ID Flashcards
What is the ID suggestions for congenital infections acronym?
CHEAP TORCHES C: Chicken pox Hepatitis B, C,E Enterovirus AIDS Parvovirus B19 Toxoplasmosis Other (TB, WMV) Rubella CMV HSV Every other STD Syphilis
What are the clinical features of a CMV infection?
17-20% will have permanent sequelae Thromobocytopenia, petechiae Microcephaly, PV calcifictions Chorioretinitis SN HL
What is the one screening test you MUST consider in CMV?
HEARING
In whom should you consider PO valganciclovir for symptomatic congential CMV?
32 wk, wt>1.8, Sx: plts, petechiae, HM, SM, IUGR, hepatitis or CNS involvement End points: Best earing test at 6 months
What is the treatment approach for CMV?
All SX neonates with CNS, SNHL, chorioretinitis Valganciclovir x 6 months MONITOR CBC (neutrophils) and creatinine
What are the classic findings in syphilis?
SNUFFLES, maculopapular rash, microcephaly, HSM
When should you evaluate an infant for congenital syphilis?
Sx of congenital syphilis Mother not treated or treatment not adequately documented Mother treated with non-penicillin regime Mother treated within 30 days of the childs birth Less than 4-fold drop in mothers titer Mother had relapse or re-infection
What is the classic triad of congenital toxoplasmosis?
- Hydrocephalus 2. Cerebral calcifications 3. Chorioretinitis
How do you confirm toxo?
PCR on CSF blood urine
What is the treatment of confirmed toxo?
Triple therapy for 12 months Steroids for eye disease VP shunt
What are the characteristics of early GBS?
Generalized
What are the characteristics of late GBS?
Focal >7 days Vertical or horizontal transmission Meningitis, osteomyelitis, soft tissue infections sepsis
What are the indications for intrapartum antibiotic prophylaxis?
Positive GBS screening cx (35-37 weeks) Previous infant with GBS d/o GBS bacteriuria during current pregnancy Delivery at 18 hours Intrapartum fever >38
What is the antibiotic selection for GBS PPX?
No allergy= penicillin or ampicillin Mild pencillin allergy= cefazolin Severe pencillin allergy= clindamycin
What is the suggested approach to fever without a source?
Toxic infants= FSWU, admit, empiric ABx 0-28 days: FSWU, admit, ABx 29-90 days: clinical and lab screening and assess risk 3-36 months: Viral, clinical FU
What are the low risk criteria for febrile infants?
29-90 days: Previously healthy Non-toxic clinical appearance No focal infection Peripheral WBC count 5-15 Absolute band count
Most common bacterial pathogens in fever without a source
0-28 day: GBS, E, coli (Listeria, S. aureus, GAS, kleb) 29-90 day: GBS, E coli (Strep pneumonia, Neiseria) 3-36 months: Strep pneumonia
What % of women who delivery an HSV infected child have no history of genital herpes?
60-80%
Empiric pneumonia-stable
Ampicilin
Empiric pneumonia- shock
ceftriaxone/vanco
Meningitis bugs neonate?
GBS, E coli, Listeria Amp + Cefotaxime
Meningitis bugs >3 months?
Strep pneumo Neiseeria H. influenzae B Ceftriaxone + Vanco
What is the evidence behind dexamethasone in meningitis?
Reduces mortality and hearing loss in H flu and possiblity S pneumo meningitis
What are the etiologies of toxic shock syndrome?
S pyogenes S aureus Empiric cloxa plus clinda GAS: pencillin and clinda + IVIG for TSS
Impetigo bugs and rx
S aureus GAS Cloxacillin, cephalexin, topical mupircoin
Cellulitis
S. aureus GAS IV: Cloxa and ancef PO: cloa and keflex
Nec fas
GAS, S aureus Cloxa or ancef plus clinda think post varicella
What are the main bugs in asplenic children?
50-90% Strep pneumoniae HIB Neiseeria Salmonella
Approach to prevention in asplenic kids?
Prevnar 13 and 23-v polysacchirde vaccine 4CMenB Influenza annual S. typhi vaccine pre travel
Presentation of cat scratch?
Unilateral swollen Cx nodes and ipsilateral conjuctivitis NO FEVER
Chronically draining Cx LN
Atypical mycobacterium
Cat scratch RX?
Bartonella henselae Azithromycin for nodes Doxcycline + rifampin for neuroretinitis
How does early localized lyme present?
Ertherma migrains Systemic sx: fever, myalgia, neck stiffness
How does early disseminated lyme present?
Multiple EM Meninigitis FACIAL NERVE PALSY
How does late disease lyme present?
Pauciarticular arthritis, peripheral neuropathy, CNS manifestations
Treatment options for lyme disease?
PO: Doxycycline, amoxicillin, cefuroxime IV: ceftriaxone, pencillin G
Prevention of mosquito and tick bites?
Physical: screens on windows and doors, fine mesh netting for cribs, long loose clothing, hat, closed shoes Repellents: DEET 12 years 30%, Icaridin for children 6M-12Y Insepct skin daily for ticks Shower within 2 hours of removal
When do you consider ABx PPx for lyme?
Single dose doxy for children > 8 years of age in exposed endemic regions
How does west nile virus present?
Peak: late summer and fall Asymptomatic 80%, fever 20%, CNS
What are the CNS syndromes associated with WNV?
Aseptic meningitis, encephalitis, acute flaccid paralysis
What are the possible complications of chicken pox?
Cerebellar ataxia, encephalitis, reye syndrome, stroke, Zoster
What are the possibly causes of facial nerve palsy in children?
HSV Otitis media Lyme disease Varicella zoster virus Cholesteatoma Facial nerve schwannoma Vestibular schwannoma
What is Ramsey Hunt syndrome?
Facial nerve palsy Varicella zoster Worse prognosis Antivirals and corticosteriods
What are the acute medical emergenies in fever in the returned traveller?
- Malaria 2. Typhoid fever 3. Meinigococcemia 4. Viral hemorrhagic fever
Delayed onset prolonged fever in a traveller?
TB Brucellosis Leishmaniasis Typhoid fever
How do you distinguish between latent and active TB?
Chest Xray
What are the reasons for a positive TST?
Mycobacterium tuberculosis infection Non-tuberculosis mycobacteria BCG Incorrect technique
What are the reasons for a false negative TST?
Incorrect technique Active TB disease Immunodeficiency states Corticosteriods Young age Malnutrition Viral infections (measles, varicella, influenza) Live attenuated vaccines (measles)
Who is at increased risk of TB?
Infants and post-pubertal adolescents Recently infected (past 2 years) Immunodeficiency states (Primary ID, HIV, Malignancy, organ transplant, immunosuppressive medications, malnutrition)
How can you diagnose pulmonary TB?
TST INterferon gamma release assays Chest Xray Gastric aspirates (three consecutive AM aspirates) Bronchoalveolar lavage Microbiology (acid fast staining, DNA, PCR)
What is the treatment for latent TB infection?
Isoniazid for 9 months
What is the treatment for TB disease?
4 drugs (INH, RIF, PYR, ETH)
What are the adverse effects of isoniazid?
Hepatotoxicty, peripheral neuropathy,
What are the adverse effects of rifampin?
Hepatotoxicity, hypersensitivity reactions, memory impairment, drug interaction, body fluids turn orange
Pyrazinamide SE
Hepatotoxicity, increased uric acid levels
Ethambutol SE
Optic neuropathy
How can you prevent vertical HIV transmission?
Antiretroviral therapy: Triple ART starting in 2nd tri IV ziovudine during labor and to newborn for 6 weeks BF is contraindicated C/s if VL >1000
How do you exclude an HIV infection?
2 separate negative PCR tests at >1 and >2 months of age
How do you confirm HIV infection?
Positive PCR x 2 to 18 months Reactive serology >18 months
How to well controlled children with HIV compare to normal children?
Increased risk of pneumococcal disease Vaccine responses not as good as healthy children Management of acute illness same
How do you approach an HIV infected child in the ER?
Clinical status Immunologic status Virologic status Antiretroviral therapy and adherence
How do you approach vaccines in HIV infected children?
Live virus: MMR in absence of severe immune compromise VZV conisder in asymptomatic cihldren BCG and oral polio CI
How do you approach Hepatitis A PEP?
Vaccine within 2 weeks of exposure in those > 12 months
How do you manage bites in daycare?
Local wound care: allow bleeding, clean with soap and water Prevention: 1. Tetanus 2. Prophylactic ABx only for moder or severe, deep puncture, face/hand/gentalia/ foot 3. HIV PEP only if HIV infected PLUS exchange of blood
How do you manage a baby born to a known HBsAG positive mom?
HBIG and HB vaccine within 12 hours of birth HB vaccine at 1 and 6 months
How do you manage a baby born to a unknown Hep B positive mom?
Stat HBsAG on Mom If results are available within 12 hours, if positive, give HBIG and HB vaccine, if not, nothing If not available, seriously consider both
What is the transmission risk of Hep C?
5% Risk factors: HIV co-infection, higher HCV viral load, elevated ALT, cirrhosis
Approach to delivery with a Hep C + mom
No evidence to support C/s Avoid invasive procedures
Approach to breastfeeding with a Hep C + mom
No evidence of transmission in breast milk
Approach to testing baby with a Hep C + mom
HCV serology at 12-18 months
What are the infectious contraindications to breastfeeding?
HIV, HTLV, Variable: TB, HSV with lesions on breast
What are the 4 moments for hand hygiene?
- Prior to the patient or patient environment contact 2. Before aseptic procedure 3. After body fluid exposure 4. After patient/pateint environment contact
What are the antibiotic stewardship principles?
- Use clinical judgement 2. Treat infection, not contamination 3. Assessment of antibiotic allergies 4. Know your local antibiogram 5. Selecting an antibiotic (narrow, optimize dosing and duration) 6. Promote vaccinations to reduce likelihood for disease
Daycare exclusion: impetigo
24 hours after treatment start
Daycare exclusion: GAS pharyngitis
24 hours after treatment start
Daycare exclusion: Pertussis
5 full days after treatment start
Daycare exclusion: E coli 0157:H7
Resolution of diarrhea and stool negative x 2
Daycare exclusion: Shigellosis
Resolution of diarrhea and stool negative x 2
Daycare exclusion: tyhoid fever
resoltuion of Sx and stool negative x 3
Daycare exclusion: hepatitis A
until 1 week after onset of illness or jaundice
Daycare exclusion: scabies
after treatment given
Treatment of mild 1st episode c diff
PO flagy
Treatment of severe 1st episode c diff
PO vanco
Treatment of severe 1st episode c diff, complicated
PO vanco + IV flagyl
What is different about hand washing in C diff?
Alcohol doesn’t kill spores Must wash with soap and water
What are the risk factors for severe influenza?
6-59 months Chronic health conditions (NM, Cardiac or pulmonary, malignancy, IC
What are the options for PO antibiotics for febrile UTIS?
Cephalosporins, clavulin, septra
What are the indications for IV ABX in UTIs?
Toxic, unable to take PO, immunocompromised host Amp/Gent
When do you do an RBUS in febrile UTI?
First febrile UTI
What are the indications for a VCUG in febrile UTI?
US evidence of hydronephrosis, renal scarring or other findings suggestive of a high grade VUR Recurrence of febrile UTI
Who should NOT receive the LIVE ATTENUATED influenza vaccine?
infants
Contraindications to LAIV?
1.
How do you vaccine for influenza in children 6-23 months?
Quadrivalent inactiated vaccine (QIV)
What are general contraindications to vaccination?
- Anaphylaxis 2. Immunodeficiency (certain vaccines) 3. Pregnancy (live) 4. GBS
How do you approach vaccination in asplenic patients?
PCV13 (Prevnar) PPSV23 (Pneumovax) >8 weeks post prevnar, 2+ MCV4 4CMenB
What is the most common cause of medically attended gastro?
Norovirus
What are the age recommendations for rotavirus vaccines?
Universally given starting at 6 weeks no later than 15 weeks (Older kids get inssussception)
When should you not give rotavirus vaccine?
Immunocompromised History of intussussception
What are the high risk conditions for pneumococcal infections?
-Chronic pulmonary and cardiac disease -SNHL requiring cochlear implants -Chronic kidney, liver, metabolic -Immunosuppresion -neurologic swallowing disorders -Hgbopathies -Chronic CSF leak -Malignancy, past HSCT
What serogroup currently causes the most meningococcal disease?
B
What is the activity of pencillins?
Non-pencillinase producing gram + cocci and gram + anaerobic DOC: Syphilis, GBS, GAS pharyngitis
What is the mechanism of pencillins?
Beta lactam ring Interefere with peptidoglycan cross-linking that is required to produce stable bacterial cell walls DO NOT cross the blood brain barrier
What is the activity of anti-staph pencillins?
Eg: methicillin, oxacillin, dicloxacillin Side chains attached to pencillin lactam ring inhibit staph Excellent activity against Staph aureus
What is the activity of aminopencillins?
Similar to pencillin Additional activity against aerobic gram negative E. Coli, Listeria, Salmonella
Extended spectrum pencillins?
Anti-pseudo pencillins Expanded gram negative spectrum Pseudo aeruginosa and proteus
% of true pencillin allergy in those who report?
Teenage patient develops pruritic maculopapular rash 1 week after starting treatment with amoxicillin for pharyngitis, allergic?
No! Classic example of EBV + amoxicillin
Activity of first generation of cephalosporins?
Gram + organisms Some activity of E coli and klebsiella species
Activity of second generation of cephalosporins?
Increased spectrum of activity of gram negative organisms Treatment of nosocoimal pneumonia No antipseudonomal activity
Activity of third generation of cephalosporins?
Broad spectrum, excellent activity against gram negative bacteria General less activity gram positive organisms
What are the two primary mechanisms of resistance of beta lactam antibiotics?
- Penicillin binding proteins: crossing linking between glycan chains (target for beta lactam antibiotics) 2. Beta lactamase: enzymes that hydrolyze the beta lactam ring of the antibiotic. SPACE: Serratia, Pseudonomas, Actineobactera, Caitrobacter, and Enterobacter
What is redman syndrome?
-Rapid infusion of vancomycin -Complain of diffuse burning, itching, dizzines -Caused by histamine release from degradulaiton of mast cells underlies reaction -Reaction
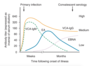
What are the three stages of pertussis infection?
Catarrheal (1-2 weeks): low grade fever, URI Sx, mild cough, apnea in infants Paroxysmal (1-6 weeks): severe cough in paroxysms and inspiratory whoop Convalescent (2-3 weeks): resolution of sympoms, cough fits may persist
What is the classic triad of malaria?
- Spiking fevers 2. Anemia 3. Splenomegaly
How is malaria diagnosed?
thick and thin smears
Which illness if referred to as the breakbone fever?
Dengue fever -Fever, severe headache, retro-orbital pain, fatigue, severemyalgias Abrovirus, transmitted by mosquitos May develop dengue hemorrhagic dever
What are the characteristics of PFAPA?
Period fever, aphthous stomatitis, pharyngitis and cervical adenitits Childhood 4 day fevers 2-8 weeks in between
What are the characteristics of familial Mediterranean fever?
What are the three Cs of measles?
Cough, coryza and conjunctivitis
Risk factors for AOM?
Mid face hypoplasia
Dayare attendance
Aboriginal
Low SES
Second hand smoke
No BF
First choice for bite antibiotics?
Amox clav
What are the three phases of pertussis?
Catarrhal: 1 week (incubation 3-21 days) coryza, conjunctiviotis, mild cough Only phase that can be treated
Paroxysmal: 2-6 weeks: severe paroxxysms of coughing with inspiratory whoop. Apnea in small infants
Convalescent: up to 1 year, gradual decrease in cough
Organism and treatment of pertussis?
Bordetella
Azithromucin, clarithromycin, erthyromycin
When do you think of a brucella infection?
Food borne unpasteruized milk
Adults working with livestock
Triad: Fever, arthralgia, HSM
how do you tell the difference between periorbital and orbital cellulitis?
Orbital: proptosis, impairment of eye movement, pain, visual acuity decreased, SICK
Salmonella incubation
6-72 hours
Campylobactera incubation
Days with abdo pain
What are the two clinical syndromes caused by Salmonella?
Gastroenteritis
Typhoid fever
Which bug has the shortest incubation period for gastro?
Staph aureus
What causes eosinophilia?
CHINA
C: Connectiv tissue diseases
H: Helminithic infections
I: Idiopathic HES
N: Neoplasia
A: Allergies
What are the most common agents in infective endocarditis?
Viridans type strp
Staph aureus
Which is tender osler nodes or Janeway lesions?
Osler nodes
What are the Duke Critiera for IE?
Major:
- Positive blood cultures
- Evidence of endocarditits on echo
Minor:
1 Predisposing conditions
- Fever
- Embolic vascular signs
- Immune complex phenomena
- Single blood culture
Diagnosis: 2 major, 1 major and 3 minor, 5 minor
When can kids with diarrhea go back to daycare?
Salmonella-diarrhea resolves, 3 negative cultures
Shigella and e coli- diahrrhea reolves and 2 negative cultures
Campylobactera- diarrhea resolves
Vomiting daycare exclusion?
>2 in 24 hours until resolves
Scabies daycare exclusion?
Until completed treatment
VARICELLA daycare exclusion?
Well enough to go
Pertussis daycare exclusion?
5 days of antibiotics
Hep A virus daycare exclusion
1 week after onset of illness or jaundice
Things that do not require daycare exclusion
Nonpurulent conjuctivitis
Rash without fver
Parvo B19
CMV
HBV
HIV
Hep A characteristics
Acute, self-limited fever, jaundice, malaise
Highly contagious, fecal-oral
Exclude x 1 week
PEP: HepA IG within 2 weeks and Hep A vaccine if>12 M
Prevention of HIV transmission
Screening in pregnancy
Antiretrovirals for Mom in pregnancy
C section pre ROM
AZT for baby x 6 weeks
NO breastfeeding
Rheumatic fever diagnostic criteria
Major:
- Migratory polyarthritis
- Carditis
- Chorea
- Subcutaneous nodules
- Erthyema marginatum
Minor: Fever, AV block, Inflam markers, Arthralgia
Rheumatic fever treatment
Anti-inflammatory meds for the joints x2 months
Pen V 10 day course
PPx: minimum 5-10 years or until age 21 (longest)
What is the progression of sinus development?
Ethmoidal-Birth
maxillary- 4
Sphenoid 5
Frontal 7-8
What is the PEP for varicella?
Vaccine for susceptibles < 72 hours
VZIG within 96 hours if: IC, pregnant, newborn of mom’s with varicella 5 before, 2 after delivery, Prem <28 or <1000g
Hep A PEP?
PPX within 2 weeks
Vaccine
IG for IC, Infants, Liver Dz
PEP for Hep B
Neonate/Unvaccination: HBIg and Vaccine
What are the virulence factors of Staph aureus?
Polysaccharide capsule
Protein A (binds IG)
Catalase inactivated hydrogen perioxide