Hypertension Flashcards
Normal BP
less than 120
and
Less than 80

Elevated BP
120 - 129
and
Less than 80

Stage 1 Hypertension
High Blood Pressure
130 - 139
or
80 - 89

Stage 2 hypertension
High blood pressure
140 or higher
or
90 or higher
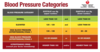
Hypertensive Crisis
Consult your doctor immediately
Higher than 180
and/or
Higher than 120

What is primary (or essential) hypertension
Primary (or essential) hypertension (90-95%): unclear etiology but multifactorial (genetic and environmental factors)
Recall that secondary hypertension (5-10%) is hypertension contributing to another disease or medications
What are the complications of hypertension
Left ventricular hypertrophy
Heart failure
ischemic stroke
Intracerebral hemorrhage
Ischemic heart disease
Chronic kidney disease and end-stage renal disease (bad for kidneys)
Risk of CVD doubles with every 20 mmHg increase, starting at 115 mmHg
Treatment of hypertension
address secondary cause, if present
lifestyle modification
Pharmacological therapy
What are first-line hypertension drugs?
What are different drug classes associated with hypertension drugs?
- roughly equivalent BP lowering efficacy
- Consider: cost, side effects, other health conditions, occasionally ethnicity
- Drug classes
- Thiazide diuretic
- Angiotensin-converting enzyme inhibitor (ACEI)
- Angiotensin II receptor blocker (ARB)
- Long-acting calcium channel blocker (most often dihydropyridines (DHP))
Understand the physiological mechanisms that can be targeted for the treatment of hypertension
Lifestyle Modifications
Weight reduction
Adopt DASH eating plan
Dietary sodium reduction
Physical activity
Moderation of alcohol consumption
Antihypertensives
Reduce sympathetic tone/stimulation
Beta-blockers (propranolol), alpha blockers (prazosin), alpha two agonist (clonidine)
- Antihypertensives; reduce plasma volume: diuretics
- gets rid of more fluid and therefore decrease blood volume
- Relax arterial smooth muscle, cause vasodilation (smooth muscle tone)
- Renin-angiotensin inhibitors
- Ca2+ channel blockers
What does Short term MAP regulation look like?
Depends on increases in CO and TPR through baroreceptor reflexes and SNS activation

What does Long-term MAP regulation look like?
vasoconstriction due to angiotensin II, increased fluid volume due to aldosterone and vasopressin

MAP =
CO x TRP
Beta-blockers = decrease in force and rate of cardiac contraction = decrease CO
Diuretics, angiotensin inhibitors, beta receptor blockers = Decrease blood volume = decrease CO
Peripherally acting sympatholytics, Ca channel blockers, direct vasodilators, angiotensin inhibitors = relax vascular smooth muscle = decrease TPR
Centrally acting sympatholytics, Beta receptor blockers -> decreased sympathetic outflow = decrease CO and TPR

Diuretics (“water pills”)
- Often a first choice for treatment of mild/moderate hypertension
- Low-cost but effective drugs: treatment of hypertension associated with reduced morbidity and mortality
- Act on various segments of the nephron to produce an increase in renal sodium excretion leading to an increase in urine volume

What are the initial and delayed effects of diuretics (“water pills”)
Initial effects: reduction in blood volume resulting in decreased blood pressure due to decreases in cardiac output (stroke volume)
Delayed effects: after 6-8 weeks, blood volume and cardiac output are restored back to normal, but peripheral resistance declines

What are mediators in secretion and reabsorption?
Within the kidney tubules
Tubular epithelial cells
Luminal membrane facing tubule lumen
Basolateral membrane near capillaries
Tight junctions
Membranes on both sides contain channels and transporters that move solutes
Reabsorption is regulated by transporters, not through the cells because the tight junctions block

Explain sodium Reabsorption
Two Steps
- Diffuses from lumen into epithelial cells
- Actively transported out of cell on basolateral side
Specific channels and transporters on luminal side differ in different regions of the tubules, but pattern remains the same

Furosemide
(Lasix)
Loop diuretics
Ethacrynic acid (edecrin)
Block Na/K/2CL cotransporter (NKCC2) in ascending limb of loop of henle
Na continues through the lumen of the nephron and reaches the collecting duct. More water is retained in the lumen due to the osmotic effect of Na+
Most common uses: edema; short-term management of severe hypertension
Highest efficacy of the diuretics

What is the highest efficacy of the diuretics
Furosemide
Loop diuretic
What are the major side effects of furosemide?
Hypokalemia (low potassium)
- K+ reabsorption decreased in loop
- K+ secretion in collecting duct is increased due to higher level of Na+ in the lumen
hydrochlorothiazide
Thiazide diuretics
Hydrochlorothiazide, chlorthalidone
Block Na/Cl cotransporter (NCC) in distal tubule
Major use: long-term outpatient management of hypertension
Efficacy to cause diuresis is lower than loop diuretics

What are the adverse effects of Thiazide diuretics (hydrochlorothiazide, chlorthalidone)?
Adverse effects: similar to loop diuretics, can cause hypokalemia due to higher levels of sodium in the collecting duct
Chlorthalidone is more efficacious and longer acting than* *hctz* but also carries *greater* *risk of hypokalemia





















