Case Studies in Cardiology Flashcards
What are some common etiologies of chest pain?
- myocardial ischemia / infarction
- pulmonary embolus
- pneumothorax
- pericarditis
- tamponade
- pneumonia
- aortic dissection
- gastritis,, peptic ulcer disease
- musculo-skeletal
- shingles (herpes zoster)
All chesst pain is what until proven othewise?
ischemic
What symptomatic featurs are specific to myocardial ischemia/infarction?
If a person comes in with one or more of these symptoms, what shoud you do?
- pressure-type of chest pain
- left-sided pain with radiation to jaw or arms
- exacerbatd by activity, relieved with rest
- relieved with nitro spray or sublingual
- nausea, diaphoresis (sweating to an unusual degree), syncope, shortness of breath
Do: enquirea bout cardiac risk factors
A decrease in BP indicates what complication associated with MI?
cardiogenic shock
An increase in JVP, pulsatile liver and peripheral edema indicates what complication associated with MI?
right-sided heart failure
Oxygen desaturation, croackles, S3 indicate what type of complication associated with MI?
left-sided heart failure
New murmurs can indicate what type of complication associated with MI?
mitral regurgitation can occur in papillary muscle dysfunction
If you suspect someone has an MI, what are work-up steps?
What are you looking for in these steps?
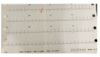
- EKG
- Chest X-ray to look for signs of congestive heart failure
- Cardiac enzymes
- CK (will begin to rise 6 hrs after infarct & remain elevated 24-48 hrs)
- troponin (will begin to rise 3-6 hrs after infarct & remain elevated 2 weeks)
- follow serially if first set is negative
What factors make up the “HEART” score & what does this score tell us?
What number is low risk?
if they should be admitted to the hospital
Low risk = 0-3
- History
- ECG
- Age
- Risk factors
- Troponin

What is the initial therapy for NSTEMI?
- M (morphine for the pain)
- O (oxygen if hypoxic)
- N (nitro SL/topical/IV for pain)
- A (Aspirin)
Describe the management strategy for NSTEMI
- Establish risk level usign a scorign system
-
low risk:
- may be discharged after symptom control
-
moderate risk:
- admit for further evaluation
- add B-blockers & ACE-inhibitors
- follow cardiac enzyme level
- if MI ruled out, exercise or adenosine stress test before discharge
-
high risk:
- admit for cardiac catheterization
-
low risk:
What is the management strategy for STEMI?
- Morphine, oxygen, nitro, aspirin
- beta-blocker, ACE-inhibitor
- early invasive strategy with either thrombolytic therapy or percutaneous coronary intervention (preferred)
What clinical features indicate a pulmonary embolism?
Risk factors?
- Clinical features
- sudden-onse sharp chest pain
- exacerbated by inspiratory effort
- associated - hemoptysis, syncope, dyspnea, calf swelling/pain from DVT
- anxious patient, sense of impendign doom
- tachycardia, tachypnea, hypoxia
- Risk factors
- immoblization
- fracture of limb
- post-operative complications
- hypercoaguable states
How can you diagnose a pulmonary embolism?
- EKG:
- sinus tachycardia
- S1Q3T3 (indicatd deep sections) with large embolus (classic, but rare)
- look for right-axis deviation
- V/Q scan very sensitive but not specific
- Spiral CT with contrast show large, central emboli
- Pulmonary angiogram is gold standard but carries risk
- Consider doppler U/S of legs
What is the typical clinical presentation of a pneumothorax?
What causes a pneumothorax?
- Clinical presentaiton
- Can be asymptomatic or present with acute pleuritis chest pain & dyspnea
- healthy, young, tall males
- Cause
- trauma (MVA, rib fracure, iatrogenic-medical treatment)
- increaed alveolar pressure from asthma or barotraumas (biPAP, ventilator-associated)
- rupture of bleb in COPD patients
What physical exam findings indicate a pneumothorax?
- decreased expansion of chest
- decreased breath sounds
- decreased tatile/vocal fremitus or side of pneumothorax
- hyperresonant percussion note
- usually easily confirmed by chest x-ray
Describe the typical clinical presentation of aortic dissection
Risk factors?
Diagnosis?
- Clinical presentaiton
- abrupt onset of ripping/tearing pain intrascapular area
- new diastolic murmur
- asymmetrical pulses, asymmetrical blood pressure measurements
- Risk factors
- hypertension
- Marfans
- coarctation of aorta
- Diagnois
- widened mediastinum on AP radiograph
- TEE is diagnostic test of choice
- b/c faster than CT


