Block 2 Flashcards
The esophagus has what type of epithelium?
Stratified nonkeratinizing squamous
The stomach has what type of epithelium?
simple columnar epithelium
The ___ junction is defined as the point where rugal folds stop between the stomach and the esophagus
gastroesophageal junction (GEJ)
The ____ junction is defined as the mucosal junction between the stomach and the esophagus.
Also called the ___ line
Squamocolumnar junction (SCJ)
Z line
If the gastroesophageal junction and the squamocolumnar junction (Z line) so not occur at the same level, what disease may be present?
Columnar metaplasia –> Barrett’s esophagus
The respiratory system develops as a diverticulum on the ventral surface of the gut tube at the level of the ___ pharyngeal arch.
This diverticulum is called the ___ ___. Divides in the midline to create the lung buds.
4th
Laryngotracheal groove
Esophageal atresia (which normally occurs as proximal atresia with distal fistula to the trachea) results in ____ in the fetus, because the fetus is unable to swallow amniotic fluid.
The blind esophageal pouch may hypertrophy and compress/thin the trachea, called ____.
polyhydramnios
Tracheomalacia
infant presents immediately after food with choking or vomiting when feeding. Dx and what other abnormalities may be present?
Esophageal atresia
VACTERL: Vertebral anomalies, anal atresia, cardiac defects, tracheoesophageal fistula, renal defects, and limb defects
Alternatively, TACRD: tracheal agenesis/atresia, cardiac abnormalities, radial ray defects, duodenal atresia
Non-circumferential, thin pieces of tissue in the mid or proximal esophagus. Can be congenital or acquired, such as in iron-deficiency anemia (Plummer-Vinson Syndrome)
Mucosal webs
Circumferential, thick rings of tissue in the distal esophagus. Associated with hiatal hernia
Schatzki rings
Dx?
Esophageal, mucosal webs
Iron-deficiency anemia
Glossitis
Cheilosis
Dysphagia
Plummer-Vinson Syndrome
An outpouching of the esophageal wall above the upper esophageal sphincter, which tightens abnormally instead of relaxing when swallowing.
Food may collect, causing halitosis, regurgitation, extrinsic obstruction, and squamous cell carcinoma.
Reflects underlying motor dysfunction.
Esophageal/Zenker diverticulum
List a few causes of extrinsic esophageal obstruction
Mediastinal masses
Vascular compression (aortic aneurysm, etc)
Surgical changes (herniation, fibrosis)
Degeneration of the ganglion cells in the myenteric plexus of the esophagus.
Can be primary (at birth) or acquired (Chagas disease, diabetes, autoimmune).
The inability of the LES to relax after swallowing and lack of peristalsis. Results in periodic obstruction and eventual dilation proximally.
Dysphagia, odynophagia, regurgitation, and increased risk of squamous cell carcinoma.
Achalasia
A 40-yo physician returns from a trip with Doctors Without Borders in South America for 10 years. He suffers from dysphagia and weight loss over the last six months.
Achalasia secondary to Chagas disease
A patient presents with acute profuse bleeding following a night out drinking and vomiting this morning.
Mallory-Weiss tear at GEJ
A patient presents with acute profuse bleeding following a night out drinking and vomiting this morning. He suddenly develops trouble breathing and tachycardia.
Boerhaave’s Syndrome
An immunocompromised patient presents with an esophageal infection that stains as pseudohyphae.
Esophageal candidiasis
An immunosuppressed patient presents with an ulcerated esophagus. Ground glass intranuclear inclusions appear when cells from the periphery of the ulcers are placed on slides.
Herpes simplex esophagitis
An immunosuppressed patient presents with an ulcerated esophagus. Intranuclear and intracytoplasmic inclusions are visible when cells from the base of the ulcer are placed on slides.
Cytomegalovirus esophagitis
Patient presents with dysphagia and a feeling of food in the bottom of his throat. He has a 30 year history of excessive drinking and often eats acidic or fatty foods.
GERD
Dx?

GERD
erosive esophagitis seen as vertical linear streaks in the superficial mucosa
Top picture is normal. Dx the bottom picture.

GERD
Less surface maturation, basal cell hyperplasia, increases lamina propria inflammation, and papillae elongation
Columnar metaplasia with the addition of goblet cells can be defined as ____.
Intestinal metaplasia
Intestinal metaplasia and discontinuity of the GEJ/Z line together are dx for ____.
Barrett’s esophagus
Barrett’s esophagus increases the risk for what type of cancer?
Adenocarcinoma
A 15 yo male presents with dysphagia, which endoscopy shows as a food bolus obstructing his esophagus. He has a positive history of several childhood allergies, including pollen and nuts. His pH levels are testes and appear normal.
Dx and Tx?

Primary eosinophilic esophagitis (EE)
Elimination diet and corticosteroids
A 60 yo male patient presents with bleeding when coughing. He has a 35 year history of excessive alcoholism. His stomach appears distended with visible striae across the skin. What is the direct cause of the bleeding he is experiencing? Describe the pathogenesis.
Esophageal varices
Alcoholic cirrhosis > portal hypertension > esophageal varices, ascites, hemorrhoids, caput medusa
Abdominal organs shift upward through a defect in the diaphragm. May result in pulmonary hypoplasia.
Congenital diagphramatic hernia
Defect in the abdominal wall muscle that allows herniation of the abdominal contents into a ventral membranous (peritoneal) sac.
Omphalocele
Herniation of the abdominal contents through all layers of the abdominal wall, thus they are completely outside the body.
Gastroschisis
What is the diagnostic difference between an omphalocele and gastroschisis?
Omphalocele: contents within a membranous sac
Gastroschisis: no sac, contents outside of the body
A 4 week old make neonate presents with vomiting after feeding. The milk he expels contains no bile. A mass is palpable in the epigastric region of his abdomen.
Congenital hypertrophic pyloric stenosis
Alcohol, drugs (NSAIDS) or reflux result in foveolar hyperplasia with lack of inflammation.

Reactive (Chemical) Gastropathy
Abrupt onset of abdominal pain and bleeding associated with almost any etiology (alcohol, drugs, iron pills, radiation, etc.) that results in the breakdown of the mucosal barrier of the stomach.
Acute gastritis
NSAIDS contribute to acute gastritis mostly through what primary mechanism?
A. Recruitment of inflammatory cells
B. Inhibition of PG synth
C. Inhibition of bicarb secretion
D. Activation of acid secretion
B. Inhibition of PG synthesis
In turn, decreases bicarb and mucus secretion, which are secondary mechanisms.
Petechiae, erosions, and ulcers limited to the stomach mucosa. Neutrophils can also be seen.
Dx? Tx?
Acute erosive/hemorrhagic gastritis
Tx with acid suppression
1 cause of chronic gastritis, associated with PUD, MALToma and adenocarcinoma. Plasma cells in the lamina propria and neutrophils in the the epithelium/lamina propria.

H. pylori gastritis
Some strains of H. pylori have what toxin, which penetrates gastric cells and causes cell growth, gastritis, and adenocarcinoma.
cytotoxin-associated A (CagA) gene
Some strains of H. pylori promote B cell and T cell proliferation, which can result in ___?
lymphoma
H. pylori infection most commonly occurs in what area of the stomach?
Antrum
Results in gastric as well as duodenal ulcers
Anti-parietal cell and anti-IF factors result in the loss of parietal cells and the inability to absorb B12, limited to the body/fundus. Most commonly occurs in women.
Hypo or achlorhydria, increased gastrin (no negative feedback of HCl)
Degeneration of the spinal cord that cannot be corrected by folate supplementation.
B12 deficiency: Megaloblastic anemia, pancytopenia, peripheral neuropathy, CNS, and cardiovascular disease
Autoimmune gastritis
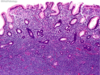
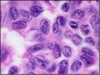
A patient has a gastric antral biopsy for abdominal pain, the slide of which is pictured. How does this organism survive in the acidic stomach?
A. Ammonia production
B. Hydroxide production
C. Bicarbonate production
D. Sulfate production

A. Ammonia production
H. pylori has a urase, which converts urea and water to CO2 and ammonia, which neutralizes gastric acid.
A 62 yo woman is diagnosed with autoimmune gastritis and pernicious anemia. Which of the following laboratory findings is most likely?
A. High vitamin B12
B. Hypergastrinemia
C. Elevated hematocrit
D. Low serum iron
B. Hypergastrinemia
Loss of parietal cells results in low acid secretion (elevated pH) which signals an increase in gastrin to re-stimulate parietal cell acid secretion.
[Low B12 (elevated methylmalonic acid and homocysteine) and megaloblastic anemia, serum iron should be normal]
Allergy or parasitic infection causes increased ___ in the lamina propria.

Eosinophils
Eosinophil gastritis
Increased intraepithelial lymphocytes in the surface foveolar epithelium. Associated with celiac disease.

Lymphocytic gastritis
Chronic infection

Granulomatous gastritis
Body and fundus-restricted hyperplasia of foveolar epithelium with hypoproteinemia. Loss of plasma proteins (albumin) through the gastric mucosa leads to peripheral edema. TGF-a overexpression. May occur after infection.

Menetrier’s Disease (hyperplastic gastropathy)
Diffuse hyperplasia of the fundic and body parietal cells in response to hypergastrinemia, usually a gastrinoma in the pancreas, duodenum, or antrum.
25% associated with MEN-1, 60-90% malignant.
Increased oxyntic mucosal thickness, so increased gastric acid.
Fundus > body affected
Duodenal ulcers and chronic diarrhea present clinically

Zollinger-Ellison Syndrome
Hereditary gastric cancer is associated with what mutation?
E-cadherin/CDH1 tumor-suppressor-gene
Loss of E-cadherin
What type of gastric cancer?
Wnt pathway mutation

Intestinal type
What type of gastric cancer?
Loss of E-cadherin
Diagnostic cells?
Diffuse gastric cancer
Signet ring cells

Enlarged supraclavicular node with gastric cancer
Virchow’s node
Enlarged periumbilical node with gastric cancer
Sister Mary Joseph’s node
Bilateral ovarian tumors metastasized from gastric cancer
Krukenberg tumors
___ Shelf due to metastasis of gastric tumors into Douglas’ pouch.
Blumer shelf
Mesenchymal tumor derived from interstitial cells of Cajal (pacemakers of the GI tract)

Gastrointestinal stromal tumors (GIST)
marker for gastrointestinal stromal tumors (GIST)
C-KIT, a tyrosine kinase
Most common primary gastric B cell lymphoma. Most commonly arises from chronic H. pylori gastritis. Treatment of infection can lead to tumor remission unless it has undergone genetic translocation.
Glands with intraepithelial lymphocytes and destruction of glands.
Gastric MALT lymphoma
Genetic mutation of gastric MALT lymphoma
t(11;18)
true (includes muscle) diverticulum of the ileum
failure of vitelline duct to involute (vitelline duct connects the developing gut to yolk sac)
Rule of 2’s
technetium-99m pertechnetate scintiscan scan
Image shows retained gastric mucosa, including chief and parietal cells

Meckel’s diverticulum
Causes of ____
herniation
adhesions
volvulus
intussusception
Small bowel obstruction
Most common cause of small bowel obstruction in children <2 yo
Intussusception
Acute vascular compromise that results in transmural necrosis in neonates when they begin oral feeding.
Form of ischemia
Distention, bloody stools, perforation and possible death
Especially in premie or low birth weight neonates (likely bowel immaturity)
Neonatal necrotizing enterocolitis (NEC)
AR disease of ion transport protein for chloride and bicarbonate across epithelial linings in the respiratory, GI and reproductive tracts
CFTR gene encodes the channel protein as well as inhibits ENaC (loss results in uncontrolled salt loss from the sweat ducts = salty skin and uncontrolled salt reabsorption from the other tracts, so mucous becomes dehydrated and thick)
Cystic fibrosis
Immune-mediated enteropathy triggered by foods containing gluten in genetically susceptible individuals
Association with other autoimmune diseases: HLA DQ-2, DQ-8
Gliadin digestion induces inflammation
Most sensitive test: anti-tissue transglutaminase IgA
Blunted villi = malabsorption

Celiac disease
Celiac disease is caused by a sensitivity to the products of gluten metabolism, particularly ____
Gliadin
All of the following are used to make a diagnosis of celiac disease EXCEPT:
a. anti-tissue transglutaminase Ab
b. anti-endomysial Ab
c. Anti-nuclear Ab
d. HLA DQ2 or DQ8
e. duodenal biopsy
C
Molecules in wheat, rye, and barley can cause symptoms but patients tests negative for celiac disease.
Amylase-trypsin inhibitors
FODMAPs (fermentable oligosaccharides, di-saccharides, mono-saccharides, and polyols)
Non-celiac gluten sensitivity (NCGS)
What is the main importance of differentiating celiac disease from NCGS?
Celiac disease increases the risk for adenocarcinoma. NCGS does not.
A 40yo man has a 5-year history of diarrhea, bloating, and crampy abdominal pain. He complains that his stools are “very greasy and very smelly.” He has similar symptoms as a child, but this resolved spontaneously after his mother starting banning processed foods in the house. In addition to his GI complaints, the patient complains of the following pruritic rash that is seen on his elbows below. What is the likely diagnosis?

Celiac disease
chronic diarrhea + processed food (gluten) + dematitis herpetiformis
Malabsorptive chronic diarrheal disease in regions with poor sanitation, likely bacterial, but compounded by poor nutrition which creates an impaired mucosal barrier in the gut. Malabsorption results in folate/B12 deficiency, megaloblastic anemia, failure to respond to oral vaccines, and early death.
Villous atrophy believed to affect the entire length of the bowel

Tropical sprue
A congenital or acquired deficiency that presents as the inability to digest lactose. Presents as bloating and flatulence after consumption of dairy.
Congenital: mt in lactase gene
Acquired: down-regulated lactase expression
Lactase deficiency or Lactose intolerance
AR disease that results in the inability to assemble TAG-rich lipoproteins due to a mt in a transporter. Thus, FFA accumulate within enterocyte cytoplasm. No apoprotein B in plasma.
Presents in infancy as diarrhea, steatorrhea, fat-soluble vitamin deficiencies, and lipid membrane defects (spikey RBCs, aka acanthocytes)

abetalipoproteinemia
Abetalipoproteinemia is associated with which hematologic abnormality?
a. schistocytes
b. sickle cells
c. acanthocytes
d. spherocytes
e. ringed sideroblasts
C
Infection with Tropheryma whipplei
Macrophages filled with organisms accumulate in small intestine lamina propria, mesenteric lymph nodes, joints, heart and brain.
Triad: diarrhea, weight loss, arthralgia
Villi are not blunted but are distended bt foamy macrophages
Tx: antibiotics

Whipple disease
Most common parasite in humans. Fecal-oral, usually rural streams or campers. Non-invasive but causes microvillus damage and apoptosis of intestinal epithelial cells. Asymptomatic to diarrhea. Most commonly seen in the duodenum.

Giardia
Parasite, fecal-oral, with increased prevalence in immunocompromised patients. The parasite resides in an endocytic vacuole within apical enterocyte cytoplasm (microvillus), although it appears to sit on top of the cell. Causes sodium malabsorption and chloride secretion –> watery diarrhea.

Cryptosporidium
Dx?

Hamartomatous polyps
(Peutz-Jeghers syndrome)
Dx?

Hamartomatous polyps
(Peutz-Jeghers syndrome)
Shows arborizing smooth muscle of the jejunum
Dx?
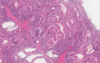
Hamartomatous polyps
(Peutz-Jeghers syndrome)
Shows arborizing smooth muscle + lobulated glands without dysplasia
Mucocutaneous pigmentation as typically seen in __?

Hamartomatous polyps
(Peutz-Jeghers syndrome)
Dx?
Intestinal obstruction (usually due to intussusception), abdominal pain, blood in the stool, prolapse of polyps through the anus, and mucocutaneous pigmentation.
Increased risk of cancers
AD germline mutation of STK11 (aka LKB1), a tumor suppressor gene.
Hamartomatous polyps
(Peutz-Jeghers syndrome)
Which embryological section of the GIT is most likely to present with aggressive tumors, rather than benign?
Midgut
Neuroendocrine tumor that presents as flushing, diarrhea, wheezing, pellagra, and cardiac disease
Carcinoid syndrome - Serotonin
A neuroendocrine tumor that presents as gastric acid hypersecretion (pain, ulcers, diarrhea)
Zollinger-Ellison Syndrome - gastrinoma
Neuroendocrine tumor that presents as neuroglycopenia, sympathetic overdrive, and obesity
Insulinoma
neuroendocrine tumor that presents as hyperglycemia, rash, anemia, hypoaminoacidemia, weight loss, thromboembolism, and glossitis
Glucagonoma
neuroendocrine tumor that presents as watery diarrhea, hypokalemia, achlorhydria, and other (hyperglycemia, hypercalcemia, and flushing)
VIPoma
Failure of neural crest cells to fully migrate from cecum –> rectum –> distal colon. Begins at anal sphincter and extends a variable distance proximally. Failure of peristalasis to travel full length of bowel; functional obstruction. Patient presents with failure to pass meconium in the first few days of life, followed by abdominal distention.

Hirschprung disease
aka congenital aganglionic megacolon
Barium enema. Dx?

Hirschprung disease
Most common form of congenital intestinal atresia. Failure of cloacal diaphragm to involute. Patient presents with failure to pass meconium and abdominal distention.
Imperforate anus
Commonly presents with other malformations - VACTERL
This a radiograph of a newborn taken after he failed to pass meconium and developed abdominal distention. A biopsy of his rectum is taken. What is the leading differential diagnosis?
a. imperforate anus
b. esophageal atresia with tracheoesophageal fistula
c. Hirschsprung disease
d. hypertrophic pyloric stenosis

a. imperforate anus
can also present with esophageal atresia and tracheoesophageal fistula, but that is secondary
Hirschprung presents as MEGAcolon
Chronic inflammatory condition resulting from dysfunctional mucosal immune activation. Usually presents in teens-20s in Caucasians and Ashkenazi Jews. Idiopathic but genetic elements? Also, research suggests epithelial defects in tight junctions, “leaky gut,” allowing microbial components to invade the lamina propria and trigger an immune response. An altered microbiome may also play a role.
Inflammatory bowel disease
Inflammatory (non-necrotizing granulomas) and ulcerative lesions that may present from mouth to anus, but tend to appear in the terminal ileum. Discontinuous lesions. Patient presents with diarrhea, fever, abdominal pain, and malabsorptive nutritional defects. Fistulae may also develop, signifying transmural involvement. Extraintestinal manifestations include uveitis and arthritis (other inflammatory processes), along with other autoimmune disorders. Increased risk of adenocarcinoma.

Crohn Disease
Inflammatory and ulcerative lesions limited to the colon and rectum in a continuous fashion, distal to proximal. Mucosal and submucosal inflammation only, so no fistulas occur. Active cryptitis, no granulomas. Patient presents with relapsing attacks of bloody diarrhea and abdominal pain relieved by defecation. Sometimes associated with primary sclerosing cholangitis (seen in women), and an increased risk of adenocarcinoma.

Ulcerative colitis
A 17yo male has abdominal pain with long-standing intermittent bloody diarrhea. All of the following findings from the physical and endoscopic examination would favor UC over Crohn’s EXCEPT:
a. perianal fistula
b. inflammation limited to the mucosa
c. inflammatory pseudopolyps
d. continuous disease from rectum to sigmoid colon
A. perianal fistula
Fistulas only occur with transmural necrosis, which is characteristic of Crohn’s not UC, which involved inflammation in only the mucosa and submucosa.
A 30yo female presents with abdominal pain for a few days at a time over the course of the last few months. The pain improves after defecation, and she has noted some changes in her stool. Biopsy shows no changes in her GIT.
Inflammatory bowel SYNDROME
Colitis in a portion of the colon excluded from the normal fecal stream (blind pouch). Diversion of the fecal flow deprived the diverted segment from the nutritional short fatty acid chains available in fecal material.

Diversion colitis
Tx: short FA enema
Idiopathic disease that is associated with celiac disease, autoimmune disease, drugs (NSAIDs)
Patient presents with watery diarrhea and normal findings on colonoscopy.
Biopsy shows two forms: lymphocytic or collagenous.
Microscopic colitis
Idiopathic disease that is associated with celiac disease, autoimmune disease, drugs (NSAIDs)
Patient presents with watery diarrhea and normal findings on colonoscopy.
Biopsy reveals intraepithelial lymphocytes, which prevent absorption water, leading to the watery diarrhea.

Lymphocytic (microscopic) colitis
Idiopathic disease that is associated with celiac disease, autoimmune disease, drugs (NSAIDs)
Patient presents with watery diarrhea and normal findings on colonoscopy.
Biopsy shows thickened subendothelial collagen layer.

Outpouchings of the colonic mucosa/submucosa, typically in the sigmoid colon (highest intraluminal pressure), which may become infected or inflamed. Incidence may increase in connective tissue disorders and is also higher in western countries with low fiber diets and the habit of sitting while defecating. Patient presents with lower left quadrant cramping, constipation or diarrhea, the sensation of never emptying the rectum.

Diverticulosis/diverticulitis
Acute inflammation of the appendix with neutrophilic infiltration and ulceration of the appendiceal wall, typically in children or young adults. Patient presents with periumbilical pain that later localizes to the RLQ.

Acute appendicits
Patient presents with acute abdominal pain, bloody diarrhea, vomiting, distention, and possibly death.
In adults, this is occlusion of a major blood vessel due to atherosclerosis, tumor, masses, volvulus, or shock.
In children, volvulus from malrotation.
The mucosa is most susceptible as it is furthest from the blood supply and presents as ulceration/atrophy through to normal submucosa or muscular layer.

Intestinal ischemia
Most common location of intestinal ischemia? Explain
Small/large intestine near the splenic flexure. The anastomosis of the super mesenteric artery and arcuate arteries/inferior mesenteric creates a watershed area.
Tortuous focus of mucosal and submucosal vessels, usually within the cecum/right colon. increased incidence with age.
Angiodysplasia
Swelling of internal or external perianal tissue due to persistently elevated venous pressure. Causes include straining at defecation, pregnancy, portal hypertension, and a sedentary lifestyle.

Hemorrhoids
Difference between internal and external hemorrhoids?
internal = transitional epithelium
external = squamous epithelium, frank blood, and itching or pain
Bacterial overgrowth due to longterm antibiotic use and the elimination of beneficial colonic flora. Toxin is released and causes loss of epithelial tight junctions, sloughing of epithelium, and watery diarrhea.

Pseudomembranous colitis (C. difficile)
Amebic cysts resistant to gastric acid are passed to the colon where they release trophozoites. If they invade the colon, they produce flask-shaped ulcers and bloody diarrhea. Fecal-oral transmission in countries with poor sanitation.

Entamoeba histolytics colitis
What is the major histologic clue to distinguish an acute from a chronic clolitis?
a. presence of neutrophils
b. presence of crypt architectural distortion
c. presence of lymphocytes
d. presence of mucosal granulomas
b. presence of crypt architectural distortion
see chronic crypt distortion below

Benign epithelial proliferation with no malignant potential. Commonly occurs in the LEFT colon. Crowding of epithelial cells, serrations and star shapes, but NO cytological atypia
Hyperplastic polyp
An inflammatory polyp typically seen in the rectum, resulting from impaired relaxation of the anorectal sphincter with recurrent abrasion. Thickened muscularis mucosa herniates upward into the mucosa, enveloping crypts.
Clinical triad: rectal bleeding, mucus discharge, inflammatory lesion of the anterior rectal wall

Mucosal prolapse polyps
An island od regenerating mucosa in a sea of ulceration, as commonly seen in ulcerative colitis.

Inflammatory pseudopolyp
AD inheritance of up to 100 hamartomatous colonic polyps. SMAD4 or BMPR1a mutation, upregulated cellular growth, mucosal hyperplasia. Most polyps within the rectosigmoid. Increased risk of cancer throughout the GIT, requiring endoscopic surveillance throughout their lifetime.
Globoid shaped polyp with many dilated, branching, mucin-filled cysts. May see stromal infiltration.

Juvenile polyposis syndrome
Cytologic dysplasia in the colon that is a premalignancy (precursor), and risk of progression directly correlates to size.
Dysplasia = enlarged, cigar-shaped hyperchromatic nuclei, pseudostratified
Can be sessile, pedunculated, and villous

Colonic adenoma
A type of polyp that most commonly occurs in the RIGHT colon and resembles a hyperplastic polyp but possesses malignant potential. Often MLH1 mutated, DNA mismatch repair gene. Architectural dysplasia but no cytologic dysplasia.
Seen below: crypt basal dilation (inverted T) and crypts growing horizontally.

Sessile serrated adenoma
Chromosomal instability pathway to colon cancer as seen in familial adenomatous polyposis (FAP), which accounts for approximately 75% of sporadic colorectal neoplasias. CIN+
APC/WNT
The pathway that leads to colon cancer as seen in Lynch Syndrome.
Microsatellite instability
A minor pathway to colon cancer that is CIMP+
Acquired CpG island hypermethylation
AD inheritance that all but guarantees colon cancer by 30yo. An inherited mutation in APC, a tumor suppressor gene that is a negative regulator of the Wnt signaling pathway. Additional mutations, such as KRAS or TP53, result in cancer. Also has extracolonic manifestations.

Familial adenomatous polyposis (FAP)
Most common cause of hereditary colon cancer. AD defect in one of several DNA mismatch repair enzymes: MLH1, MSH1, MSH6, PMS2. Leads to microsatellite instability –> rapid somatic mutations in genes that control tumor progression. Cancers occurring at younger ages than sporadic cancers. RIGHT sided. Extracolonic manifestations too.
Hereditary non-polyposis colon cancer (Lynch syndrome)
Malignant neoplasm of the colon with varying degrees of atypia. Atypical cells form glands with necrotic debris visible in the lumen.
Adenocarcinoma
Malignant neoplasm of the colon with >50% extracellular mucin
Occurring R side = L side
Can see debris floating within the mucin and lumen of atypical glands.

Mucinous adenocarcinoma
Malignant neoplasm of the colon that occurs in F>M and on the R side>L. Often defects in DNA mismatch repair and microsatellite instability. Islands of polygonal cells with prominent nucleoli, syncytial growth. Cells blend together and lose cell borders.

Medullary carcinoma of the colon
Adenocarcinoma can invade through the wall of the appendix, resulting in perforation. Seeding and spreading of tumor cells throughout the abdomen. Continued production of mucus by tumor cells fills the abdomen. Called ____ ____.
Presents as increased abdominal growth, inguinal hernia in men/ovarian mass in women, and can mimic appendicitis.
CT shows scalloping of liver and spleen and redistribution phenomenon.
Pseudomyxoma peritonei
Malignant neoplasm originating in the lower 2/3 of the anal canal.
F:M 2:1, but increased in young males with HIV. Increased in urban populations, alcohol/smoking, unprotected sex, immunosuppression.
Squamous cell carcinoma of anal canal
Exophytic papillomatous lesion os squamous epithelium associated with low-risk HPV strains.
Hyperkeratosis, parakeratosis, and koilocytes. Cytologic atypia is minimal, signifying low chance of malignancy with these strains.
Dx? Which strains are involved?

Condyloma acuminatum
HPV 6 and 11
HPV E6 blocks ___
HPV E7 blocks ___
p53 and Rb tumor supressor genes
Which zone of the liver?
Oxidative functions, e.g. gluconeogenesis, B-oxidation, and cholesterol synthesis. Deposition of hemosiderin in hemochromatosis.
Zone 1
Which zone of the liver?
Necrosis in yellow fever
Zone 2
Which zone of the liver?
Cytochrome P-450 based drug detoxification, glycolysis, and lipogenesis. Highest concentration of CYP2E1, so most sensitivity to NAPQI production in acetaminophen toxicity when all GSH has been spent.
Zone 3
Tx of acetaminophen overdose?
N-acetyl-L-cysteine which is processed by cells to L-cysteine and used in de novo synthesis of GSH, which is depleted in overdose. Detoxifies NAPQI byproduct of acetaminophen.
Bile moves (away/toward) the portal triad
Toward
(away from central vein)
Blood moves (away/toward) the portal triad
Away
(toward central vein)
(conj/unconj) bilirubin migrates to the brain of a newborn and causes severe neurological defects that are irreversible.
Unconj
(conj/unconj) bilirubin?
Tightly conjugated to serum albumin
Insoluble in water at physiologic pH
Cannot be excreted in urine
Increased in severe hemolytic disease or displacement from albumin
Unconjugated
(conj/unconj) bilirubin?
Loosely bound to albumin
Water-soluble, nontoxic
Excess is excreted in urine
Increase seen in alcohol abuse, infectious hepatitis, drug reactions, and autoimmune disorders. Liver obstruction.
Conjugated
decreased UDP-glucuronyltransferase (UGT1A1) activity
mild/self-limited
Treated by phototherapy (blue light coverts bilirubin to a soluble isomer)
Neonatal jaundice
AR inheritance that results in a complete lack of UGT1A1. Fatal secondary to kernicterus.
Crigler-Najjar syndrome type 1
AD inheritance that results in a partial defect in UGT1A1. Not fatal.
Crigler-Najjar syndrome type 2
Relatively common, but benign, decrease in levels of UGT1A1 that presents either asymptomatically or with mild jaundice related to increased stress (illness, menstruation, fasting, exercise, or medications)
Gilbert syndrome
AR inheritance that results in a defect in the bilirubin transport protein in bile canaliculi. Results in a darkly pigmented liver (conjugated bilirubin).

Dubin-Johnson syndrome
AR inheritance that results in a defect in the bilirubin transport protein in bile canaliculi. Does not show any liver pigmentation, but does show an increase in conjugated bilirubin.
Rotor syndrome
Systemic retention of conjugated bilirubin and other solutes eliminated in bile (bile salts, cholesterol, etc.) caused by hepatocellular dysfunction; intrahepatic or extrahepatic biliary obstruction. Patient presents with jaundice, pruritus, xanthomas, and elevated ALP and GGT.
Accumulation of bile pigment in hepatocytes, foamy degeneration of hepatocytes, distended bile ducts and lakes, portal tract fibrosis leading to cirrhosis.

Cholestasis
Complete or partial obstruction of the lumen of the extrahepatic biliary tree within the first three months of life. Fetal or perinatal forms. Due to inflammation and fibrosing stricture of the hepatic or common bile ducts. Elevated bilirubin but normal aminotransferase and ALP. Tx: transplant
biliary atresia
Acute massive liver destruction. Shrunken, soft with wrinkled capsule

Fulminant hepatitis
Most common cause of chronic liver disease, usually associated with alcohol abuse. Narrow to broad dense bands of fibrosis, regenerative parenchymal nodules, and entire liver architecture disruption. Leads to death via progressive liver failure, portal hypertension, and hepatocellular carcinoma.

Cirrhosis
Dx? Why?

Spider angioma
In liver failure, cannot metabolize circulation estrogens, causing increased levels in the blood. Also results in gynecomastia.
A complication of acute and chronic hepatic failure. Patient presents with marked stupor and confusion, deep coma and death. Neurological signs include rigidity, hyperreflexia, seizures, or asterixis (flapping tremor).
Hepatic encephalopathy
The appearance of renal failure in patients with liver failure. Associated with sodium retention, impaired free water excretion and decreased renal perfusion and GFR. Biopsy shows NO intrinsic causes of renal failrue. Renal failure improves if hepatic failure is reversed.
Hepatorenal syndrome
Increased resistance to portal flow resulting in ascites, congestive splenomegaly, portosystemic venous shunts - varices and hemorrhoids, and hepatic encephalopathy.
Portal hypertension
Apoptotic hepatocytes typically seen in acute hepatitis
Councilman bodies
(acute/chronic) hepatitis is characterized by lobular inflammation and hepatocellular injury. Inflammation contains predominantly lymphocytes and lobular infiltrate.
Ballooning degeneration, a type of cell death by enlarging and vacuolation
Acidophilic, hyaline bodies called Councilman bodies, which are apoptotic hepatocytes

Acute
(acute/chronic) hepatitis is characterized by dense portal inflammation, bridging necrosis and fibrosis. Ductular reaction in areas of fibrosis.
Highly variable clinical features, with fatigue being the most common
Few physical findings
May/may not see elevated PT, hyperglobulinemia, hyperbilirubinemia, and ALP

Chronic
Dx?
Benign, self-limited
Incubation 2-6 weeks
No chronic or carrier state
Spread by ingestion of contaminate food/water and shed in stool
IgM Ab
Hepatitis A
Acute or chronic hepatitis
Cirrhosis or fulminant hepatitis
Asymptomatic carrier state
Increased incidence of hepatocellular carcinoma
Incubation 4-26 weeks
Present in all body fluids and transmitted via IV drug use, sex, transfusion, etc.
DNA virus
HBsAg in overt disease/HBeAg signifies infectivity/IgM during window period/IgG in acute phase
Ground-glass hepatocytes in chronic inflection caused by an accumulation of hepatitis B surface antigen

Hepatitis B
RNA virus that is a leading cause of liver disease. Genomic instability makes vaccination difficult. Persistent infection is most common, and 20% progress to cirrhosis. Present in body fluids and transmitted via drug use or sex.
Hepatitis C
RNA virus dependent on HBV coinfection for multiplication. Can be an acute co-infection (self-limiting) or present as a superinfection in a chronic HBV carrier. Can cause acute hepatic failure.
Hepatitis D
Self-limited virus transmitted via fecal-oral route. Incubation 2-8 weeks and is NOT associated with chronic liver disease. High mortality among pregnant women
Hepatitis E
Hepatotoxicity with steatosis, inflammation (neutrophils), ballooning degenerations, Mallory bodies (ropey eosinophilic material in the cytoplasm), and fibrosis (sclerosing hyaline necrosis) leading to cirrhosis.
Large, yellow, greasy liver. Macrovesicular lipid globules. Causes increased lipid biosynthesis, impaired secretion, increased peripheral catabolism of fat. (all reversible is treatment is initiated).
Anorexia, malaise, weight loss, upper abdominal discomfort, tender hepatomegaly
Hyperbilirubinemia, increased ALP, neutrophilic leukocytosis, elevated ALT/AST

Alcoholic liver disease
Hepatic manifestation of a metabolic syndrome such as obesity, T2D, hyperlipidemia, or hypertension.
The presence of hepatic steatosis (macrovesicular) in individuals who do not consume alcohol or only in small quantities. Elevated serum transaminases, Mallory bodies and fibrosis. Increased risk of hepatocellular carcinoma. CV disease is a common cause of death.

Non-alcoholic fatty liver disease
AR defect in regulation of intestinal iron absorption due to a mutation in HFE gene –> deficiency of hepcidin. Acquired version is secondary to iron overload.
Deposition of hemosiderin in liver, pancreas, myocardium, skin, etc. Liver shows brown granular pigment, stains with Prussian blue. Also becomes cirrhotic. Pancreatic deposits are visible in islets.
Males >40yo
Hepatomegaly, abdominal pain, arrhythmia, arthritis
Bronze diabetes: cirrhotic hepatomegaly, skin pigmentation, and DM
Tx: phlebotomy

Hemochromatosis
AR inherited mutation in ATP7B gene that decreases ceruloplasmin, causing an increase in copper.
Liver: hepatitis then cirrhosis
Brain: deposits in basal ganglia
Eye: Kayser-Fleischer ring
Presents with liver disease and Parkinson-like symptoms
tx: chelation or Zn-based therapy
Wilson disease
AR mutation in PiMM –> PiZZ on chromosome 14. A1-antitrypsin is retained in cytoplasmic globules. Positive PAS stain. Common diagnosis in children. Results in cirrhosis in adults.
Associated with panacinar emphysema.
Magenta cytoplasmic granules, dilated endoplasmic reticulum with aggregates of misfolded protein
A1-antitrypsin deficiency
Childhood reaction to aspirin administration. Fatty change and encephalopathy (microvascular steatosis)
Reye syndrome
An autoimmune disorder associated with chronic cholestatic liver disease and antimitochondrial antibodies.
Nonsuppurative, granulomatous destruction of small and medium intrahepatic ducts (Florid duct lesion and non-necrotizing granulomas). Lymphocytic infiltration.
Women 40-50yo
Pruritis, later jaundice, and late cirrhosis

Primary biliary cirrhosis
Chronic progressive inflammatory destruction of the extrahepatic and large intrahepatic bile ducts.
M:F 2:1
Strong association with IBD and UC
Progressive! Fibrosis –> cirrhosis.
Increased incidence of cholangiocarcinoma
Chronic inflammation, necrosis, and eventual fibrosis. Onion skin fibrosis
“beading” - alternating areas of stricture and dilation of the extrahepatic and large intrahepatic bile ducts

Primary sclerosing cholangitis
Right sided heart failure causes congestion of the centrilobular sinusoids. ischemia –> centrilobular necrosis. Results in nutmeg liver. Can uncommonly cause cardiac sclerosis (centrilobular fibrosis).

Passive congestion
Patient presents with hepatomegaly, weight gain, ascites, and abdominal pain.
Associated with polycythemia vera or other myeloproliferative disorders, pregnancy, oral contraceptives, etc.
Severe centrilobular congestion and necrosis
High mortality if untreated
Hepatic vein thrombosis/ Budd-Chiari syndrome
Most common benign liver tumor
Appear as discrete red-blue, soft nodules, usually less than 2 cm in diameter
Consists of dilated vascular channels in a bed of fibrous connective tissue

Cavernous hemangioma
Gross: solitary, well-circumscribed mass +/- intratumoral hemorrhage
Micro: architecturally disorganized plates of well-differentiated hepatocytes. No bile ducts or portal tracts - Hepatocytes but NOT functional tissue
Rupture may lead to intraabdominal bleeding
Associated with oral contraceptives and anabolic steroids

Hepatic adenoma
Subtype of hepatic adenoma that increases risk for malignant transformation.
B-catenin
Most common primary cancer
Associated with B-catenin and loss of p53
M:F 8:1
Large, unifocal lesion which may be multifocal or diffuse
Well-differentiated hepatocytes arranged in cords or nests
Cholestasis
Can be caused by virus, cirrhosis, aflatoxins, etc.
Patient presents with silent hepatomegaly, elevated a-fetoprotein.
Death from cachexia, variceal bleeding or liver failure

Hepatocellular carcinoma
2 mutations that increase susceptibility for hepatocellular carcinoma
B-catenin and p53
Primary cancer arising from the biliary tree. Incidence higher in china and associated with the Opisthorchis sinesis liver fluke

Cholangiocarcinoma
Primary cancer associated with polyvinyl chloride, arsenic, and thorotrast exposure
Angiosarcoma
Mass lesions in the liver are more commonly (hepatic/metastatic)?
Hepatic
Doubel vagina or double uterus result from developmental anomalies in the fusion of ____ ducts and absorption of the septum.
Mullerian
Impaired fusion of the Mullerian ducts that manifests as double uterus and double vagina
Double vagina presents as dysmenorrhea and dyspareunia
Bicollis
Impaired fusion of the Mullerian ducts that manifests as double uterus and single vagina
A congenital malformation characterized by incomplete development or agenesis of the Mullerian duct, causing the uterus and the upper two-thirds of the vagina to be underdeveloped or absent, although external genitalia are normal.
Primary amenorrhea and may be associated with other organ anomalies.
Mayer-Tokitansky-Kuster-Hauser Syndrome (MRKHS)
Persistence of small patches of glandular epithelium (from the endocervix) in the vagina. There are normally NO glands in the vagina. Occurs when the female fetus is exposed to diethylstilbestrol in-utero. Can lead to an increased risk of clear cell carcinoma

Vaginal adenosis
Vaginal adenosis increases the risk of this type of cancer

Clear cell carcinoma
Vaginal infection associated with diabetes, antibiotics, and immunosuppression. Appears as white plaques, red base. Pseudohypahe and spores.

Candidal vulvovaginitis
STD that is typically asymptomatic. Vaginal and cervical mucosa are erythematous and speckled with foci of dilated capillaries.

Trichomoniasis
STD, gram-negative bacterium. Replicates only within host cells. Usually causes urethritis, cervicitis, blindness in vertical transmission to newborn, lymphogranuloma venereum and pneumonitis. Infeection may ascend to the uterus and fallopian tubes, resulting in PID and possible sterility.

Chlamydia trachomatis
STD, vesicles –> inflammation –> ulcers. Multinucleated epithelial cells with nuclear molding, intranuclear inclusions. High risk of vertical transmission during delivery.

Genital herpes simplex virus (HSV2 > 1)
Chancroid (soft chancre)

Haemophilus ducreyi
Hard chancre, condylomata lata

Primary syphilis
Granuloma inguinale, destructive lesions. Donovan bodies are rod-shaped, oval organisms in the cytoplasm of the host cell.

Klebsiella granulomatis
Water warts, STD. Poxvirus, DNA enveloped. Skin and mucous membrane infection commonly in sexually active adults or immunocompromised patients. Highly infectious on skin, toys, etc. Can autoinoculate other locations on the same patient. 6 week incubation. Papule with central umbilication or cheese-like matieral. Intracytoplasmic inclusion and epidermal hyperplasia.

Molluscum contagiosum
Ascending bilateral infection of the uterus and fallopian tubes, usually including pelvic peritonitis. Caused by some STDs. Can result in infertility, ectopic pregnancy, pain, intestinal obstruction, and liver capsule adhesions (Fitz-Hugh-Curtis Syndrome).
Pelvic inflammatory disease
Any white plaque on the vagina
Leukoplakia
Benign mesenchymal growths
Simple fibroepithelial polyps (skin tags)
Benign exophytic lesion caused by low grade HPV serotypes.
Dx? Which serotypes?
Condyloma acuminata
HPV 6 and 11
Decreased estrogen, typically in older age, causes ___ of the vagina, urethra, and bladder mucosa. Shortening and tightening of the vaginal canal, lack of secretions. Inflammation is secondary. Symptoms: dyspareunia, UTI, incontinence, spotting after intercourse, pain with intercourse.
atrophy
Chronic lymphocyte-mediated skin disease with probable autoimmune etiology. Typically in post-menopausal women. Can increase the Irish of squamous cell carcinoma and requires lifetime surveillance. Smooth white plaques, epidermal atrophy, dermal fibrosis with lymphocytic infiltrate beneath.

Lichen sclerosus
Changes in epithelium secondary to chronic irritation/scratching to relieve pruritus. Low risk of developing squamous cell carcinoma of the vulva. Marked hyperplasia, hyperkeratosis, +/- lymphocytic infiltration. No atypia. Atopy - the genetic tendency to develop allergic diseases such as allergic rhinitis, asthma, and atopic dermatitis.

Squamous cell hyperplasia (lichen simplex chronicus)
The intraepidermal proliferation of malignant epithelial cells, usually in the vulva. The primary format arises from epidermal progenitor cells, not an underlying malignancy, but it does have to potential to spread and progress into an invasive tumor. Red, scaly, crusty lesions (“cake-icing scaling”) mimicking other inflammatory dermatoses. Often multifocal. Large malignant epithelioid cells in the epidermis, pale granular and/or vacuolated cytoplasm. PAS stains mucin pink.

Extramammary Paget Disease
Rare primary vaginal tumor, usually in infants and young children, composed of malignant embryonal rhabdomyoblasts. Presents as polyploid grape-like lesions composed of small cells with a superficial crowded “cambium” layer. Tends to invade locally and can metastasize. Immature skeletal muscle tumor, +Desmin, +myogenin.

Embryonal rhabdomyosarcoma of the vagina
Cross striation like skeletal muscle seen in a vaginal tumor

Embryonal rhabdomyosarcoma
Keratinization typical of what kind of cancer? Here, in the cervix. Mostly related to infection with high grade serotypes of HPV. Microscopic to exophytic tumors.

Squamous cell carcinoma
Glands typically present in what part of the female anatomy?

endocervix
Most common cause of abnormal uterine bleeding during reproductive age
Anovulatory cycles
Most common cause of heavy bleeding
Bleeding disorder - ie. von Willebrand’s disease
Nine categories of abnormal uterine bleeding
PALM-COIEN
Polyps, Adenomyosis, Leiomyoma, Malignancy - Coagulopathy, Ovulatory disorders, Endometrial iatrogenic, NOC (other)
Infection in the uterus commonly caused by retention of gestational tissue, PID, IUDs, or TB.
Many plasma cells are seen

Chronic endometritis
A nonneoplastic lesion of the myometrium characterized by the presence of endometrial glands and stroma within the myometrium, in continuity with the endometrium. An asymmetrically enlarged, globular uterus. Trabeculated, cut surface with ill-defined hypertrophic swirls of smooth muscle and petechiae-like gray or hemorrhagic foci in the endometrium. The glandular tissue is usually inactive. Presents as menorrhagia, dysmenorrhea, and pain. Often associated with endometriosis.

Adenomyosis
Presence of endometrial glands and stroma outside of endometrium. Often coexists with adenomyosis and is multi-focal. Presents as chronic pain, dysmenorrhea, infertility. Increased levels of inflammatory mediators, including PGE2 and abnormal estrogen. PGs increase estrogen which increases gland and stromal proliferation. This in turn increases cytokines and inflammation. Increased risk of ovarian and uterine cancers.
Functional glands bleed with each cycle. May form coalesced cysts. Fibrosis and scarring create adhesions and infertility.

Endometriosis
Normal gland to stroma ratio in the endometrium
2:1
Endometrial proliferation with increased gland to stroma ratio (3:1). Crowded, abnormally shaped glands. Can be simple, complex, typical, or atypical. Causes abnormal uterine bleeding and an increased risk of endometrial cancer.
Caused by an excess of estrogen relative to progesterone, which can be from exogenous or endogenous sources. PTEN mutation may also be present, resulting in the increased risk of cancer.

Endometrial hyperplasia
Mutation in endometrial hyperplasia that causes an increased risk of cancer
PTEN
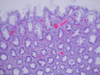
Classify this endometrial hyperplasia

Simple hyperplasia without atypia
Classify this endometrial hyperplasia

Complex without atypia
Classify this endometrial hyperplasia

complex atypical
Benign, sessile mass lined by epithelium on three sides. May protrude into the endocervical canal. Glands can be inactive or active. Fibrous stroma often with thick-walled and/or dilated blood vessels. Smooth muscle occasionally present.

Endometrial polyp
Benign growth composed of a fibrovascular core and normal or malignant squamous epithelium. Sessile or polyploid, often protrude through the cervical os. Glands surrounding loose myxoid stroma. May lead to bleeding.

Endocervical polyp
Type 1 or 2 endometrial cancer?
60yo, obese or excessive estrogen:progesterone, hyperplastic endometrium. Endometroid type. Hyperplasia is a precursor. PTEN mt. Indolent course.
Closely resembles normal endometrium. Types include mucinous, tubal, squamous, and adenosquamous

Type 1 aka endometroid adenocarcinoma
Type 1 or 2 endometrial cancer?
70 yo, thin physique, atrophic endometrium. Serous morphology. Intraepithelial carcinoma is precursor. TP53 mt, but a mt in PTEN is also commonly seen. Aggressive course.
Forms small tufts and papillae, with marked cytologic atypia.
Includes clear cell and mixed Mullerian types.

Type 2 aka serous endometrial carcinoma
Endometrial adenocarcinoma with a malignant mesenchymal component, which may be homologous or heterologous (tissues abnormal to the uterus). Post menopausal and poor prognosis.
Gross: bulky, polyploid, fleshy
Seen here with heterologous cartilage

Malignant mixed Mullerian tumor (MMMT) aka carcinosarcoma
Genes fused in stromal endometrial sarcomas
JAZF1 and polycomb factor genes such as SUZ12
A benign smooth muscle tumor, often multiple. Most common uterine tumor in reproductive age. More common in African-Americans. Monoclonal tumors often with rearrangements in chromosomes 6 and 12. Estrogens and contraceptives stimulate growth, therefore usually shrink after menopause. Present with heavy bleeding and a dragging sensation but are often asymptomatic. Major cause of infertility.
Bundles of smooth muscle cells, often mixed with fibrosis or calcification. No atypia.

Leiomyoma aka fibroids
Chromosomes involved in the development of leiomyomas
6 and 12
Single tumors in the uterus. De novo and postmenopausal. Recurrence and metastasis are common. Gross: soft, fish-flesh cut surface, hemorrhagic, necrotic, with irregular outline. Atypia is seen. + desmin and smooth muscle actin. - myogenin.

Leiomyosarcoma
Inflammation of the fallopian tubes commonly caused by gonococcal or chlamydial infection and PID. TB is a rare cause.
Neutrophilic infiltration

salpingitis
Most common site of an ectopic pregnancy
Fallopian tube
____ fallopian tube cyst from Mullerian duct remnants

Paratubal
____ fallopian tube tumors can be solid or multicystic. Benign, mesothelial origin, subserosal. In males, also found in the epididymis and testis

Adenomatoid
Serous carcinoma in the fallopian tube can extend to the ovary or peritoneum. It is associated with what mutation?
BRCA
Intrauterine adhesions or in the endocervix with risk of hypomenorrhea/amenorrhea, reduced fertility, miscarriage, and abnormal placentation. Usually results from pregnancy-related curettage that damages the basal layer of the endometrium. Can also be related to infection or uterine surgery.
Asherman’s syndrome
The collapse of the uterus due to weakened fibromuscular walla. Increased by vaginal delivery, force delivery, and age. Results in voiding dysfunction or obstructed defecation
Prolapse
45, XO, pure monosomy or mosaic. The most common sex chromosome abnormality in females. Hypogonadism due to accelerated loss of oocytes from the ovaries after 18 weeks of fetal life, leading to steak ovaries (fibrotic). “Menopause before menarche.” Most common cause of primary amenorrhea.
Turner syndrome
Difference between a cystic follicle and a follicular cyst.
<3 cm = cystic follicle
>3 cm = follicular cyst
Complete or partial rotation of the ovary on its ligamentous supports. Can be a complication of a cyst or mass. Ovarian artery and vein within the suspensory ligament are obstructed –> infarction.
Ovarian torsion
If tube also twisted = adnexal torsion
Endocrine disorder characterized by hyperandrogenism, ovulatory dysfunction and cysts. Most common cause of anovulatory infertility. OHIO: oligomenorrhea, hirsutism, infertility and obesity.
Caused by excessive androgen production by ovarian theca cells due to a variant DENND1A gene.
Increased BP, HDL low, TAGs increase, sugars increased
Polycystic ovarian syndrome (PCOS)
variant gene in PCOS
DENND1A
Most common ovarian epithelial tumor
Malignancy increases with age
CA-125 tumor marker used to monitor but not to screen, as it is present in other conditions. May be BRCA associated. May be seen in Lynch syndrome.
Includes 3 types: cystadenoma, borderline and carcinoma
Ovarian serous tumors
Tumor marker for ovarian serous tumors
CA-125
Type of ovarian serous tumor
Gross: thin walls, filled with clear serous fluid, smooth inner surfaces with occasional papillary projections
Micro: a single layer of tall columnar epithelial cells, which are often ciliated. No/little atypia.

benign serous cystadenoma
Type of ovarian serous tumor
Gross: increased papillary projections, filled with clear serous fluid.
Micro: lining cells show nuclear atypia, nuclear stratification and cellular buds. No stromal invasion.
Good prognosis but may recur.

Borderline serous tumor
Type of ovarian tumor
Usually high grade with complex architecture and nuclear atypia. Develop rapidly from serous tubal intraepithelial carcinoma (STIC), usually in the fimbriae of fallopian tubes.
BRCA+ and tp53
(Low grade KRAS or BRAF)
Gross: solid and cystic mass with necrosis and hemorrhage.
Micro: stromal invasion. Nuclear atypia. Papillary or solid structure. Psamomma bodies

Serous carcinoma (serous adenocarcinoma)
____ ____ are calcifications seen in the tips of papillae of serous carcinoma
Psamomma bodies
Ovarian tumors with >50% intracellular mucin. Small amount of extracellular mucin. Usually benign, but 10% malignant.
KRAS associated
Malignant tumors show solid areas, serosal penetration, architectural complexity, atypia, invasion. Bilaterality increases the likelihood of malignancy.
Extensive mucin secretion can lead to pseudomyxoma peritonei.
Includes 3 types: cystadenoma, borderline, and carcinoma
Ovarian mucinous tumor
mt associated with ovarian mucinous tumor
KRAS
excessive mucin secretion from ovarian mucinous tumors can lead to ___ ___ ascites.
pseudomyxoma peritonei
Bilateral ovarian mucinous tumors are typically malignant, such as ____ tumors metastasized from where?
Krukenberg tumor
GIT
Solid or cystic tumor of the ovary. May be associated with endometriosis. Tubular glands, similar to the endometrium. May be benign or borderline, but are usually malignant. Associated with mutations in PTEN, MSI, KRAS, and B-catenin.
Variant type is clear cell adenocarcinoma

Endometrioid carcinoma of the ovary
An uncommon, solid tumor of the ovary. Abundant stroma containing nests of transitional epithelium similar to that in the urinary tract along with coffee bean nuclei. Occasionally nests are cystic and mucin-secreting. Very variable in size. Usually benign but borderline and malignant types also occur.

Brenner (Transitional cell) tumor
What are the four long-term consequences of PCOS?
ECDM - Every cyst doesn’t matter
Endometrial cancer, CV disease, Diabetes T2, Metabolic syndrome
A tumor arising from more than one germ cell line, therefore show 46 XX genotype (in women).
Teratoma
A tumor arising from more than one germ cell line. See in prepubertal and young women. Bulky, predominantly solid, areas of necrosis and hemorrhage. The presence of immature and atypical neuroepithelial tissues differentiates it as malignant.
Immature/ Malignant teratoma
A tumor arising from entirely or mostly thyroid tissue, present in the ovary. May produce hyperthyroidism or thyroid carcinoma.

Struma ovarii
Tumor producing serotonin in the ovary

Ovarian carcinoid
tumor in ovary that contains both thyroid tissue and serotonin producing cells.
Struma carcinoid
Ovarian tumor arising from primordial germ cells. Some occur with gonadal dysgenesis, including Turner syndrome. Elevated LDH and may rarely produce chorionic gonadotropin (if syncytiotrophoblasts are present).
Nests of uniform polygonal malignant germ cells with clear or eosinophilic cytoplasm and squared off by distinct cell membranes, surrounded by fibrous bands. Typically with many small benign reactive T cells.
+PLAP

Dysgerminoma
Tumor marker for dysgerminoma

Placental alkaline phosphatase (PLAP)
Ovarian tumor usually occurring in children or young adults.Increased alpha fetoprotein and alpha-1-antitrypsin. hCG negative. Schiller-Duval bodies: layers of endothelial cells surrounding a capillary.

Yolk sac (endodermal sinus) tumor
Tumor markers for yolk sac (endodermal sinus) tumor
(2)
alpha fetoprotein
a-1-antitrypsin
layers of endothelial cells surrounding a capillary as commonly seen in yolk sac (endodermal sinus) tumors

Schiller-Duval bodies
Rare ovarian tumor. The most aggressive form of germ cell tumor. Presence of syncytiotrophoblasts, cytotrophoblasts, and intermediate trophoblasts with an absence of chorionic villi. Usually mixed with other germ cell types. High levels of hCG.

Ovarian non-gestational choriocarcinoma
Ovarian tumor that occurs typically postmenopause. Cuboidal granulosa cells in cords, sheets with spindle or plump, lipid-laden theca cells. Granulosa cells may form Call-Exner bodies (shown), recapitulating ovarian follicles. These show coffee bean nuclei with folds/grooves. +Inhibin
Increased estrogen causes precocious puberty and predisposes patient to endometrial and breast cancers

Granulosa cell tumors, adult ype
Tumor marker for granulosa cell tumors
Inhibin
____ bodies formed in granulosa cell tumors.
Call-Exner
An ovarian tumor that grossly appears solid, white. Composed of spindle cells (fibroblasts) with collagenous bands of stroma. Not hormonally active

Fibroma
Ovarian tumor that grossly appears yellow due to increased intracellular lipids –> vacuolated cells. May be hormonally active

Thecoma
An ovarian tumor with both fibroblasts and increased intracellular lipids. Most are hormonally active.
Increased estrogen, ascites, pleural effusion and Meia’s syndrome.
Fibrothecoma
Ovarian tumor in all ages, but especially young adults. Composed of sex cord (Sertoli cells) and stroma (Leydig cells). May occur sporadically in patients with DICER1 syndrome. Produce androgens and masculinization of the female patient. Shown below well-differentiated.

Sertoli-Leydig cell tumor (androblastoma)
Marker for myoepithelium of breast tissue. The presence of epithelium and myoepithelium (2 layers) signifies that a tumor is benign.

p63
Age of the patient with the breast tissue shown
Radiodense, making detection of dense tumors difficult.

Young
Age of the patient with the breast tissue shown?
Branching of terminal ducts

Pregnancy
Age of patient with breast tissue shown?
Radiolucent makes detecting radiodense masses easy.

Older age
Lobules decrease in size and number.
Tumor?
Lobular architecture is maintained with no malignant cytologic features

Benign pregnancy-related lactating adenoma
Infection that arises within the first few weeks of nursing. The breast appears swollen, red, and diffusely tender. When advances, can become localized, soft, fluctuant swelling abscess. Single or multiple abscesses. Typically staph aureus, but rarely Strep group A.

acute mastitis
___ ___ of lactiferous ducts is common in smokers. When it extends deep into the nipple, keratin becomes trapped and accumulates. If the duct ruptures, the ensuing intense inflammatory response to keratin results in an erythematous painful mass. A fistula may form between the smooth muscle and the areola.
Squamous metaplasis
Nonbacterial chronic inflammation of the breast seen in elderly women. Associated with thick-white or brown nipple discharge.
Duct obstruction and dilation –> rupture –> periductal chronic inflammation with a preponderance of plasma cells and lymphocytes and dense fibrosis.
Must differentiate from invasive carcinoma

duct ectasia
A response to breast trauma or surgery –> granulomatous inflammation with a large number of lipid-laden (foamy) macrophages, multinucleated giant cells and increased fibrocollagenous tissue –> indurated mass formation mimics carcinoma.
Resolving areas show fibrosis –> sclerosis –> dystrophic calcification

Fat necrosis
The lumen of a breast duct is filled with heterogeneous, mixed population luminal and myoepithelial cell types. Irregular fenestrations are prominent at the periphery.
Type of proliferative fibrocystic change without atypia

Ductal hyperplasia
Type of proliferative fibrocystic change without atypia
Benign lesion in perimenopausal women. Presents with bloody nipple discharge.
Within dilated lactiferous ducts, branching finger-like projections lines by two later of epithelial cells. Central, fibrous core. Epithelial hyperplasia and apocrine metaplasia are frequently present.

Intraductal papilloma (benign)
Type of proliferative fibrocystic change without atypia
Proliferation of small duct epithelial cells
Proliferation of myoepithelial cells
Increased intralobular stroma
Sclerosing adenosis
Type of proliferative fibrocystic change without atypia
Complex proliferation of small duct epithelial cells and myoepithelial cells with increased intralobular stroma. Papillomas and complex epithelial hyperplasia. Radial scar.
Complex sclerosing lesion
Proliferative fibrocystic changes WITH atypia
Clonal proliferation with all the features of carcinoma but are reversible
Two types: ductal or lobular
May have chromosomal changes such as 16q or 17q
Atypical hyperplasia
Atypical ___ hyperplasia shows mixed population of cells consisting of oriented columnar cells at the periphery and rounded cells within the central portion. Central spaces are rounded but peripheral spaces are irregular and slitlike. Highly atypical features.

Ductal
Atypical ___ hyperplasia. ___ filled with proliferating cells

Lobular
Most common benign tumor of the breast. Multiple and bilateral. Estrogen-dependent. In young women usually presents as a palpable mass. In order women, usually presents with radiodensity and calcifications.
Sharply demarcated, mobile lump that is hard to grab or palpate
Well encapsulated tumor with fibrous and ductal elements
The proliferating lobular connective tissue - loose, myxoid stroma - often compresses ductal tissue
Grossly: rubbery, white, well-circumscribed mass

Fibroadenoma
Intralobular breast tumor that usually occurs after age 40 due to acquired chromosomal changes. Overexpression of the homeobox transcription factor HOXB13 is associated with more aggressive behavior.
Large, hypercellular, with mitoses and may become malignant

Phyllodes tumor
Chromosomal change associated with malignant phyllodes tumor
HOXB13
Tumor type?
Ducts are distended with malignant cells that have hyperchrommatic and prominent nuclei. Myoepithelial cells may be seen in the involved ducts. Comedo pattern: high grade, dentral duct cells become necrotic and calcify, which are linear and branching. Non-comedo pattern: solid, cribiform, papillary and micro papillary. Basement membrane remains intact.

Ductal carcinoma in situ
Papillary and micropapillary, solid cribriform tumor within breast ducts.

Non-comedo DCIS
Underlying tumor cells extend upward to involve the epidermis of the nipple. Nipple becomes red and crusted. Micro, tumor cells occur singly or in small groups in the epidermis, have pale cytoplasm ,and satin positive for mucin (red).

Paget disease
Stain for Paget disease

Mucin
Terminal duct and lobular units are packed with abnormal cells with round hyperchromatic nuclei. Basement membrane remains intact. Increased tendency for multicentricity and bilaterality. No microcalcifications. mt in E-cadherin (-).

lobular carcinoma in situ
Most common quadrant for breast cancer
Upper axillary quadrant
BRCA 2 is associated with which chromosome?
Ch 13
BRCA 1 is associated with which chromosome?
CH 17
What grade of breast carcinoma?
BRCA-2
Ki-67
ER+
Her2+/-
Luminal, mucinous, most common
Low grade
What grade of breast carcinoma?
p53
ER+/-
Her2+
Young patients, typically minorites
High grade
What grade of breast carcinoma?
BRCA-1
ER-
Her2-
Basal-like
Generally young patients, minorities
Medullary and metoplastic
Most common type of invasive carcinoma. “Irregular hard mas of malignant cells in cords, tubules, and solid sheets. Dense, reactive fibrous (“desmoplastic”) stroma, may be scirrhous/hard.

Infiltrating ductal carcinoma
Multicentric and bilateral breast cancer that does not form a distinct mass and rarely calcifies. “Single file” stromal infiltrate. Also see signet-ring cells with mucin. Alveolar and solid variants consist of clusters of tumor cells. Usually loss of CDH1, the gene that encodes E-cadherin.

Infiltrating lobular carcinoma
Breast cancer occuring in older women.
Groups or nests of tumor cells float in pools of mucin. The borders are pushing or circumscribed.

Mucinous (colloid) carcinoma
Well-differentiated breast carcinoma consists of well-formed tubules, lacking myoepithelial cells.

Tubular carcinoma
Well circumscribed soft, fleshy tumors with pleomorphic, hyperchromatic, large cancer cells. Tumor is surrounded peripherally by a dense lymphoid infiltrate. May be BRCA1 associated.

Medullary carcinoma
Breast cancer containing both glandular and nonglandular components. Can be epithelial or mixed type. Typically aggressive.

Metaplastic breast carcinoma
The least frequent but most severe form of epithelial breast cancer that can arise as a complication of any other type. Presents with clinical signs of inflammation.

Inflammatory breast cancer
___ mastectomy: removal of breast tissue + axillary LN + part of pectoral m
Radical
___ ___ mastectomy: removal of breast tissue + axillary LN. Pectoral muscle not removed
Modified radical
___ mastectomy: removal of breast tissue only
Simple
_____: removal of tumor only, breast tissue remains intact
Lumpectomy
____ implants are inserted over both the pectoralis minor and the pectoralis major muscles.
Subglandular
____ implants are fully inserted under the pectoralis major and over the pectoralis minor muscle.
Submuscular
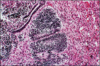
dx?

Complicated breast implant with fibrous capsule formation
Hyperplasia of ductal epithelium in a male patient. No lobules are formed. Can be due to liver cirrhosis, low androgens, hormonal imbalance, drugs, or genetic syndromes such as Klinefelters.

Gynecomastia


