Blood transfusion Flashcards
Why do we transfuse blood?
- For replacement of blood loss
- Failure of blood production
What differentiates the blood groups?
- Arrise from antigens
- (something that invokes immune response
- Red cell antigens are expressed on the cell surface
- Can provoke antibodies
How can we imagine ABO blood types?
Donuts and Sprinkles

What does ABO gene encode for?
Glycosyltransferase
These establish linkages: Glycans added to proteins or lipids on Red Cells
What do A and B genes code for?
Code for transferase enzymes:
- A antigen is N-acetyl-galactosamine
- B antigen is galactose
What does O code for?
- ‘O’ gene is non-functional allele
- So A and B are (co-)dominant and O is recessive
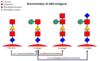
Which blood groups have antibodies against each other?
- If blood group A, have antibodies against B
- If blood group B, have antibodies against A
- If blood group O, have antibodies against A and B
- If blood group AB, have no antibodies against A and B
What does IgM do?
- anti-A/B naturally occurring
Percentage of different blood groups?
- A 42%
- B 9%
- AB 3%
- O 46%
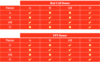
Which red cell vs FFP (fresh frozen plasma) blood groups can be administered to others?
Please see table:
What is RhD?
Either Rhesus negative or positive

What is notable about anti-RhD?
-
RhD negative individuals can make anti-D if exposed to RhD+ cells
- Transfusion or pregnancy
- Anti-D can cause transfusion reactions or haemolytic disease of the newborn
What do we cover for blood donors?
- Extensive ‘behavioural’ screening
- Sex, age, travel, tattoos…………
- Tested for ABO and Rh blood groups
- Screened for HepB/C/E, HIV, syphilis
- Variably screened for:
- HTLV1, malaria, West Nile virus, Zika virus…
What are the components of blood?
- Plasma (clotting, coagulation factors, albumin, antibodies)
- Buffy coat (Platelets, white cells)
- RBCs

What are 4 common indications for red cell transfusion?
- To correct severe acute anaemia, which might otherwise cause organ damage
- To improve quality of life in patient with otherwise uncorrectable anaemia
- To prepare a patient for surgery or speed up recovery
- To reverse damage caused by patient’s own red cells - Sickle Cell Disease
RBC
How do we store?
How long do we transfuse over?
Increments?
- Stored at 4 degrees
- Transfuse over 2-4hrs
- 1 unit increments ~5 g/L



