Acute care/NICU Flashcards
What tests are done as part of the IPS (integrated prenatal screen)?
- Frist trimester screen (12 week nuchal translucency +PAPP-A+ BHCG)
- Maternal serum screen (AFP + E + HCG)
Can detect: trisomies, open NTD, Placental insufficiency
When can chorionic villius sampling be completed? What does it detect?
9-12 weeks
Chromosome abnormalities
1% pregnancy loss
When can aminocentesis be completed? What does it detect?
>16 weeks
Chromosome AbN, lung maturation, infection, renal
0.5% pregnancy loss
When is the anatomic ultrasound completed?
18-20 weeks
What is the diagnosis if a baby had: transient myeloproliferative disorder, AVSD, hypotonia, absence of rectal ganglion cells?
T21
What is the diagnosis if a baby had: cutis aplsia, cleft lip and clino/polydactyly?
T13
What is the diagnosis if a baby had rocker bottom feet, interupted aortic arch, overlapping fingers, microcephaly?

T18
What is the diagnosisif a baby had extra nuchal fold and lymphedema of the hands?
45 X0
Which of the following statements is FALSE?
- Antenatal steriods are indicated for women presenting with the risk of PTL
- Antenatal steroids are used for neuroprotection and reduce CP
- MGSO4 is indicated forwomen
- MgSO4 is used for neuroprotection and decreases CP
2
What are the prenatal interventions to prevent birth defects?
- Folic acid: decreased NTD
- Glucose control in diabetes
What are the antenatal interventions to improve outcomes in prematurity?
- Antenatal steroids,
- MgSO4
What is the most common cause of SN hearing loss?
CMV
What are the main findings in congenital CMV?
IUGR, Microcephaly, MR, deafness, HSM
What are the main findings in toxoplasmosis?
IUD, hydrocephalus, MR, chorioretinitis
What are the main findins in parvovirus B19?
Anemia, heart failure, hydrops, IUD
What are the main findings of prenatal varicella?
Hypertrophic scars, limb deformities, brain atrophy, cataracts
What are the main findings of prenatal syphilis?
Snuffles, skin findings, metaphyseal bone lesions
What is the diagnosis?

Transient neonatal pustular melanosis
What is the diagnosis?

Erytherma toxicum
Usually not hands/feet
What is the diagnosis?

Milia
How does HIV present at birth?
Usually asymptomatic at birth
PResents with CNS, DD, growth, diarrhea in the 1st year
Which of the following is NOT a risk factor for neonatal hypocalcemia?
- Maternal Graves disease
- Maternal DM
- Maternal Vitamin D defiency
- Maternal hyperparathyroidism
Maternal Graves
How can maternal diabetes effect the fetus?
HypoGlc, macrosomia, jaundice, polycythemia, small left colon syndrome, cardiomyopathy, RDS, jaundice
How does pregnancy induced hypertension effect the fetus?
IUGR, Low Plt, Low neutro, fetal demise
Prenatal NSAIDS/ASA?
Hemorrhage
PDAclosure
PPHN
Carbamazepine/VPA?
NTD
Midface hypoplasia
Phenytoin?
Midfacial hypoplasia
Hemorrhage
Fetal hydantoin syndrome (MR/IUGR/Hypoplasia of the distal phalanges)
What are risk factors for preterm delivery?
- SES status: 40Y, very low SES, low BMI
- Past Gyne/OB Hx: Pyelo, Cx abN, multiple abortion, preterm delivery
- Lifestyle: >10 cig/day, heavy work
- Pregnancy: multiples
What are risk factors for IUGR?
Maternal:HTN, renal diseas, diabetes, APL syndrome, nutritional deficiency, smoking, substance use, maternal hypoxia
Fetal: multiple gestation, placental abnormalities, infection, congenital anomaly
How can you prevent hemorrhagic disease of the newborn?
- Vitamin K IM at birth (0.5mg )
- Alternative: 2mg PO with 1st feed then 2-4 wk, 6-8 wks
What are the presentations of hemorrhagic disease of the newborn?
- Early: 1st 24 hours, due to maternal medication
- Classic: 1:400, bleeding in 1st week of life, vitamin K deficiency
- Late: 2-12th week of life (3-8 wk in CPS statement), exclusive BG
Rx: Vitamin K, FFP
When will most newborns void?
Within the first 24 hours
Can babies shiver?
Less likely to do so
Will use brown fat thermogenesis to generate heat
What % of babies pass stool in the first 24 horus?
96%
Think: Meconiumplug, Hirschprungs, meconium ileus, imperforate anus, small left colon (IDM)
What are the three questions you ask at the beginning of NRP?
- Term?
- Crying or breathing?
- Tone?
What does MRSOPA stand for in NRP?
M- Mask adjust
R- reposition head
S- suction
O- open mouth
P- Pressure increase
A-Alternative airway
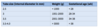
Neonatal ETT sizes?
>35 weeks: 3.5-4
>1 kg: 3
At what GA do you use a plastic bag?
What are the early onset causes of respiratory disease in newborns?
TTN, RDS, Severe malformations, pulmonary hypoplasia
What are the evolving onset causes of respiratory disease in newborns?
PTX, RDS, MAS, PPHN, pneumonia, loabr emphysema
What is the diagnosis?

Hyperinflated
Fluid in the fissures
What is the diagnosis?

RDS
Hypoinflated
Ground glass
What are the clues on history for TEF?
Apnea, cyanosis, forthing, choking with feeds
LOOK FOR ASSOCIATED: VACTERL
NPO, NG to suction, surgical consult
How does surfactant therapy help preterm babies?
Decreased mrotality, PTX, PIE
Decreases duration of vent support, LOS
No effect on IVH, BPD, NEC, ROP
What are the indications for surfactant therapy?
Intubated preterm with RDS
MAS FIO@ >50%, sick with pneumonia + OI >15
Natural is better
May repeat, max 3doses
What are the risks of surfactant therapy?
PTX, bradycardia, blocked tube, hemorrhage
What is the definition of BPD?
Oxygen dependence beyond 28 days or 36 weeks CGA
How late can apnea be considered apnea of prematurity?
44 wk CGA
When does a PDA normally close? What are the clinical features?
- Closes at 5-7 days
- Clinical features: bounding pulses, hyperdynamic precordium, loud second HS, systolic murmure
What are the risk factors for PVL?
CAN OCCUR INDEPENDENT OF IVH
PVL=CP
- Twin-twin transfusion
- Chorioamnionitis
- Asphyxia
- Severe lung disease
- Hypocarbia
- NEC
- Post natal dex
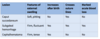
When is the screening for ROP?
Who?
When? At 4weeks of age (>26+6) OR after 31 CGA (
What are the risk factors for ROP?
- Hypotension
- Prolonged ventilation
- Oxygen therapy
What are the risk factors for NEC?
- Prematurity
- Ischemia: asphxia, CHD, PDA, severe UGR, exchange transfusions
What are the organisms and treatment for early onset sepsis (1st week of life)?
- GBS, Ecoli, Listeria
- FSWU
- Amp/Gent
What are the organisms and treatment for late onset sepsis (1 month)?
CONS, staph aures, enterococci
What are the indications for therapeutic hypothermia in HIE?
>36 weeks GA
Both 1&2:
1- Any 2 of APGAR 16 (Cord or one hour)
- Signs of moderate to severe encephalopathy
How do you cool?
Aim for temp 34+/- 0.5 degrees
Passive cooling in the community
Active cooling when in teritary centre
Method: Total body or selective cranial cooling
When? Within first 6 hours of life
Complications: hypotension, bradycardia, coagulopathy, fat necrosis
What is the outcome of HIE? What are the benefits of cooling?
Prognosis: Severe 80% morbidity, Moderate 30-50%, mild usually no deficits
Benefits of cooling: risk reduction 25% combined mortality and major NDD (NNT 11 for 1 mortality)
How do you calculate GIR?
GIR = (IV Rate (mL/hr) * Dextrose Conc (g/dL) * 1000 (mg/g))/
Weight (kg) * 60 (min/hr) * 100 (mL/dL)
What are red flags for neonatal jaundice?
Onset before 24 hours
Hemolysis
Pallor, unwell
HSM
Pale stools, dark urine
Conjugated hyperbili
What are the symptoms of acute bilirubin encephalopathy?
- Lethargy, decreased tone and suck
- Increased tone, opisthoclonus, retrocollis,
High pitched cry, seizure, coma
Any of these signs: EXCHANGE
What are the complications of exchange transfusion?
NEC, thrombocytopenia, anemia, hemolysis, portal vein thrombosis
When do you treat polycythemia?
Hct >70 or symptomatic: partial exchange transfusion
How do you calculate the volume of blood to be exchanged in partial exchange for polycythemia?
Volume= ((actual-desired hct) x wt x 90)/actual hct
What is the mechanism of TTN?
Pulmonary edema from delayed resorption of fluid from alveoli
Excess water =decreased pulmonary compliance therefore tachypnea used as a compensatory mechanism
What are the risk factors for TTN?
C/s, preterm birth, IDM, maternal asthma
What stage of lung development occurs between 16-25 weeks?
Canalicular stage: the transition between previable and potential viable lung occurs, as respiratory bronchioles and alveolar ducts are formed
What stage of lung development occurs > 25 weeks GA?
Saccular stage: potential for viability because gas exchange possible due to large and primitive forms of future alveoli, alveoli at 32 weeks= ZERO, term 50-150 million
Does alveolar growth continue after birth?
Yes, for at least two years!
What is RDS caused by?
- Surfactant deficiency
- Increase in the amount of pressure needed to open alveoli and collapse leading to V/Q mismatch and hypoxemia
- Also leads to inflammation and epithetial injury
Where is surfactant produced?
Type II alveolar cells
Composed of 90% lipids and 10% proteins
Antenatal steroids help to stimulate surfactant synthesis
What are the CXR signs of RDS?
- Low lung volumes
- Reticulogranular ground-glass appearance with air bronchograms
What are the two main groups of diseases that lead to PPHN
- Underdevelopment: pulmonary hypoplasia (CDH, CCAM, renal agensis, IUGR)
- Maldevleopment: post-term delivery, meconium
- Maladaption: normal development of pulmonary vascular bed however acive vasoconstriction occurs
What are the general management guidelines for PPHN?
- Keep O2 >90%
- Correction of acidosis (low pH causes increased PVR)
- Sedation
- Circulatory support
- iNO, sildenafil, ECMO
What are the mechanisms that keep the PDA open?
Decrease sats, PGE2, increase NO
When does functional closure of the PDA occur?
50% within 24 hour, 90% within 48 hour, all within 72hour
What are the physiologic effects of a PDA?
- Increased PBF
- Decreased SBF
What are the clinical features of a PDA?
Murmur over the entire precordium, LUSB, initially systolic only however as pulmonary pressures decrease will become present in both systole and diastole
Bounding pulses
Widened pulse pressure
Tachypnea, apnea
What is the treatment of PDA?
Indomethacin or ibuprofen
SE: decreased renal, cerebral and GI blood flow
When does vascularization of the retinal occur?
No blood vessels are present before 16 weeks
Retinal vascularization begins a 15-18 weeks, starts from optic nerve and moves outward
Vascularization is complete by 34 weeks in the nasal retina and 40 weeks in the temporal retina
What are prevention strategies for NEC?
Human milk
Trophic feeds
Avoidance of H2 blockers
Probiotics
Avoidance of prolonged ABx
What are the ways in which meconium interferes with normal breathing?
- Airway obstruction (Ball valve effect)
- Chemical irritation/pneumonitis
- Infection (riskfactor as mec is sterile)
- Surfactant disruption
- Hypoxemia
What are the risk factors for BPD?
Prematurity, mechanical ventilation, oxygen toxicity, infection, inflammation, genetics, late surfactant deficiency
What are the basic toxicology investigations?
Point of care glucose, acetaminophen, salicylate levels, serial ECGs, pregnancy tst, AXR, core temperature
What toxiodromes cause tachycardia?
- Anticholinergics
- Sympathomimetics
- Ethanol
What toxidromes cause bradycardia?
Opiods
Beta blockers
What toxidromes cause QRS widening?
TCAs
What toxidromes cause prolonged QTc
Neuroleptics
Celexa
What are the four main types of toxidromes?
- Cholinergic
- Anticholinergic
- Sympathomimetics
- Opiods
What drugs give you a cholinergic toxidrome?
- Organophosphates
- Carbamates: neostigmine!
- Alzheimers drugs
What is the acronym for a cholinergic toxidrome?
DUMBELS
Diaphoresis
Urination
Miosis
Bronchorrhea/Bradycardia
Emesis
Lacrimation
Lethargy
Salivation
What is the management of cholinergic exposure?
Early intubation, 100%
Decontamination
Atrophine until secretions and wheezing stops (muscarnic symptoms)
Inhaled atrovent/ventolin
Pralidoxime (Nicotininc symptoms)
What drugs give you anticholinergic toxidromes?
TCA
Antihistamines
Benztropine
Atropine
Lomotil
Neuroleptics
Jimson weed
What are the symptoms of an anticholinergic toxidrome?
Blind as a bat (mydriasis-dilated)
Mad as a hatter
Red as a beet
Hot as a desert
Dry as a bone
Tachycardia, absent bowel sounds
What is the management of anticholinergic exposures?
Sodium HCO3 for wide QRS
Lorazepam for agitation
Water spray and cooling fans for hyperthermia
Physostigimine is ++ toxicity
What drugs give you a sympathomimetic toxidrome?
Cocaine
Amphetamine/Meth
MDMA
Ephedrine
What are the symptoms of a sympathomimetic toxidrome?
Mydriasis
Diaphoresis
Hypertension
Tachycardia
Seizure
Hyperthermia
Psychosis
Agitation
What are the serious side effects of MDMA?
HTN
Hyperthermia: rhabdo, DIC
Hyponatremia
Serotonin syndrome
Cardiac ischemia
Hepatotoxcity
What is lysergic acid?
- LSD
- Rapid oral adsorption, symptoms within 30-60 min
Most of the potent hallucinogens
Mydriasis, HTN, Increased RR HR, diaphoresis
Massive OD: fever, autonomic dysregulation, vomiting, respiratory arrest, ICH
What is phencyclidine?
PCP or Angel Dust, similar to ketamine
Fluctuating behavior with delirium, paranoia, agitation
NYSTAGAMUS WHILE AWAKE
When do you suggest giving milk?
Only if toxin produces simple irritation
What metabolic diagnosis is represented by respiratory alkalosis?
Hyper NH4 until proven otherwise
In a baby presenting with a possible metabolic d/o with gram negative sepsis, what is the likely diagnosis?
Galactosemia
How do you calculate an anion gap?
AG= [Na+K]-[Cl+HCO3]
Normal
What are the first tests you order when suspecting a metabolic condition?
- VBG
- Electrolytes
- Glc
- Lactate
What are the three metabolic specific tests you should order?
- Urine organic acids
- Serum amino acids
- Acylcartinine profile
What is the difference between breastmilk and formula that effects the presentation of metabolic conditions?
Breastmilk 1g protein/100cc
Formula 2.5g/100cc
Therefore breastfeeding delays the presentation
What is the specific differential diagnoses for AG metabolic acidosis?
- Ketones
- Lactate
- Organic acids
What is the differential diagnosis for nonketotic hypoglycemia?
- Hyperinsulinism
- FAOD
How do you calculate BSA?
BSA=SqRt of Ht x Wt/3600
How do you calculate insensible losses?
300-400 ml/m2/day
(30 ml/kg/day)
What must you not forget with high urine outputs in water/Na dysregulation?
Osmotic diuresis from glucose
When can you give charcoal?
Within one hour of ingestion
Must have protected airway if low LOC
What can activated charcoal NOT remove?
PHAILS:
P:Potassium
H: Hydrocarbons
A: Alcohols
I: Iron
L: Lithium
S:Solvents
Is gastric lavage recommended?
NO- not been shown to improve outcomes
What is the antidote to iron?
DFO/Deferoxamine
What is the antidote to carbon monoxide?
Oxygen
What is the antidote to pesticides?
Atropine
What is the antidote to nifedipine (CCB)?
Glucagon, Insulin
What is the antidote to amitriptyline (TCA)?
Na HCO3
What is the antidote to methanol?
Fomepizole
How to hydrocarbon ingestions kill?
Aspiration and pulmonary toxicity
Present in: gasoline, nail polish remover, lighter fluid
Approach with STAT CXR and repeat 4-6 hours later
Rx with oxygen and bronchodilators
What do you see on the CXR of a hydrocarbon ingestion?
Perihilar infiltrates
Pneumatoceles
Which diabetic medication will present without hypoglycemia with Kussmaul respirations and an acidosis?
Metformin
Lactic acidosis
What drugs cause hypoglycemia?
- Glyburide (difficult to control)
- Beta blockers
- Ethanol
- Salicylates
What is the toxic metabolite of acetaminophen? What dose is toxic?
NAPQI
Dose 150 mg/kg
Hepatoxicity reported >90mg/kg/day
How will an acetaminophen overdose present?
AG metabolic acidosis
Acute tubular necrosis
Fulminant liver failure
What is the treatment of acetaminophen overdose?
Activated charcoal within 1 hour
Avoid AC if sedated
NAC dosing based on Rumack-Matthew nomogram
Best outcomes if NAC started within 8 hours
Follow LFTS/live function
What are the symptoms of a salicylate overdose?
Hyperpnea/tachypnea
AG metabolic acidosis
Nausea, vomiting, GI bleed
TINNITUS (progresses to hearing loss)
Hyperglycemia
Diaphoersis
What is the management of a salicylate overdose?
Charcoal up to 6 hours (to avoid bezoar formation)
Glucose to all patients
Treat hypokalemia
Alkalinize serum
Hemodialysis for CNS sypmtoms
What are the radio-opaque drugs?
COINS
Chloral Hydrate
Opiod packets
Iron and other heavy metals
Neuroleptics
Sustained release tablets
What is the presentation of iron?
10% of intentional overdoses are fatal
Stage 1 (30min-6hr): Nausea, vomiting, diarrhea
Stage 2 (6-12 hours): “Quiesent phase”
Stage 3 (12-24 hours): Metabolic acidosis, shock, GI bleed, coagulopathy, resp failure
Stage 4 (2-3 days): ARDS, liver failure
Stage 5 (3-4 weeks): GI stricture at gastric outlet
What are the clues to iron exposure?
GI symptoms
Acidosis
Multiorgan failure
What is the treatment of iron exposure?
No role for either charcoal or gastric lavage
Fluid resus
WBI if tablets seen or ,6 hours
IV deferoxamine 15mg/kg/hr until urine clears
What is unique about the presentation of isoproyl alcohol ingestion?
Ketosis without acidosis (cannot be metabolized past ketones)
Why is methanol so toxic?
- Less inebriating than ethanol
- Toxicity in little as one teaspoon
- Formate causes retinal injury
Profound AG acidosis presents late
What substance is in antifreeze, paints, brake fluid?
Ethylene glycol
Colorless, ordorless, sweet taste
Inebriation without smell of ethnaol
Metabolic acidosis
Hypocalcemia (prolonged QTc)
Oxalate crystals
What are the clues to toxic alcohol exposures?
Inebriation
Odor
Osmolar gap or acidosis
How do you calculate osmolality?
Two salts and a sticky bun
OG= 2x NA + Glucose + BUN
How do you calculate an osmolar gap?
OG= Measured-Calculated Osmolarlity
What is the general management of toxic alcohol exposure?
- Wash skin if exposed
- Fomepizole or ethanol
- Hemodialysis if high AG acidosis or end-organ damage
- Cofactor therapy with folic acid
- Thiamine and pyridoxine
What are the common TCAs to be ingested?
Amitriptyline, despiramine, imipramine
What are the clinical effects of TCA overdoses?
Inhibit NE and serotonin reuptake
Block cardiac fast Na channels- wide QRS
block muscarinic receptors-weakly anticholinergic
Block histamine receptors- sedation
Block alpha receptors- hypotension
block GABA- seizures
What is the treatment for a TCA overdose?
Activated charcoal
Intubation
NAHCO3 for QRS >100mS
NE if hypotension
How does carbon monoxide poisoining present?
Headache, dizziness, nausea, confusion, seizure, syncope, coma
Most commonly from smoke inhalation
Tasteless, odourless, non-irritating gas
240x higher affinity to Hb than O2
Dysrhythmia, cardiac arrest in up to 30%
Cherry red skin colour after excessive exposure
What is the treatment of a carbon monoxide exposure?
Remove from source and r/o smoke inhalation
Check cyanide level
Follow ECG and cardiac enzymes
Provide 100% FiO2
Hyperbaric O2 if COHb> 25%
What are the clues to a carbon monoxide exposure?
Flu-like symptoms
Fire exposure
Normal Sats
What is the most common cause of pediatric death in children 1-4 years?
Trauma
What preventative strategies are used to prevent submersion injury?
- Four sided self closing fence with a self locking gate (MOST EFFECTIVE)
- At least 4 feet high
- Toddlers should always be wtihin arms length of an adult, even in a tub
- 1 adult per baby, 1 adult per 2 young children
- Swimming
What are the risk factors for submersion injury?
- Leaving children unattended
- Alcohol or drug abuse
- Limited swimming ability
- Underlying medical condition: seizure disorder, toxin, prolonged QTc, syncope
A 14 year old male is pulled from an icy lake after being found face down. What is the most important strategy influencing survival?
- Imediate c-spine
- immediate CPR by rescuers
- Passive external rewarming, EMS activation and transport to a health care facility
- Early placement of definitive airway
2
What are GOOD prognostic indicators in submersion injuries?
IMMEDIATE BYSTANDER CPR is the most important factor influencing survival
ROSC in
Submersion
Pupils equal and reactive at the scene
NSR at scene
What are BAD prognostic indicators in submersion injuries?
Delayed CPR
ROSC > 25 min
Submersion >10 min
What do you see at different degrees of hypothermia?
31-32: Normal ECG, Increased HR, Increased BP, loss of shivering
28-31: Decreased HR, Decreased BP, Flipped T, afib, sluggish dilated pupils
What are the ECG changes you will see in hypothermia?
- Marked bradycardia
- First degree AV block
- Osborn or J waves
- Associated prolonged QTc and bradycardia
What are the principles of rewarming without a pulse?
>30: CPR, IV meds as needed, defibrillation as needed
Gentle intubation
Warm O2, Warm IVF
What is heat stroke?
Core temp >40 and CNS dysfuntion
Headache, disorientation, dizziness, weakness, gait disturbance
What are the clues to a superficial partial thickness burn?
Pain, moist, blisters
What is the initial management of burns?
- Cover sterile bandages
- Early cooling (
- TETANUS
- Analgesia
- Remove shoulder clothing
What are indications for early intubation in burns?
Carbonaceous sputum
Singed nasal hairs
Soot in airway
Hoarseness
How do you calculate fluid management in burns?
Age > 9: Rule of 9s
Age
Age > 5: Parkland formula: 4cc/kg/BSA over 24 hours, 1st half in 8 hours, 2nd half in 16 hours
What are the physical findings of a post term infant?
Cracked, dry, peeling skin
Creases covering the entire sole of the foot
Mature, long fingernails
Basence of lanugo over the back
Palpable breast buds
What is the way to remember gastroschisis vs omphalocele?
Gastroschisis: Good baby, bad bowel
Omphalocele: Baby baby, good bowel
What is the appearance of gastroschosis?
Centrally located, full thickness, abdo wall defect
- Extruded intestine NEVER has protective sac
- Umbilical cord intact to the left of the defect
25% associated with bowel atresias
What are the risk factors for gastroschsis?
Young mom, EtOH abuse, ASA, ibuprofen, pseudoephedrine
What is the immediate management of a baby with gastrochisis?
Temp regulatin
Protective covering
Right lateral position and ensure bowel not kinked
NG decompression
IV fluids 2-3 maintenance
Surgical correction ASAP
What is the clinical appearnace of omphalocele?
- Protective membrane covered gut
- Cord is always attached to membrane
What is the likely mortality of a baby with omphalocele?
30%
What are the syndromes associated with omphalocele?
Beckwith-Wiedemann, conjoined twins, T18, meningomyelocele, imperforate anus
What are the breastfeeding benefits for baby?
Immunologic: IgA, lower rate of OM, LRTI, gastro,
Less allergenic
Less constipating
Better jaw/mandible development
What are the breastfeeding benefits for Mom?
ABCDEFGH
Allergic conidtions reduced
Best food for infant
Close relationship with mother
Development of IQ, jaws, mouth
Economical
Fitness
Guards against cancers for mother (breast, ovary, uterus)
Hemorrhage reduced postpartum
How does breastmilk compared to cow milks?
67kcal/100cc
Lower portein content
Greater whey
Both lactose based
More fat!
Richer in A
Lower FE
What are the metabolic complications of TPN?
Electrolyte Ab
Glucose AB
Ca/PO4 abN
Cholestasis
Line infection
Bone D/o
What is the differential diagnosis for ambiguous gentalia?
- Undervirilization of males
- Virilization of females
- True hermphroditism
- Incomplete gonadal dysgenesis
What does VACTERL stand for?
Verterbal
Anal
Cardiac (VSD)
TEF
Eo Atresia
Renal
Limb
NORMAL DEVELOP AND INTELLIGENCE
What does CHARGE stand for?
Coloboma
Heart d/s
Atresia (chonal)
Retarded growth and developemtn
Gential AbN
Ear abN
How does galactosemia present?
Within first few days after bith
Jaundice, vomiting, HSM, FTT, poor feeding, lethargy
E coli sepsis!
What are the causes of early onset hemorhhagic disease of the newborn?
0-24 hours
Maternal drugs
Inherited coagulopathy
What are the causes of classic hemorhhagic disease of the newborn?
Vitamin K deficiency
BF
(
What are the causes of late onset hemorhagic disease of the newborn?
Cholestatis
Warfarin
ABLP deficiency
Lack of Vitamin K
What are the components of the APGAR scores?
Appearance
Pulse
Grimace
Activity
Respiratory effort
When should rH negative moms receive rHoGAM?
28 weeks
Invasive procedures
What is the most common cause of severe thrombocytopenias in the first day of life?
Neonatal alloimmune thrombocytopenia (NAIT)
Maternal alloimmune antibodies against HPA on fetal platelets results in NAIT
Can occur in first pregnancy
What is the treatment of NAIT?
Need to administer a specific HPA type to avoid continued destruction of transfused platelets.
Subsequent pregnancies: weekly IVIG to minimize the incidence of thrombocytopneia and ICH.
Which infants have a set-up for ABO incompatilibility?
Mom O, Infants A or B
Individuals with type A or B have naturally occuring Anti-A and anti B isoantibodies that are frequently igM and do not cross the placenta
Individuals with type O have isoantibodies that are IgG and can cross the placenta.
What are the contraindications to a lumbar puncture?
- Low platelets
- Infections of the skin at the puncture site
- Lumbosacral anomalies
- Cardioresp instability
- Increased ICP
What are the contraindications to breastfeeding?
HIV
HTLV
Galactosemia
Active TB
What does cryo contain?
Plasma thats been spun: fibringoen, factors V,VIII, XIII, VWF
1 unit/5 kg (1 unit=15mL)
What is the dose of FFP?
10 ml/kg
Should you never glue a hand?
NO
Which is more likely to cause infection: dog or cat bites?
CAT >50% will get infected
When is antimicrobial therapy indicated for bite wounds?
- Moderate or severe bite wounds
- Puncture wounds
- Facial bites
- Hand and foot bites
- Wounds in IC and asplenic people
- Wounds with signs of infection