Female Pathology - Uterus Flashcards
How can the functional endometrium be subdivided?
-
Secretory endometrium
- Tortuous secretory glands + pseudodecidualized stroma
- Proliferative endometrium

What conditions can affect the uterine body?
- Inflammation/endometritis/pelvic inflammatory disease
- Polyps
- Adenomyosis
- Leiomyomas
- Premalignant (hyperplasia)
- Malignancies
What is common between the conditions that affect the uterine body?
All uterine body conditions may lead to dysfunctional and/or abnormal bleeding
- What is endometritis?
- What can cause it?
- What can be seen in the stroma?
-
Inflammation of Endometrium
- Acute/Chronic
- Due to:
- PID
- Retained POC
- IUD
- Plasma cells in the endometrial stroma

Endometrial Polyps
- Definition:
- Clinical Signs:
- Prevalence:
- Immunohistochemistry:
- Polyp Type:
- Appearance of glands:
- Benign biphasic neoplastic growth (glands and stroma)
- Dysfuntional bleeding
- Most common ± menopause
- Rearrangement of 6p21
- Intrauterine sessile or pedunculated growth
- Dilated glands

Endometriosis:
- Definition:
- Clinical Signs:
- Characteristic Finding:
- Discharge of blood leads to ….
- Histology:
- Presence of endometrial glands and stroma outside of uterus
- Cyclic bleeding
- Can become blood filled cysts (chocolate cyst)
- Discharge of blood leads to reactive changes, fibrosis and adhesions
-
Histology:
- Endometrial glands + stroma
- ± hemosiderin

- What is adenomyosis?
- What are the histological changes?
- What is the clinical sign?

- Growth of endometrium in the myometrium
-
Histology:
- Enlarged, nodular myometrium with cysts
- Hemorrhagic cysts in functional endometrium
-
Clinical Signs:
- Abnormal uterine bleeding
- Infertility

What can cause endometrial disorders?
- hyperplasia
- prolonged/excess estrogen
What defines endometrial hyperplasia (4)?
- Exagerated endometrial proliferation
- Abnormal glandular architecture
- Increase gland/stroma ratio ( > 1:1)
- Nuclear atypia

What can lead to prolonged/excess estrogen (3)?
- Obesity
- Anovulation
- Estrogen producing tumors
What changes are seen in endometrial adenocarcinoma?
- Back to back glands
- Cellular atypia
- Abundant mitosis, including abnormal forms
- Necrosis

What are the risk factors for endometrial disorders?
- Obesity
- Diabetes
- Hypertension
- Infertility
- Exposure to unopposed estrogen
Is there a risk for adenocarcinoma if endometrial hyperplasia is present?
Yes
- 5% risk of progression to carcinoma in hyperplasia without atypia
- 20%-50% risk of carcinoma in hyperplasia with atypia
Type I Endometrial Adenocarcinoma:
- Endometrial hyperplasia association?
- Grade:
- Estrogen dependence?
- Progression:
- Mutation:

- In a background of endometrial hyperplasia
- Low grade endometrioid and mucinous adenocarcinoma
- Estrogen dependent
- Progression:
- Hyperplasia-carcinoma sequence
-
Mutation in Mismatch repair (HNPCC) ;
- tumor suppressor gene PTEN (Cowden syndrome)

Type II Endometrial Adenocarcinoma
- Association with endometrial hyperplasia?
- Mutation:
- Demographics:

- Usually in a atrophic background
- Independent of endometrial hyperplasia
- p53 mutation
-
Older women; more aggressive
- High grade endometrioidcarcinoma
- Serous carcinoma
- Clear cell carcinoma
- Carcinosarcoma
- Undifferentiated

What is also known as fibroids?
Leiomyoma
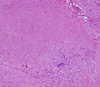
Leiomyoma
- Prevalence:
- Symptoms:
- Apperance:
- Pathogenesis:

-
Most common benign tumors in females (35%-50%)
- Blacks > whites
-
Asymptomatic, usually
- Abnormal bleeding
-
Sharply demarcated tumors
- Usually multiple
- Submucosal, intramural and subserosal
- Monoclonal proliferation of smooth muscle cells (bundles of benign smooth muscle)

What is the relation between leiomyoma and leiomyosarcoma?
**No relation**
Leiomyosarcoma
- Pathogenesis:
- Demographics:
- Appearance:
- Pathological Diagnostic Features:
- Recurrence and Metastasis?
- De novo from myometrialmesenchymal cells
- Post menopausal
-
Solitary
- Soft, hemorrhagic, necrotic mass
-
Pathological Diagnostic Features
- Tumor necrosis, cytological atypiaand mitosis (abnormal forms)
-
Recurrence and metastasis are common
- Pelvis, lungs, bones



