colorectal cancer Flashcards
epidemiology of colorectal cancer
major cancer in developed countries
4th most common cancer overall
2nd leading cause of cancer death overall
environmental (diet) factors and genetic factors are the aetiology
anatomy of the colon
caecum is hollow, large part of colon in R ileum
then have ascending colon
then hepatic flexure, transverse colon, splenic flexure, descending colon, sigmoid colon, rectum
in front of colon is the peritoneum
behind the colon is the mesentry where bv come in and out, it is fatty tissue
what is the function of the colon
extract water from faeces and therefore maintain electrolyte balance - therefore people with colorectomy become dehydrated - so gastroenterologists need to give them more water than normal and monitor electrolyte destrubances
is a faecal resevoir - this is an evolutionary advantage
bacterial digestion for vitamens especiall`y B and K
describe the structure of the colon
has mucosal surface folds
layers:
- area where the stool is
- epithelium (part of mucosa)
- lamina propria (part of mucosa)
- muscularis mucosa - thin layer of muscle
- muscularis externa
- submucosal
- muscularis propria - thick muscle
- fat and bv - this is the mesentry
- abdominal cavity
*

describe the colorectal crypt of lieberkuhn
have goblet cells that produce mucin - for immune function and lubrication
stem cells - constantly proliferating - move the cells up the crypt
mesenchymal cells are support cells - hold other cells in place

describe the colonic microanatomy
can see the lamina propria full of inflammatory cells
nucleus at the base of the cells and cytoplasm comes all the way up
below the nucleus have neuroendocrine cells

describe the turnover of colon cells *
a lot of turnover
proliferation renders cells vulnerable because that is the area where they are more likely to mutate
APC mutation prevents cell loss = mutation
normally there are protective mechanisms to eliminate genetically defective cells by natural loss of cells that are then replaced by normal cells, DNA monitors, repair enzymes that remove the damaged pieces of DNA and replace it
what is a polyp*
any projection from a mucosal surface into a hollow viscus and may be hyperplastic, neoplastic, inflammatory, harmartomatous etc
what is an adenoma *
a benign neoplasm of the mucosal epithelial cells - type of polyp
what are the colonic polyp types *
metaplastic/hyperplastic
adenomas
juvenille
peutz jeghers - familial disorder where get mucosal hyperpigmentation and polyps in GIT - can lead to higher risk of cancer
lipomas - benign growths of fatty tissue
others - any circumscribed intramucosal lesions
describe hyperplastic polyps *
very common
<0.5cm
90% of all lower intestinal polyps
often multiple
no malignant potential
15% have K-ras mutation
on histopath - still pink similar to normal, have serrated appearance

what are the different colonic adenoma types *
tubular when >75% adenoma is tubular - 90%
tubulovillous - 25-50% is villous - 10%
villous >50% is villous
flat - not polyp
serrated - similar to hyperplastic polyp but displastic
describe pedunculated and sessile adenomas *
pedunculated - means on stalk - A is intramucosal carcinoma that has not reached the musclaris propria; B has reached the muscularis propria it is invasive- but cutting stalk you can easily remove the adenoma
sessile adenoma - flat - more likely to spread into the muscle

what are the microscopic features of tubular adenomas *
columnar cells with nuclear enlargement, elongation, multilayering and loss of polarity (nucleus has moved to the lumen side of the epi)
increased proliferative activity - look at the mitotic count
reduced differentiation - how much look like normal colon
complexty/disorganisation of the architecture
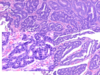
histopath of colonic adenoma *
more purple - increased nuclear material
nuclei look larger than hyperplastic
there is a loss of polarity

microscopic structure of villus adenomas *
mucinous cells with nucleus enlargement, elongation, multilayering and loss of polarity - these are signs of dysplasia
are exophytic frond-like extensions
may have hypersecretory function and result in excess mucus discharge and hypokalaemia - lose K into Gi tract because of mucin
small nucleoli
increased nucleocytoplasmic ratio

describe dysplasia *
means bad growth
abnormal growth of cells with some features of cancer
not invasive
there is subjective analysis - low, high or intermediate grade
describe the dysplasia

normal on R - relatively small nuclei on bottom and cells have plenty of mucin
low grade dysplasia on L - architecture still the same as normal
but nuclei are bigger, increased nucleocytoplasmic ratio, small nucleoli
describe this high grade dysplasia *
cells dont have normal architecture
high nucleocytoplasmic ratio
there is higher risk of it being carcinoma because of the high grade dysplasia
describe this high grade dysplasia *
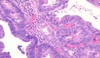
nuclei becoming big
back to back glands
describe the polyp *

Large villous adenoma with an ulcerated adenocarcinoma in its center.
describe adenomatous polyposis coli *
it is a mutation on 5q21
the site of mutation determines clinical variants
- classic - 100% sure will get colon carcinoma
- attenuated - less adenomas
- gardner - tumour in bone and skin
- turcot - tumour in brain - glioblastoma and blastoma
develop 1000s of polyps
many pts have a profylactic colectomy <30yrs
describe the natural history of colonic adenoma *
25% of adults have adenomas at age 50
5% of these become cancers if left
large polyps have higher risk than small - because there are more cells
lead time 10yrs - time from development of adenoma to development of carcinoma
cancers stay at a curable stage for 2yrs
describe the progression from adenoma to carcinoma *
most colon carcinomas (CRC) arise from adenomas
there is residual adenoma in 10-30% of CRCs
adenomas and CRC have similar distribution within the kidney
adenomas usually precede carcinomas by 10-20yrs
endoscopic removal of polyps reduces chances of CRC











