Exam 1 Flashcards
why are people with CVD given aspirin?
aspirin is COX inhibitor
PGH2 –> TXA2 (constrictor - produced by platelets) and PGI2 (dilator - produced by ECs)
PGI2 effects not taken out because ECs have nuclei
caldesmon
binds to actin filaments at low Ca conc. to prevent actin and muosin from interacting (preventing contraction)
doesn’t do it’s job when phosphorylated (is phosphorylated by MAPK)
what causes the water loss in the thin descending LOH?
the neighboring salt loss in the thick ascending LOH pulls water out of TDL into interstitum
(saltier the fluid means more Na is pumped out of the tubule)
systolic right heart failure (HFrEF)
myocardium can’t generate enough force to eject blood. breathlessness, large diliated heart
heart sound 3
2

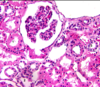
interlobular artery
which diuretic spares K loss?
amiloride (acts at collecting tubules)
channel is only Na so K not affected
autoregulation
how we maintain constant blood flow despite changes in pressure
what is the difference in generating activity induced flow in the brain vs everywhere else
neurotransmitters (espec. glutamate) rather than energy are the principal agents in generating activity induced flow
what is excitation coupling? what are the two types?
the process where excitation triggers an increase in calcium
-
electromechanical coupling: contraction WITH a change in membrane potential
- AP dependent - Ca channels open slower in SM
- graded depolarization - no AP generated/is resting potential
- pharmacomechanical coupling: contraction WITHOUT a change in membrane depolarization - usually caused by local tissue factors that open Ca ion channel or GPCR and depolarize membrane without AP
calsequestrin
Ca buffering molecule in the junctional SR
what does countercurrent mean?
fluid flows in opposite directions - down descending limb, up ascending limb
what are the steps of calcium excitation contraction?
- increase in calcium concentration (from AP)
- Ca binds to calmodulin (like troponin)
- Ca/calmodulin activates MLCK (myosin light chain kinase)
- MLCK phosphorylates and activates the myosin head ATPase activtiy
- ATP is cleaved and Pi is released resulting in confirmational changes
eccentric hypertrophy/dilation
HF thinning of wall; increases wall stress
heart sound 3
rapid blood flow from atria to ventricles (in kids). indicates CHF/Mitral regurg.
3

Collecting Duct
resitance compliance filter
what lets blood move through the CC even during diastole - guaruntees steady flow in capillaries
where does most of the Ca influx come from?
25% influx thru plasma membrane
75% Sarcomplasmic reticulum
pericyte
tight communication with ECs via gap junctions (in the brain). impacts phenotype to influence tightness of BBB - controls angiogenesis/vasculogenesis
whats the BFD about convective transport?
its the movement of blood around the body so diffusion can occur over short distances
1

PCT
how is the Ca transient increased?
by increased TIME to bind to troponin
NOT BY SUMMATION!
1

Macula Densa
=GFR
creatinine (inulin)
all of it is eliminated in the urine
- freely filtered at the glomerulus
- not reabsorbed
- not secreted
where is urea reabsorbed?
the collecting duct by vasopressin - puts VTA1 channels in the CT