Exam 1 Flashcards
(82 cards)
What are the bonds/forces of each level of protein structure?
- Primary structure: peptide bonds
- Secondary structure: H-bonding
- Tertiary structure: Cystine disulfide bridges (from two cysteines), hydrogen bonding, ionic interactions (salt bridges), hydrophobic forces
How do the oxygen-binding properties of HbF and HbA1 differ? Why is this important?
- HbA1 refers to the alpha2beta2 Hb tetramer, which is the most common form in adults, account for over 90% of total in blood - HbF is the predominant Hb tetramer present in the 2nd/3rd trimester of development. In contrast to adult Hb, HbF curve is shifted to the left indicating that at a specific o2 pressure, HbF is more saturated than adult Hb. Has higher affinity for o2 than adult Hb. This ensures that the fetus’ high metabolic o2 requirements are met. - This is due to the replacement of a histidine residue with a serine residue in the gamma chain of HbF. As a result, HbF has reduced affinity for 2,3-BPG and is left shifted.
Describe the 4 main groups of amino acids. What are their characteristics?
a.) non-polar, aliphatic: hydrophobic and chained/branched, found interior aspect of proteins, uncharged Gly, Ala, Val, Leu, Ile, Met, Pro • Gly – no asymmetric carbon (2 Hs) • Pro – ring structure • Met – sulfur-containing AA b.) aromatic: hydrophobic (non-polar rings), often found interior of water-soluble proteins, uncharged Phe, Tyr, Trp • Tyr – has OH group and can be phosphorylated c.) polar, uncharged: hydrogen bond, interior/exterior of proteins Ser, Thr, Cys, Asn, Gln • Ser/Thr – have OH groups that can be phosphorylated • Cys – sulfur-containing AA, forms disulfide bridges with other thiol containing molecules (ie. cystine = 2 cysteines) d.) Ionizable side chained AA – basic/acidic: Acidic: Asp, Glu (net -1 charge at physiological pH) Basic: Lys, Arg, His* (net +1 charge at physiological pH) * His can be basic/uncharged as pKa = 6.0
Explain what occurs to the Hb binding curve as pH, 2,3-BPG, temp, CO2 change? Draw it.

Define primary structure, secondary structure, tertiary structure, and quaternary protein structure.
a. Primary structure: the amino acid sequence of the polypeptide chain b. Secondary structure: a segment of polypeptide chain that has regular repeating structure. Results from H-bonding between the C=O and H-N groups of the polypeptide backbone. Alpha-helices and beta-pleated sheets. c. Tertiary structure: the 3D structure resulting from the interaction of various secondary structures and non-ordered regions of the polypeptide chain, results from disulfide bridges (covalent) and hydrogen bonding, ionic interactions (salt bridges) an hydrophobic forces (all non-covalent) d. Quaternary structure: protein molecules that have more than one subunit, each with tertiary structure, have overall quaternary structure. The subunits associate through same forces found in tertiary structures
Explain the biochemistry of CO (carbon monoxide poisoning).
- CO binds to heme iron at ~ 240 higher affinity than o2 (known as carboxyhemoglobin) - When 2 x CO molecules bind to Hb, R-form stabilizing, meaning T-form unfavored and o2 wants to remain bound and not deliver to tissue. - Treatment is removing individual from CO and administering 100% o2 at high pressure.
Describe the properties of HbS, the variant of hemoglobin found in sickle cell anemia.
- HbS is an altered Hb structure where a glutamate residue in the beta chain has been substituted for valine. Glu is a acidic hydrophilic AA, which valine is a non-polar, aliphatic AA. As a result, a “sticky hydrophobic pathy” is generated in the betal chains. When in the R-form, it is shielded from water. When in the T-form; however, it is exposed to surface. When in this form, it interacts with other Hb molecules to avoid interaction in polar environment and polymerization of poly Hb is catalyzed. This distores the shape of RBCs. Cells block blood vessels and damage organs.
What does the formation of hydroxyproline and hydroxylysine require?
-Fe2+, ascorbate and alpha-ketoglutarate in addition to enzyme.
What amino acid change occurs resulting in: (Explain each)
a. )HbS
b. )HbF
c. )Hbsaki/Hbgenova
- a.) Glu to Val. Valine residue is sticky when in T-form, polymerizes with other sticky residues.
- b.) His to Ser. Serine has decreased affinity for 2,3-BPG.
- c.) Val to Pro. Proline breaks alpha-helix resulting in unstable Hb molecule, unable to bind o2 (or decreased affinity?)
To what AA residue does 2,3-BPG bind on Hb? Result.
-His. Causes stabilization of T-form.
How can one experimentally distinguish between noncompetitive and irreversible inhibition?
- removal of irreversible inhibitor does not restore enzyme activity; however, removal of non-competitive inhibitor will restore enzyme activity.
What is the relationship between the magnitude of Km and enzyme/substrate affinity?
- inverse relationship - low Km = high S-E affinity - high Km = low S-E affinity - means some enzyme-substrates interact better than others
Explain what a competitive inhibitor is?
- A competitive inhibitor is a reversible inhibitor. These compete with substrate to bind at the active site on the enzyme. Increasing substrate concentration will prevent inhibitor binding. Infinite concentration of substrate will abolish inhibition. Inhibitor once removed will not affect enzyme functionality. - These are the most common type of drug
Describe and identify the reactions catalyzed by the following classes of enzymes: oxidoreductases, transferases, hydrolases, lyases, isomerases and ligases.
- a.) oxidoreductases: class I: catalyze redox reactions, involve electron acceptors / donors incl. oxidases, oxygenases, reductases, dehydrogenases - b.) transferases: class II: transfer groups (carboxyl, amino, glucosyl, phosphoryl, methyl etc.) from one substrate to another without the input of energy incl. kinases, aminotransferases, carboxylases, methyltransferases - c.) hydrolases: class III: cleave bonds by addition of water incl. glucosidases, ATPases, phosphatases, peptidases, lipases - d.) lyases: class IV: break bonds without addition of water or oxidative cleavage - e.) isomerases: class V: change steoreochemistry of optical or geometric isomers incl. epimerases, mutases, racemases - f.) ligases: class VI: catalyze formation of bonds via input of energy (usually via hydrolysis of XTP), not via transfer to bond incl. ligases, synthases, synthetases, carboxylases
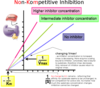
Explain what a non-competitive inhibitor is?
- A non-competitive inhibitor is a reversible inhibitor. These bind at sites on the enzyme other than the active site, forming inactive enzymes (E-I form or E-S-I). Increasing the concentration of the substrate does not influence inhibitor binding. It is reversible if the inhibitor can be removed. Enzyme will work after inhibitor removal.
What signaling cascades to Gs, Gi and Gq affect?
- Gs – stimulation of cAMP via adenylate cyclase
- Gi – inhibition of cAMP via adenylate cyclase
- Gq – stimulation of IP3/DAG via PLC
What are suicide substrates?
- Suicide substrates, aka Trojan Horse substrates, are special classes of irreversible inhibitors that only become inhibitors through the catalytic action of the target enzyme. They bind covalently at active site residues.
How does one determine the value of pKa to predict what form(s) a weak acid will predominate at, at a given pH?
The value of the pKa can help determine which forms of the acid will be dominant at a certain pH. When the pH=pKa the concentrations of acid and base are equal. When pHpKa the base form dominates.
Describe what happens at a molecular level when oxygen binds to a heme in deoxygenated hemoglobin. How do these events contribute to allosterism? How does the oxygen-binding behavior of hemoglobin translate into an efficient oxygen carrier?
Deoxygenated Hb is in a T-form (tight) with low o2 affinity. A valine reside partially blocks the o2 binding site in the beta subunits. When o2 concentration increases (ie. in lungs), o2 is forced by mere concentration onto alpha subunits. A conformational change occurs as a result of this binding and the valine residues are rotated out of the o2 binding site in the beta subunits. The Hb molecule is now in a high o2 affinity form known as the R-form (relaxed). The importance of this is considered when looking at the physiological range when o2 is loaded / unloaded from Hb.
Draw a substrate saturation curve and indicate Vmax, Km, Vmax/2.

Describe how the cAMP signal transduction system works. Include all the necessary players from activation to deactivation.
- cAMP, or cyclic AMP, is a secondary messenger. It is generated through the enzyme adenylate cyclase by converting ATP. - Gs proteins activate adenylate cyclase and cause rapid rises in cAMP levels. - cAMP acts as a secondary messenger by targeting protein kinase A (PKA, also known as cAMP-dependent protein kinase). It transfers gamma-phosphate groups from ATP to the hydroxyl groups of serine / threonine residues on the regulatory subunits, which cause conformational change and dissociation from the catalytic subunits, which then perform their specific downstream functions. - Deactivation of cAMP signaling: 1.) cAMP is hydrolyzed by cAMP phosphodiesterase to AMP and is no longer capable of activating PKA. 2.) intrinsic GTPase activity of G-protein returns protein to inactive states and adenylate cyclase is no longer activated. 3.) Hormone-receptor are no longer in active state (either internalized/degraded or inactivated by phosphorylation. 4.) Downstream enzymes phosphorylated by PKA are dephosphorylated by protein phosphatases and therefore are deactivated. - Gi proteins typically inhibit adenylate cyclase and cause rapid decreases in cAMP levels.
Describe how the determination of the 3-D structures of the isozymes of prostaglandin synthase aided in the design of drugs that selectively inhibit COX-2.
- NSAIDs act by inhibiting prostaglandin synthase, which are responsible for pain and inflammation. This enzyme has two enzymatic activities, one of which is cyclooxygenase activity and the other, hydroperoxidase. NSIADs inhibit the cyclooxygenase. Turns out there are two isozymes for this enzyme, COX-1 and 2. - COX-1 protects gastrointestinal mucosa, while COX-2 is associated with inflammation of arthritis. - As a result of this discovery, drugs have been designed specifically as inhibitors to COX-2. Eg. Celebrex, bextra and vioxx.
How is adenylate cyclase activated? Deactivated? Inactivated?
- Adenylate cyclase is activated by Gs proteins. Deactivated when Gs proteins are inactivated by their GTPase or when Gi proteins bind adenylate cyclase.
Describe how the IP3-DAG signal transduction system works. Include all the necessary players from activation to deactivation.
- Phospholipase C is activated by G-proteins (upon hormone/receptor binding) and hydrolyzes PIP2 (phosphatidylinositol 4,5 bisphosphate), a membrane lipid, generating two second messengers: IP3 (inositol 1,4,5 triphosphate) and DAG (diacylglycerol). - IP3 is water soluble and diffuses into cytosol where it binds to receptors on ER, triggering release of Ca2+ down its concentration gradient and into the cytosol. Ca2+ activates cytosolic protein kinase C (PKC) who have downstream effects. - DAG is liphophilic and remains membrane-associated, but easilty diffuses in the plane of the membrane. With Ca2+, it activates plasma membrane associated PKC. - Ca2+ released by the mechanism above can also bind calmodulin, causing it to interact with other protein kinases, phosphatases and ion channels. - Inactivation: 1.) receptor down-regulation/internalization/degration; 2.) protein phosphatases reverse action of PKC; 3.) Ca2+ pumped out of cytosol (into ER or to ECF); 4.) IP3 is dephosphorylated by phosphatase converting it into derivative that isn’t active; 5.) DAG is phosphorylated yielding phosphatidic acid or hydrolyzed to glycerol and FAs.