CHEMPATH: Clinical chemistry CPC Flashcards
Which of the following is associated with depression?
- Hyperkalaemia
- Hypokalaemia
- Hypercalcaemia
- Hypocalcaemia
- Uraemia
- Hypocalcaemia –> irritability and fits;
- Hypercalcaemia –> subtle tiredness, depression
Calcium, in general, affects the brain and nervous system
- Potassium affects heart before neurones –> heart becomes irritable –> arrhythmias (VF)
- As potassium rises, myocardium becomes more stable, however, the ultimate stable rhythm = asystole

- Answer:
-
Smith’s fracture = posterior displacement of the radius (i.e. radius** towards the **BACK of the hand)
- Falling on a flexed wrist
- Treated with manipulation under anaesthesia (MUA) and plaster
-
Smith’s fracture = posterior displacement of the radius (i.e. radius** towards the **BACK of the hand)
Other:
-
Colle’s fracture = anterior displacement of the radius (i.e. radius** towards the **PALM of the hand)
* Falling on an extended wrist- Pott’s fracture = ankle fracture involving both tibia and fibula
-
Colle’s fracture = anterior displacement of the radius (i.e. radius** towards the **PALM of the hand)

What do these results show?

Haematuria
What is the cause of massive haematuria in this patient? (with hypercalcaemia, depression, fracture and blood in urine)
- Renal stone
- Glomerulonephritis
- DKA
- Acute rheumatic fever
- Subacute bacterial endocarditis
Renal stones (or glomerulonephritis)
- Renal stones –> tear urothelium –> macroscopic haematuria
- Glomerulonephritis –> microscopic haematuria (not overt)
- DKA –> acidosis, ketonuria
- Acute rheumatic fever –> proteinuria (or normal)
- Subacute bacterial endocarditis à microemboli, microscopic haematuria, splenomegaly
How do you investigate calcified renal stones?
- Investigated with:
- Plain abdominal XR –> calcified stones (can be confused with gallstones)
- USS abdomen –> nephrocalcinosis

N.B. do plasma calcium before PTH because you need the calcium level to interpret any PTH level
List 3 causes of Ca2+ levels of 2.82.
- Cancer
- Primary HPT
- Sarcoidosis
If the PTH level is 3.0 (1.1-6.8 pM) and Ca is 2.82, what is the cause?
PTH is INAPPROPRIATELY high for the Ca level.
This is a normal level so malignancy and sarcoid would be excluded as the high Ca would suppress PTH.
- Sarcoid = PTH suppression/low (as produces lots of calcium which suppresses PTH)
- Cancer = PTH high (endogenous production) = from PTHrP or invading bone cancer
- 1st HPT = PTH normal/high (despite hypercalcaemia)
What are the actions of PTH?
PTH actions:
- Kidneys:
- Activate 1-alpha hydroxylase = vitamin D activation:
- Absorb calcium from gut
- Absorb phosphate from gut
- Directly resorb calcium
- Directly excrete phosphate
- Activate 1-alpha hydroxylase = vitamin D activation:
- Bone:
- Activate osteoclasts
What are the features and complications of hypercalcaemia?
Band keratopathy shown on eye

What are the different types of kidney stones?

What are the risk factors for renal calcium stones?
- Risk Factors:
- FHx
- Dehydration
- Hypercalciuria
- Hypercalcaemia
- HPT
- Recurrent UTI
How do renal stones present?
- Pain
- Haematuria
- Recurrent infections (Proteus mirabilis)
- Renal failure
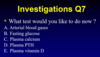
What Ix do you do for calcium renal stones?
- CT-KUB
- Stone analysis
- Urine and serum biochemistry
How do you manage renal stones?
- Most stones will pass –> painkillers:
- PR diclofenac is very good
- Lithotripsy
- Cystoscopy
- Lithotomy
How do you prevent renal stones?
- Drink more water
- Treat hypercalciuria (e.g. thiazides)
- Not in parathyroid adenoma –> hypercalcaemia (reduces calcinuria but increases serum Ca)
- Treat hypercalcaemia
How do you manage hypercalcaemia firstly?
Urgent treatment ([Ca2+] >3.0mmol/L ± unwell) – if calcium <2.8mmol/L, this doesn’t need to be as intense
-
FLUIDS –> IV 0.9% saline
- 4-hourly or 6-hourly bags of 1L 0.9% NaCl
- 1st bag of 1L given over 1 hour (if severely dehydrated)
- IV frusemide (prevent pulmonary oedema and aid calciuresis)
- MAYBE IV pamidronate (bisphosphonate), 30-60mg (if CANCER is the primary cause of the hypercalcaemia)
How is the primary hyperparathyroidism/hypercalcaemia managed in the long term?
- Well hydrated
- Avoid thiazides (reduce hypercalciuria but increase plasma calcium)
- Surgery (parathyroidectomy)
- Technetium Sesta MIBI and USS performed à shows hyperactive parathyroid
- If both tests concordant à whole neck does NOT need to be opened
- If tests not concordant à surgeon needs to view all four glands and take out the largest one
What does this bone histology show?

Brown tumours =
- multinucleate giant cells
- Activated osteoclasts in the bone
- long-standing undiagnosed HPT
What does the XR show in longstanding hypercalcaemia?
Radial cysic changes with longstanding hypercalcaemia (but initially normal)
NB: Looser’s zones are in longstanding Vitamin D deficiency/osteomalacia (needs to be very low). This is a pseudofracture.
What does this CXR show?

Bihilar lymohadenopathy
How does
Macrophages in the lungs express 1 alpha hydroxylase
Vitamin D leads to excessive calcium
Patients more likely to become hypercalcaemic in summer months because of increased exposure to sunlight
What is most increased in bloods in Paget’s disease? What about osteomalacia?
Alkaline phosphatase in bone (because increased osteoclast activity which release ALP)




