
“FISH TANK GRANULOMA!!!!!”
**person cleaning out their fishtank and they nick themselves and they don’t think about it!!! slowly progressive and without treatment becomes necrotic***

hookworm
explain the lifestyle cylce of this helminth
humans are the only host!
penetrate the skin and migrate in bloodstream to the pulmonary capillaries when they destroy the alveoli and are carried to the mouth by cilia
once swallowed, they attach to the small bowel mucose and suck the blood
once they mature they release eggs and the cycle is repeated
what is the difference between a light and moderate infection with hookworm?
light infection 1000 eggs per g feces
moderate infection 2,000-8,000 eggs per g feces
what percent of the worlds population is infected with hookworm?
25%
what are the sxs associated with hookworm?
(5)
- puritis at the site of penetration
- erythematous dermatitis and maculopapular or vesicular rash folllows
- pulmonary stages causes coughing with blood tinged sputum
- anemia, protein loss, malabsorption, ulcer like epigastric
- anorexia
how do you dx hookworm? what is the tx? (4)
dx:
eggs in feces
tx:
- mebendazole BID 3 days
- high protein diet
- vitamins
- ferrous sulfate
what is malaria spread by?
spread by anopheles mosquito
what are the four parasites taht cause malaria?
what is the most dangerous?
what are some brief characteristics of each?
- plasmodium vivax: dormant in liver, requires more tx
- plasmodium ovale: dorman in liver, requires more tx
- plasmodium falciparum: MALIGNANT, MOST DANGEROUS
- plasmodium malariae: chronic
what is the lifecyle of malaria?
- sporozoites in mosquito saliva
- go to liver develop in merozoites
- RBCS (this is when people get really sick)

what are the sxs of malaria? (5)
what do you dx with?
- cyclical fevers
2. leukopenia
3. hemolytic anemia
4. thrombocytopenia
- fevers, childs, nausea blah blah
DX: thick and thin geimsa stain
what are the two goals of txing malaria?
decrease parasite load
eradicate the parasite
what are the DOCs for malaria? (3)
- DOC #1 chloroquine
- doxy in pregnant, children
- mfleoquine: heart/seizure conditions
what are 3 complications of malaria?
DIC
splenic rupture
anemia
what is the best prevention for malaria?
control the mosquitos!!!
what are two conditions that provide protection against malaria?
sickle cell disease
thallesemia
pinworms
what parasite causes this?
who does it effect the most?
where are the eggs?
how long can they survive outside of the body?
transmission?
when does this become infective?
enterobius vermicularis
***CHILDREN MORE THAN ADULTS***
gravid females pass through the anus to lay eggs on the perianal skin
***EGGS are viable outside of body 2-3 weeks***
Transmission: hands, food, drinks!!
infective within a few hours
PINWORM
what are the sxs 3?
what are the 2 dx?
tx?
sxs:
1. perianal pruritis crawling sensation worse at night
2. examination at night may reveal worms in the anus or stool
3. scratching, excoriation, and secondary impetigo (staph) infection common
DX:
- capture egg on piece of tape over perianal skin
- 3 ries over 3 nights yield 90% success rate
tx:
**must tx all members of the household at same time**
albendazole, mebendazole given single dose and repeated 2-4 weeks later
leprosy

type of non typical mycobacteria’
mycobacterium leprae
numbness and paralysis of the hands and feet, travels along the nerve, debilitating
effects skin, nerves, mucous membranes

what is 2 important prevention methods for pinworms?
- wash hands before eating
- thorough linen washing
toxoplasmosis
what is this caused by?
what are associated symptoms?
what test do you want to do?
tx?
toxoplasmosis gondii
*****reactivation of latent T. gondii****
COMMON OPPORTUNISTIC INFECTION WITH AIDS PATIENTS
SXS;
- headaches
- fevers
- neurologic dysfunction
- confusion
- lethargy
- visual disturbances
- seizures
TEST OF CHOICE: MRI IMMEDIATELY
tx: TMP SMX
what is lyme disease cause by?
what is this spread by?
borrelia burgdoferi
SPIRIOCETE
spread by ioxodes scapularis
“deer tick/black legged tick”
explain the lifestyle of the ioxodes scapularis that causes lyme? which one attacks humans?

- egg
- six legged larvae-august to september
- eight legged nymph-peaks may-july, agressive, bite humans
- adult- peak in spring and fall, prefer white tailed deer
*** prefer to feed on different hosts at each life stage***

what do the ixodes secrete when they bite you?
anesthesia and anticoagulation
in order for a tick to transmit lyme how long do they have to feed for?
at least 24 hours
what are the symtoms associated with lyme disease?
(6)

- red rxn at the bite site when bit by a tick (different than bullseye)
-
erythema migrans (buls eye rash)
- 10-30 days after bite
- only 80% get this
- can disseminate - muscle/joint pain
- fatigue
- fever/chills
- swollen lymph nodes

explain the sxs of early disseminated lyme disease?
4
- erythema migrains rash 80-90%
- early presentation without the rash
a. arthalgias, olioarticular and migrator
b. post occipital headaches
c. paresthesias on face/arm/leg
early disseminated stage of lyme
6 sxs
how long?
- multiple erythema migrans
- sxs weeks to months
- lyme carditis with AV block
- neurological symptoms
- 7th nerve palsy
- lymphocytic meningitis
- post occipital headaches
- parenthesias on face, arms, legs
late symptoms of lyme
4 sxs
length of time
greater than 6 months
- arthritis (migratory or monoarthritis)
- neurologic
peripheral axonal neuropathy, mild encephalopathy, encephalomyelitis
what is chronic lyme?
patients with persistent sxs following tx of lyme disease but without relapsed infection
what are the two tests ordered for lyme in the order you order them?
what 2 fluids can you test?
whats 1 thing to keep in mind?
- ELISA
- Western blot
**antibody tests**
use synovial fluid or CSF
***don’t order a lyme test unless you think that it is actually lyme because if not could give you false positives***
what can early antibiotcsi prevent in lyme?
antibiotics in early disease can prevent seroconversion
explain the testing time for lyme?
less than 4 weeks test IgM and IgG
greater than 4 weeks test IgG
if you see the erythema migrans do you need to to the testing for lyme?
nope its made clinically dx
is reinfection with lyme likely to occure?
unlikely to occur beyond erythema migrains
what is the tx for lyme?
- doxycycline po 21 days
2. IV ceftriaxone for neuoborreliosis and some conditions like complete HB, meningoencephalitis

is prophylaxsis reccomended for lyme? what are the rules?
what do you tx with?
monitor?
Prophylaxis, NOT recommended unless these four conditions are met:
- tick has been identified as engorged deer tick that has been attached for 36 hours
- occurred in area where there is high rate of infected ticks
- prophylaxis can be started within 72 hours
- doxycycline is not contraindicated
prophylax single dose doxy 200 mg
**monitor symptoms 30 days**
what are 3 long term sequalae you worry about wiht lyme?
- persistent arthritis 5-10%, usually monoarticular (knee) for 4-5 years
- residual neurological impairment, gradual resolution
3. post-lyme syndrome: persistent fatigue, MSK pain, cognitive complaints for greater than 6 months
rocky mountain spotted fever

what bacteria causes this?
what type carries it?
how does it occur?
what is it characterized by for rash?
bacteria rickettsia ricketsiae
dermacenter ticks dog ticks, nantucket
90% april-september, highest in CHILDREN
occur in CASE CLUSTERS in hyperendemic foci
characterized by: ring skin rash, high fever, headaches and muscle pain begins as 1-5 macules rash on ankles, wrists, forearms and spreds centripetaal to trunk includes palms/soles, petechial rash on or after day 6

what are two long term sequelae of rocky mountain spotted fever?
CNS deficit
amputations
rocky mountain spotted fever
dx?
tx?
dx
indirect immunofluorescence assay (IFA)
acute and convalescent sampes 2-4 weeks apart
Tx
tetracyclines DOC with respoinse 24-72 hours
anaplasmosis

what is the name of the bacteria?
what is it spread by?
what does it infect?
what are sxs?
waht is this nickname?
anaplasmosis phagocytophilium
spread by
ioxodes scapularis black legged tick and infects granulocytes WBC
common: fever chils, headache, malasie, myalgia, arthalgia
less common: GI upset, stiff neck
nickname: summer flu
anaplasmosis:
dx?
lab tests results? 4
tx?

dx: PCR assay for DNA
labs:
- mild anemia
- thrombocytopenia
- leukopenia with left shift
- mild elevation of LFTs
tx:
adults: doxy
children: bata lactam
babesiosis

what causes this infection?
what type of infection is i?
what spreads it to humans?
where does it go?
what are the sxs and 4 unique things
what is common?
babesia microti protoazoan infection
*parasitic infection*
vector: ixodid tick
enters RBC and causes hemolysis
literally all the same SXS as other tick disease
splenomegaly, hepatomegaly, jaundice
severe: significant hemolysis
**asymptomatic disease common**
in asymptmatic babeosis…do you tx?
maybe not
monitor 4-6 weeks and may clear on its own
**if no underlying disease watch**!!
babeosis
dx?1
tx if symptomatic? 2 options
dx: PCR
tx if symptomatic
- clindmycin/quinine or azithromycin
- parasite levels more that 10% do abx PLUS transfusion till below 5%
what is the bacteria that causes tularemia?
how many people does it kill a year?
Francisella tularensis
less than 50 people a year
where can you find tularemia?
every state besides hawaii
tularemia

What is the bacterial that causes this?
what toe keep in mind? how many bacteria?
2 geographic locations?
3 things that transmit it?
7 presentations?
francisella tularensis
HIGHLY INFECTIOUS..inhalation of 10 bacteria can cause disease
biting flies: Utah, Nevada, California
tick: east rocky mountains
infects small rodents like squirrels, rabbits, hares, voles, muskrats
spread by american dog tick, lone star tick, and rocky wood tick
SXS:
- ULCEROGLANDULAR
- oculoglandular
- typhoidal syndrome-greatest mortality if left untreated
- oropharyngeal
- gastrointestinal
- secondary pneumonia
- primary inhalational pneumonia

how is tualeremia transmissed?
(6)
ingestion by food or water
inhalation
direct contact
arthropod intermediates
animal bites
no person to person spread
tularemia
dx?
2 tx?
dx: PCR
tx:
- steptomycin
- gentamycin
what are 3 conditions that are caused by body lice disease?
- louse-borne relapsing fever
- trench fever
- epidemic typhus
syphillis

what causes this?
2 ways it is transmitted?
dx? for tertiary?
Tx considerations? 2
tremponema pallidum

transmisison:
- sexually transmitted
- congenital syphilis
DX:
fluorescent treponemal antibody absorption FTA-ABS
tertiary: lumbar puncture
TX:
benzathine penicillin G 2.4 million U IM
tertiary: 3 weekly injections
neurosyphilis: penicillin every 4 hours for 10-14 days
early primary syphilis
2 characteristics of this
- chancre-painless ulcer with clean base and firm indurated margins most commonly in the genital region
- regional lymphadenopathy
secondary syphilis
lesions on skin, mucous membrane, eye, bone, kidneys, CNS, liver

late tertiary syphilis
6 sxs

- gummatous lesions involving skin, bone,viscera
- CVD
- ophthalmic lesions
- neurosyphilis
chronic meningitis
generalized paresthesia
- tabes dorsalis: chronic progressive degeneration of parenchyma
impaired proprioception
loss of vibratory sense
argyll robertson pupil (reacts to light but doesn’t accommodate)

congenital syphilis

5 signs
if not txed can develope:
interstitial keratitis
hutchinson teeth
saddle nose
deafness
CNS abnormalities

cytomegalovirus
what causes this?
who does it occur in?
what are the 3 types?
what might you see on dx?
1 tx?
human herpes virus type 5
occurs in immunocomprimised esp HIV and post transplant
3 types
- perinatal
- acute acquired CMV
- post transplant CMV
dx:
“owl eyes” on tissue biospy
antigen
tx:
- glanciclovir
acute aquired CMV
3 ways this is transmitted?
what are the sxs and the key?
what do you diferentiate this from?
transmitted via:
- breast milk
- blood transfusion
- droplet
SXS:
fever
malaise
myalgias
arthralgias
splenomegaly
atypical lymphocytes
similar to EBV infection without pharyngitis, respiratory symptoms, or antibodies
postransplant CMV
what are the 4 regions where sxs occure?
what is key preseentation buxx word?
- retinitis CD4 less than 50
“pizza pie” neovascularization and proliferative lesions
- GI
a. esophagitis
b. small bowel ulcers
c. hematochezia
d. abdominal pain - pulmonary
- neuro
how can you prevent the transmission of CMV? (3)
- limiting blood transfusions
- filtering to remove leukocytes
- restricting organ donor pool to seronegative donors
what are the 3 conditions CMV plays a role in?
IBS
atherlosclerosis
breast cancer
epstein barr virus
what is this caused by?
nickname for this?
what should they avoid?
5 symptoms?
2 dx? findings?
tx?
human herpes virus 4
“kissing disease” spread by saliva
**don’t participate in contact sports because of potential spleen rupture**
SXS:
- EXUDATIVE PHARYNGITIS
2. SOFT PALATE PETECHIAE
3. POSTERIOR CERVICAL NODE ENLARGEMENT
4. SPLENOMEGALY IN 50% OF PATIENTS
5. MACROPAPULAR/PETECHIAL RASH
DX:
- ATYPICAL LYMPHOCYTES THAT ARE LARGER AND STAIN DARKER AND VACULOATED
- MONOSPOT
tx: supportive
what should you not give to someone with mono?
ASA
what can administration of amoxicillin cause in someone who has EBV?
a rash!!
what test can give a false positive if the pt has EBV?
false positive syphilis test
what are some complications that can come from from EBV?
5
- splenic rupture
pericarditis
myocarditis
encephalitis
aseptic meningitis
norovirus
what is this?
what is this most common strain?
**most common cause of food poisoning”
Norovirus GII.4 new orleans most common circulating strain
norovirus
where so you most likely see?
what transmission?
when contagious?
reinfection?
most common complication?
“cruise ship plague”
extremely contagious
fecal oral route
salads, sandwhichs, shellfish, oyster
**contagious from moment they feel ill to at least 2 days after, reinfection common**
strikes quick 1-2 days
DEHYDRATION IS MOST COMMON AND DANGEROUS COMPLICATION esp in elderly/infant
what is the best way to prevent norovirus spread?
- handwashing
- environmental cleaning essential
rabies
how is this transmitted and by what 6 animals? which is most common?
transmitted by animals by bite or scratch
doesn’t spread by petting rabid animal, blood, urine, or feces
reservoirs:
1.Bats-MOST COMMON *any physical contact should be considered possible rabies infection until negative tests can be obtained or patient is certain there is no bite, scratch, or mucous membrane exposure
2. raccoons
3. skunks
- foxes
- cats
- woodchuck
explain the infectious path of rabies?
when are they symptomatic?
- raccoon bitten by rabid animal
- rabies enters the racoon through infectious saliva
- rabies virus spreads through the nerves to the spinal cord and brain
- when it reaches the brain the virus multiplies rapidly and passes to the salivary glands and the raccoon starts to show symptoms of the disease
**virus MUST replicate in the CNS before getting to salivary glands….they are symptomatic once at the salivary glands**
how many people have ever survived rabies?
6
explain the progression of rabies?
3 stages
2
4
3
incubation period: 4-12 weeks
prodrome:
2-10 days
paresthesia at the site of wound, with fever, headache, and anorexia
acute neurological hase:
2-7 days signs of encephalitis
mental status change
paralysis
hyperactivity
late stage:
coma
dysrhythmia,
DEATH
is there tx for rabies?
no just PEP
what is the 5 qualifications for PEP for rabies?
- suggested for anyone who was in the same room as a bat and might be unaware direct contact has occurred
- person bitten with known rabies
- person bitten with likely rabid animal
- those bitten with skunk, fox, bat, raccon
- certain non bite exposure
explain the difference between the PEP for those who have been vaccinated and those haven’t for rabies?
1. with vaccination
-cleanse, irrigate wounds
0 and 3, only 2 doses
DONT GIVE human immunoglobulin
2. without previous vaccination
cleanse and irrgation
0, 3, 7, 14, total of 4 injections
give human rabies immunoglobulin
what is the name of the post exposure protection options?
human diploid cell vaccine (HDCV)
MC reaction is skin reaction
human rabies immunoglobulin
passive and temporary, immediate
what should you do if you are bit by a suspected rabbid animal?
try to capture it so it can be tested
if you are concerned about pets having rabies, what to do?
can be monitored within 10 dayys because they will show symptoms within that time and
if reliable followup is avaliable can deferr vaccination if followup is avaliable
ebola
what family does this come from?
name?
where MC (2)?
how is it transmitted? what can you get it from?
when do you msot likely come down with it?
incubation time?
6 sxs
filovidae, ebola virus
“ebola hemmoragic fever”
MC in sierra leone, liberia
Transmission: through direct contact of blood, body fluids (urine feces, vomit, saliva, semen)…*must be symptomatic to transfer ebola* you can get it from corpses
sxs
appeare sudenly
incubation 2-21 days
8-10 post expsure most common
SXS
sudden fever
muscle pain
headache
V/D
bruising and bleeding
impaired kidney/liver function
what is the tx for ebola?
supportive!!
what is the death rate from ebola?
50-90% of patients in developing countries
what is the reccomended PPE for ebola?
gown (fluid impermeable)
goggles/face shield
facemask
double glove
disposable shoe covers
leg coverings
head covering
what is it important to do everytime a patient present with illness no matter what?!
get a travelers history!!! every freaking time!!!
how many people are living with HIV?
35 million
**how many new cases of HIV are there a year?**
50,000 new cases a year
**what is the highest risk group for HIV infection***
men having sex with men
what are the two receptors HIV uses to get into the cell?
CCR5 and CXCR4
what percent don’t know they are infected with HIV?
1/8
explain the structure of the HIV virus? why does it mutate quickly?
- RNA virus
- glycoprotein 120 and stem gp14
- viral protein p24 core antigen
- CCR5 or CXCR4 receptors
****MUTATIONS OCCUR QUICKLY SINCE THE RNA POLYMERASE USED TO MAKE THE DNA TO INSERT INTO THE HUMAN DNA ISN’T GOOD AT ITS JOB AND OFTEN THERE ARE COPYING ERROS LEADING TO MUTATIONS***
what are the two strains of HIV and where are they found?
HIV1: most common in the US “M strain”
HIV2: Africa, less aggressive
what cells does HIV infection?
CD4 Helper T cells
also monocytes and macrophages because they have the CD4 receptor
briefly explain the differences between HIV and AIDS?
HIV is in the infection
patient is usually asymptomatic or minimally symptomatic and the infection hasn’t yet effected the persons immune system yet
HAVING HIV DOESN”T MEAN YOU HAVE AIDS
AIDS
when the persons immune system has become compromised and the CD4 cells have become significantly diminished
***Acquired immunodeficiency syndrome (AIDS)***
what are the 3 options the CDC defines this?
- clinically: opprtunistic infections effect patient that wouldn’t otherwise if the pt wasn’t immunocomprimised
- biomedically: CD4 count less than 200
- historically: at some potin in the past ever had opportunistic infections or a CD4 count lower than 200
**must have one of these qualifications but you don’ thave to have all of them***
what is the percent chance of contracting HIV from a needle stick?
0.3%
how is HIV transmitted?
(4)
sexual
vertical- mother to child
parenteral- injection drug users
transfusion
Body fluids
- blood
- seme
- vaginal fluids
what racial group have the highest burden of HIV/AIDS?
african americans
what are the four stages of HIV infection?
stage 1 primary
stage 2 asymptomatic
stage 3 symptomatic with viral replication
stage 4 AIDS
stage 1 HIV
when does this occur?
length?
sxs?
short
flu-like illness
6 weeks after infection
infectious
stage 2 asymptomatic
how llong does this last?
what might they have?
HIV levels?
antibodies?
lasts 10 years
free of symptoms
possible swollen glands
levels of HIV in blood drop to low levels
HIV antibodies are detectable in the blood
stage 3 HIV
symptomatic with viral replication
when odes this occur?
what happens?
what are theu suspectible to?
at what CD4 level are HIV patients susceptible to opportunistic infection??
after 10 years viral replication is triggered at a high rate
CD4 cells destroyed in the process and the loss is significant
cause increase symptoms of HIV and increased susceptibility to opportunistic infections, disease and malignancy
**CD4 below 500 HIV infected pt is at risk for opportunistic infection**
in stage 3 HIV what are 4 diseases that can suggest the patient may progress to AIDS?

- persistent herpes-zoster infection (shingles)

- oral candidiasis
- oral hairy leukoplakia
- kaposi sarcoma
stage 4 HIV/AIDs
what is this characterzied by?
what 2 CD4 levels suggest progression to stage 4?
what are disease that a person can be susceptible for both?
7
5
immune system significantly weakened
1. CD4 less than 500
bacterial infection
TB
Herpes simplex
herpes zoster
vaginal candidiasis
karposi sarcoma
hairy leukoplakia
2. CD4 less than 200
toxoplasmosis
crytococcois
coccidiodomycosis
crytospooriosis
non-hodgkin’s lymphoma
what is the order of tests you order if suspecting HIV in patient??
what do they tell us?
what test don’t we use anymore?
- TOC #1: 4th Gen
HIV-1 and HIV-2 IgG
and IgM plus HIV-1 p24 Antigen
**tests antigen so can be detected earlier, 2-3 weeks after infection**
*if postitive then move onto next!!!!
TOC #2 if previous postivie: Multispot Or RNA PCR
**distinguishes between presence of HIV1 or HIV2**
***this testing algorithm is more accurate, faster, and less expensive than previous so not longer use western blot**
are there at home HIV tests?
yes!!!
oraquick (mouth)
or
HIV-1 test system
(prick finger, mail it in..wait a week)
what should you do if someones at home screening test is positive?
- order 4th gen HIV1/2 IgG/IgM/p24Ag
if postivie…..
- multispot HIV1
if postiive…..
- order quantitative HIV-1 PCR to get viral load!!!
what should you continue to monitor in HIV/Aids patients every 3-6 months?
- viral load
- CD4 levels
Years ago, some patients and providers made the decision to delay initiation of HIV therapy with the thought that later treatment would reduce total medication exposure and decrease adverse effects.
Do we still follow these guidlines or suggestions?
NOPE!!!!!
data suggesting that earlier therapy improves long-term immune function
what are the 5 tx options reccomended to HIV?
4 integrase strand transfer inhibitor (INSTI)-based regimens
1 ritonavir-boosted protease inhibitor-based regiment

what are the goals of HIV treatment? (4)
- supress HIV viral load
- reconstitiute the immune system and get CD4 levels back
- prevent reistance
- prevent future infections
what is the HAART tx for HIV?
4 drug classes
highly active anti-retroviral tx

- Fusion inhibitors
- nucleoside/nucleotide reverse transcriptase inhibitors
- non-nucleoside reverse transcriptase inhibitors
- protease inhibitors
*****combination of 3 active anti-retrovirals****
what is the post-exposure DOC for HIV?
when do you give it?
goal?
truvada plus raltegravir
started ideally 1-2 hours after exposure but must be within a minimum of 72 hours for best results
tx for 28 days, but high risk groups can start up to 2 weeks post exposure
***goal: prevent initial infection with antivirals!!!***
***pre-exposure HIV prophlaxsis***
who is this given in?
what does it do?
name of the drug?
how many times must you take it for it to be effective?
given to someone with partner who has HIV or someone who plans to participate in sexual activity with someone with HIV and wants to protec thtemself
PrEP is generally well-tolerated and can be dramatically successful
that early HIV treatment can reduce the risk of transmitting HIV to the uninfected partner by 96%.1
TRUVADA can prevent transmission!!!! must be take more than or equal to 4 times a week!!!!!
***who does the CDC reccomend get tested for HIV***
CDC reccomends everyone age 13-64 to be tested at least once
and!!!…
1. everyone who presents with symptoms of STD should be tested at that visit
2. testing anyone that starts new relationship
****what is the reccomendations for HIV testing in gay or bisexual testing for HIV?****
For individuals who identify as gay or bisexual testing every 3-6 months may be beneficial.
but AT LEAST ANNUALLY
****There is evidence that referring patients elsewhere for testing, e.g. to an STD clinic from an ED, Urgent Care, or PCP office, results in lower testing rates and missed diagnoses *****
fun fact!!!
*****what type of permission must be obtained before testing for HIV? 2 other considerations****
Maine state law requires that testing be voluntary undertaken that informed consent obtained either written or oral, and the patients must be informated of what a positive or negative test means
what is the most common transmitted mutations for HIV?
makes emtricitabine not work and makes HIV susceptible to tenofovir
***can people with HIV be infected with more than one strain?**
yes they can!!
***explain the life expectancy of someone living with HIV?***
life expectancy for those living with HIV has increased to approximately the same as that for HIV negative individuals
***what does HIV treatment regimen consist of?***
regimens must consist of 3 or more active agents from multiple medication classes
many pills have a combination of multiple drugs in them to increase compliance
**what was on of the first and most common combination pills used to treat HIV? what does it contain?**
atripla is one of the first combination pills
contains efavirenz, emtricitabine, tenofovir
**when should post exposure prophylaxsis be started***
within a minimum of 72 hours for best results!!!
what are 5 notifiable diseases?
Infectious Diseases – Communicable
Infectious Diseases – Dangerous
Environmental Hazards
Bio-terrorism Agents
Public Health for Action
where can you find the notifiable diseases for maine law?
22 M.R.S.A., sections 801-825
Chapter 258: Rules for the Control of Notifiable Diseases and Conditions


