GIT Pathology Flashcards

Oral leukoplakia
- older men
- not removed by scraping
- clinical term; vast majority (~90%) of them are
benign; 3 to 7% undergo malignant transformation - buccal mucosa, tongue, floor of mouth
- hyperkeratosis
- dysplasia but no invasion
- Assoc w:
- tobacco use
- HPV (16, 18)
- chronic friction ex. ill fitting dentures

Erythroplakia
- due to EBV -> dysplasia -> malignant transformation in more than 50% of cases
- no hyperkeratosis; poorly circumscribed
- rough shaggy patches on lateral aspects of tongue

Squamous cell carcinoma (oral)
- Right: Keratin whorls
- mutations: p53 & p16 (cyclin)
- Developed from erythroplakia
- HPV 16, 18
- tobacco and alcohol are risk factors
Oral hairy leukoplakia
- no malignant potential
- almost always seen in HIV Pt
- strong assoc w EBV
- white confluent hairy hyperkeratosis
- layers of keratotic squames on underlying mucosal acanthosis (hyperkeratotic)
Hiatal hernia
- in older Pt
- Sx:
- heart burn (sliding-type) most common -> cardia of stomach pressed up towards esopagus -> risk of reflux
- resp problems due to stomach taking up space of lungs
- Dx:
- hour glass appearance
Achalasia/Cardiospasm
- incomplete relaxation of LES in response to swallowing
- functional esophageal obstruction
- 3 main features
- Aperistalsis
- Partial or incomplete relaxation of LES
- incr resting tone of LES
- Primary
- loss or absence of ganglion cells in myenteric plexus
- loss of inhibitory innervation of LES & smooth m. due to loss of NO/VIP
- Secondary (aka pseudoachalasia): impaired fx due to
- Chagas (T. cruzi)
- polio
- paraneoplastic syndrome
- sarcoidosis
- Sx:
- Dysphagia
- Odynophagia
- Reflux of contents
- hallitosis
- Vomiting
- Aspiration pneumonia
- Progressive dilation of esophagus above LES
- Dx:
- HIgh LES pressure on manometry,
- bird-beak sign on barium swallow
- Risk of developing squamous cell carcinoma (5% of cases)
Mallory Weiss syndrome
- longitudinal tears in mucosal wall of esophageal-gastric junction
- frequently in alcoholics & bulimics after a severe bout of retching
- inadequate relaxation of LES during vomiting
- tear may be only mucosal or transmural
- hememetesis -> painful
- usually heals but some times fatal
- **risk of Boerhaave syndrome -> air in mediastinum **(Pathoma)
Esophagitis
- Irritants: alcohol, acids, alkalis
- Infections:
- Allergic: eosinophilic esophagitis
- hyperemia
- presence of inflammatory cells: eos, neutrophils
- elongation of LP papillae
- basal zone hyperplasia
- Uremia
- Anticancers: bisphosphonates
Reflux esophagitis
- Causes:
- CNS depressants
- hypothyroidism
- pregnancy
- nasogastric tube
- alcohol
- tobacco
- **Etiopath: **Reflux of gastric juices is central to the development of mucosal injury in GERD. In severe cases, duodenal bile reflux may exacerbate the damage. Conditions that decrease LES tone or increase abdominal pressure contribute to GERD and include alcohol and tobacco use, obesity, central nervous system depressants, pregnancy, hiatal hernia (discussed later), delayed gastric emptying, and increased gastric volume. In many cases, no definitive cause is identified.
- Sx:
- dyspepsia
- burning sensation
- water brash
- sx worsen after lying down or after a big meal
- nocturnal cough
- Complications:
- bleeding
- stricture formation
- aspiration pneumonitis
- Barrett’s esophagus & adenocarcinoma

Barrett’s esophagus
- more common in white men
- lower 1/3 of esophagus
- non-ciliated columnar cell w Goblet cells
- salmon pink patch, tongue or large area above EG junction
- 30 to 40 x incr of adenocarcinoma


SCC of esophagus
- most common type of esophageal cancer; higher incidence in central Asia and N. China
- middle aged Blacks at higher risk than whites
- Etiology and associations with irritation
- Diet: vitamin deficiency, high nitrite content, fungal contamination
- Lifestyle: smoking, alcohol, urban env., very hot tea
- Esophageal disorders: longstanding esophagitis, achalasia, Plummer-Vinson syndrome (dysphagia, iron deficiency, glossitis, esophageal web, women);
- esophageal squamous cell carcinoma
risk is increased; therefore, it is considered a premalignant
process - associated with koilonychia, glossitic, chelitis,
and splenomegaly
- esophageal squamous cell carcinoma
- Genetic: Celiac disease, ectodermal dysplaisa (Tylosis), racial factors
- Gross: most common in middle 1/3
- Patterns: exophytic, diffusely infiltrative, ulcerated/excavated)
- Metastasis of SCC: direct to trachea or heart OR lymphatics
- Image below:
- Left: Ulcerated mass
- Right: narrowing of lumen


Adenocarcinoma of esophagus
- Lower 1/3 of esophagus
- more common in white men
- Barrett is precursor lesion
- poor prognosis
- Signs and Sx similar to Barrett
- multi-step dysplasia
Pyloric stenosis
- Acquired: chronic antral gastritis, peptic ulcers, malignancy
- Congenital:
- more common in 1st boy
- concentric hypertrophy of circular muscle coat
- Sx: presents 2 wk after birth -> regurg, projectile voimtting (nonbilious), palpable epigastric mass (olive-like), visible peristalsis
- Rx: surgery (myxotomy)
H. pylori
- non-invasive, urease+ bacillus
- mostly in antrum of stomach
- virulence factor = cagA toxin
- Rx: invasive tests (urease test, histopath, PCR) & non-invasive test (urea breath test, serology IgG, IgA), PCR in saliva & faeces)
- assoc w 2 patterns of gastritis
- superficial antral inflammation
- multifocal gastric atrophy
- Risk of developing PUD, gastric lymphoma, gastric carcinoma
Types of Gastritis
- Erosive (shallow ulcer)
- NSAID, oral iron, KCl
- Ethanol
- acute stress
- Chronic (non-erosive) gastritis
- H. pylori
- Pernicious anemia
- Sx: may be asx
- epigastric pain, nausea, vomiting
- hematemesis and melena
- bleeding can be fatal
Acute gastritis
- Etiological factors: anything incr acid production or decr mucosal protection
- NSAIDS: PG normally maintain blood flow, incr. mucus & bicarb secretion, augment epithelial defenses
- Alcohol
- Smoking
- Severe stress
- Trauma
- severe burn (Curling ulcer)
- Uremia
- Ischemia and shock
- Systemic infections
- incr ICP (Cushing ulcer) -> incr Vagal stimulation -> ACh release -> incr acid production
- Reactive Gastropathy:
- common in gastric surgeries that bypass pylorus
- watermelon stomach (GAVE)
- common in Pt on iron supplements

Chronic Gastritis: either from autoimmune or H. pylori causes
Etiology:
- Left image: chronic infection w H pylori;
- Right image: Warthin-Starry silver stain for H. pylori
- immunologic causes: anti-parietal or anti-IF Abs; achlorydia & incr. gastrin levels
- Alcohol and smoking
- post-surgical
- radiation
- Granulomatous (Crohn’s disease, sarcoidosis)
Morphology
- Endoscopy: thick mucosal folds
- Microscopy:
- Inflammatory infiltrate in LP: lymphocytes & plasma cells
- PMN in surface epithelium and glandular lumen
- Reactive lymphoid aggregates, mainly superficial
- intestinal metaplasia and glandular atrophy +/- dysplasia
Fundic type (Type A)
- Etiopath: autoimmune attack on parietal cells in stomach body and fundus
- see autoimmune gastritis card for complete def
Antral type (Type B)
- Gross: loss of rugal folds in antrum
- Micro:
- H. pylori in mucus layer of epithelium -> secretes ureases and proteases -> induce inflammation
- foci of lymphocytes, plasma cells & neutrophils
- intestinal metaplasia
- Etiopath:
- incr risk of duodenal and gastric ulcers, gastric adenocarcinoma, MALT lymphoma
- most common form of gastritis in US
Autoimmune Gastritis
- mainly involves body and fundus
- Etiopath: auto-anti-parietal cells or anti-IF cells Ab
- gland destruction
- atrophy
- Achlorydia
- Pernicious anemia
- Gross: loss of rugal folds in body and fundus
- Micro:
- mucosal atrophy w loss of glands and parietal cell
- lymphocytes and plasma cells in mucosa
- PMN may be present and indicate active inflammation despsite chronicity
- intestinal metaplasia marked by presence ofGoblet cells
Gastric ulcers
- Loss of mucosa that extends through muscularis mucosae or deeper
- Healing time greater than with erosions
- Common (gastric and duodenal)
- Peptic Ulcers
– Exposure to aggressive action of acidic peptic juices
– Chronic, often solitary lesions
Acute Gastric Ulcers
- Severe trauma, major surgeries
- Extensive burns (Curling ulcers)
- Head injuries/ intracranial lesions (Cushing Ulcers)
- Morphology:
- Multiple, small and circular
- Gastric rugae are normal
- Base usually not indurated (no fibrosis)
- Adjacent gastric mucosa normal or with reactive changes
- Etiopath:
– Systemic acidosis and hypoxia (severe trauma and
burns)
– Vagal stimulation (intra cranial lesions)
- Sx: Can present with massive upper GIT bleed
- Usually multiple and asymptomatic
- 5-10% of patients admitted in Intensive Care Unit

Chronic Gastric ulcers: PUD
- Sites (Descending order)
– Duodenum proximal
– Stomach
– Gastro esophageal junction
– Margins of gastrojejunostomy
– Meckel’s diverticulum
– Stomach, duodenum and jejunum in Zollinger Ellison syndrome -> Gastrinoma -> high Gastrin
- Morphology
- 50% < 2cms
- Round to oval, punched out with relatively
straight walls
* Sharp and raised margins but not everted
* Depth varies but may penetrate entire wall
* Smooth and clean base
* Radiating surrounding mucosal folds
* Active ulcer has four zones
* Necrotic fibrinoid debris
* Non specific inflammatory infiltrate (predominantly neutrophilic)
* Granulation tissue
* Fibrosis and collagenous scar
* Typically features of chronic gastritis in adjacent mucosa * Etiopath: balance bw damaging forces and Gastro Duodenal Mucosal Defenses
* incr post-prandial gastrin & decr SST leading to incr basal gastric acid secretion 1) H. pylori- 70% of gastric and 90% of duodenal ulcers 2) NSAIDS- inhibit prostaglandin synthesis 3) SMOKING- impairs mucosal blood flow 4) ALCOHOL 5) PSYCHOLOGICAL STRESS 6) ZOLLINGER ELLISON SYNDROME
Zollinger-Ellison Syndrome
- Multiple ulcers
- Hypertrophy of Brunner’s glands
Sx:
- Burning epigastric pain 1-3 hours after meals
- Relieved by food and alkali
- Worse at night
- Associated weight loss
- Gastric outlet obstruction
- Complications
- Bleeding
- Perforation
- Gastric outlet obstruction
- Malignant transformation
Reactive Gastropathy
- The NSAID lesion
- Other drugs/medications
– Iron, Kayexalate
- Acid, alkali, alcohol
- Duodenopancreatic reflux

Gastric adenocarcinoma
- Highest occurrence in Japan and S. Korea
- Two distinct subtypes: intestinal & diffuse
- Overall unfavorable prognosis
- Sites: Pylorus/Antrum (50-60%), Cardia 25%, Body and Fundus
- Growth Pattern: Exophytic, Flat, Excavated
- Spread: local, transcoelomic, lymphatic, hematogenous
- Sx:
- Mostly asymptomatic in early stages
- Non specific weight loss, anorexia, abdominal
pain
* Pyloric outlet obstruction * C&C * **Krukenberg tumor; assoc w diffuse type** * Virchow lymph node: L. supraclavicular node * **Sister Mary Joseph nodule:** palpable nodule bulging **peri-umbilical** as a result of metastasis * Prognosis depends upon depth of invasion and nodal status
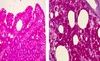
Intestinal type (LEFT IMAGE)
- In setting of chronic gastritis
- Neoplastic glands resemble intestinal epithelium (colon)
- Associated with H. pylori
- Intestinal metaplasiais precursor lesion
- More common in high- risk populations
- heaped-up margins,
- loss of rugae due to infiltration of tumour
- hyper-glandular, differentiated
- Etiopath: nitrosamines (smoked foods), A blood type,
Diffuse type (RIGHT IMAGE)
- No gland formation, thicker
- not related to H. pylori
- Single cells, sheets, clusters Signet ring cells
- poorly-differentiated
- More common in familial types with young female predominance
- Linitis plastic appearance (leather bottle stomach)
- Etiopath: Genetic -> E-Cadherins, younger women, No intestinal metaplasia

Gastrointestinal Stromal Tumors (GIST)
- Mesenchymal tumors
- Derived from cells of Cajal – the pace maker cells
- Many of these previously misdiagnosed as leiomyomata
- Anywhere in GIT: Esophagus, Stomach, small intestine, large intestine
- Can be benign or malignant: Based on size and mitoses
- Usually submucosal
- Whorls and bundles of spindle shaped cells
- C-kit (CD 117) is the tumor marker